Introduction
Hello, everyone! If you are brand new to working in a skilled nursing facility or if you have had 15 plus years of working in a different setting, but maybe are looking to switch to PRN or transition to the SNF setting, today's presentation will give you a very high-level overview of therapy within the SNFs.
Skilled
- Medicare A Beneficiary
- Up to 100 days of benefit per spell of illness
- Days 1-20: full coverage (2020= $0/day)
- Days 21-100: co-insurance (2020= $176/day)
Let's start with the question, "What does it mean to be skilled?" This is a term used to describe when a beneficiary of Medicare Part A uses their benefit post-hospital care. The Medicare beneficiary is entitled to up to 100 days during each spell of illness. This spell of illness begins the first day that the patient receives Medicare-covered care and ends when the patient has spent 60 consecutive days outside of the facility, or if they remain in the facility, they are not using any of the Medicare-covered care for 60 consecutive days.
There are many points of criteria that we are going to go through over the next few slides, but what I would like you to know is that if a beneficiary meets those criteria requirements, then they are entitled to full coverage for the first 20 days at 100% paid. Then, on Day 21, the beneficiary is required to pay co-insurance. This is why you may hear that one of your patients is trying to get out of the facility by day 21. This is probably because they just do not want to pay that co-insurance. As of 2020, that rate per day is $176 for co-insurance.
Skilled Criteria
- 3 midnights as an ‘inpatient’
- not ‘observation’
- A physician certifies that the patient needs SNF care
- Requires ‘skilled’ care by:
Skilled Nursing: registered nurses: 7 days per week And/Or
- Skilled Rehabilitation: physical, occupational, or speech therapists: 5 days a week
What makes the person skilled? First, they have to have spent three midnights as an inpatient in the hospital. The patient has been hospitalized and admitted as an inpatient that includes at least three midnights. Thus, we might also hear the phrase, "Did they get their midnights or did they have their three nights stay?" That is what that means. The patient has to be admitted into an acute care hospital for at least three midnights to kick in that benefit. The key here is also that admission. Sometimes a patient is in acute care, but they are not admitted but rather they are in observation. So, it is important for us to know if that person was actually admitted or just observed. If they were just an observation, then the benefit for skilled care does not kick in.
The next criterium is that the physician must sign off that this patient requires skilled nursing facility (SNF) care. I will use that term interchangeably throughout the presentation.
Finally, they are required to have the needs for skilled care. Skilled care is defined by either requiring seven days a week of nursing care and/or five days a week of skilled rehabilitation (PT, OT, or speech). We are going to get into the details of that throughout the presentation.
- Per Centers for Medicare & Medicaid Services – CMS
- Services must be rendered for a condition for which the patient received inpatient hospital services or a condition that arose while receiving care in an SNF for a condition for which the resident received inpatient hospital services.
- The daily skilled services can be provided only on an inpatient basis in a skilled nursing facility (SNF).
- Services delivered are reasonable and necessary for the treatment of the resident’s illness or injury.
Here are some quotes here from our Centers for Medicare and Medicaid Services, CMS. This is saying that the patient had to be admitted into the hospital for a condition that now needs to continue to be treated at the SNF level of care. They also expect that the SNF is a level of care that is both economical and efficient for this patient and that they require the daily services that can only be provided at the skilled nursing facility level. And finally, these services that are delivered must be reasonable and necessary for the treatment of the resident's illness or injury. Let's say that someone is admitted for our care, but they are very high functioning at almost a modified independent or supervised level for their ADL. We might deem that the patient only needs an eval or maybe they would only need a couple of days to establish a home program and then be discharged. We need to make sure our services are reasonable and necessary.
Skilled Nursing/Skilled Rehab
- Per Centers for Medicare & Medicaid Services - CMS
- In order to be deemed skilled, the service must be so inherently complex that it can be safely and effectively performed only by, or under the supervision of, professional or technical personnel.
What does it mean to be skilled for nursing versus skilled for rehab? A patient can be skilled just for nursing, a patient can be skilled just for therapy, or they can be skilled for both. It is important to be aware of whether it is the nursing care that is "skilling" them or the rehab. Our services must be so inherently complex that it can only be safely and effectively performed by or under the supervision of professional or technical personnel.
Skilled Rehabilitation
- √ RESOURCE: Medicare Benefit Policy Manual
- https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Internet-Only-Manuals-IOMs-Items/CMS012673
- Chapter 8- Coverage of Extended Care (SNF) Services
- Section 30.2- Skilled Nursing and Skilled Rehabilitation Services
- Daily (5x/week) Therapy
- Define day = 15 minutes minimum
- Inherently complex
- Requires the sophisticated skills of the therapist
- Daily (5x/week) Therapy
Again, in order to be skilled, they have to require our sophisticated skillset. All of these requirements and guidelines are in the Medicare benefit policy manual. I have made a little checkmark by that manual as a resource for you. In case you are looking for something extra to read, you can review these manuals. I want to focus on the requirements for skilled care, therapy, and rehab, and I will use those terms interchangeably today.
The first thing is that it is a requirement for at least one discipline to be in for five days a week to be skilled for rehab. In order for us to count as a day, we have to provide at least 15 minutes of one discipline and one discipline has to treat for at least five days in that week. Sometimes there is confusion around how Medicare defines the date of the evaluation as Day One. The following six days from that evaluation date would be week one. So, for example, if I complete the OT evaluation on Tuesday, we actually have until the following Monday to complete those five treatments. The confusion revolves around thinking that a week is a Sunday through Saturday, but that is not the case. The week is actually defined by the evaluation.
Some people have asked me about the requirement if a person is sick. It is important to remember that for the patient to maintain their skill level of care, they have to receive five days in that seven-day period. So if they are missing a day because they are out of the facility or they are sick, it is really important that we try to get in those five days for them. And if it does not happen, then you need to make sure that your documentation supports the reason why that person did not have therapy.
In order to be considered skilled, the rehab must be inherently complex. This means is that our skillset is required in order for the activities to be performed safely and effectively, and also that they need to be done under our supervision. We need to show that we are different from a nurse's aid or a therapy aid. We are licensed individuals and we have gone through a lot of work to get to that level so we need to use those specific skills.
And the last bullet, to be skilled, they need the sophisticated skills of a therapist. I say this all the time. This is a Medicare word that is out of the manual. We need to state these skills and weave this into our daily treatments. Some people think that it is the diagnosis that keeps somebody under skilled care, but it is whether or not they need the skill set of the therapist.
There are a lot of different insurances out there, but so far, I have only been talking about Medicare Part A. Let's now take a look at other insurance plans.
Medicare Vs. Managed Care
- Managed Care
- Medicare Part C: Medicare Advantage Plans or “MAs"
- Offered by private companies approved by Medicare
- Provides all Part A benefits for Hospital and SNF coverage
- Private companies must follow Medicare rules however can charge differently
- HMO / PPO / POS Plans
- Health Maintenance Organizations (HMO) usually only pay for care within the network. You choose a primary care doctor who coordinates most of your care.
- Preferred Provider Organizations (PPO) usually pay more if you get care within the network. They still pay part of the cost if you go outside the network.
- Point of Service (POS) plans let you choose between an HMO or a PPO each time you need care.
Managed Care is growing rapidly across the United States. First, Medicare Part C is comprised of the Medicare Advantage Plans, also known as MA's. If you are eligible for Part A, meaning that you are over 65, you are also eligible to choose a Medicare Advantage Plan. The Medicare Advantage Plans are more on the commercial side, but they follow Medicare guidelines. The only difference is that they are run by private companies. They follow the Medicare guidelines or rules, but they can charge differently. So, you might see that somebody comes in under a Medicare Advantage Plan or a commercial insurance plan. Commercial plans are the HMOs, your PPOs, your POS plans. Typically, these are the patients who are under 65. We need to understand is the coverage requirements no matter what insurance. For example, you might have someone who is in your facility with a commercial insurance plan that might only cover 60 minutes a day of all disciplines. If you have all three treating a client, you are going to have to make some decisions. Each contract and state is different, but it is important to know the rules for your situation.
Case Study
- Mrs. Davis
- Assisted Living resident, required set up for most ADL
- 3 nights admitted as an inpatient
- Physician documented conditions required SNF care
- The physician recommends SNF for the next level of care
- Goals set for near PLOF – at a level that AL can support
- Discharge planning starts at the time of admission
Mrs. Davis is an 82-year-old who lives in an assisted living prior to the onset of this recent condition. She was quite independent and only required setup or supervision for her ADLs. She was sent to the hospital due to a change in mental status and an increased need for care and support. She was admitted to the hospital and spent three nights there where she was diagnosed with a UTI and sepsis. They were able to stabilize her, but due to the level of the deconditioning, the physician recommended SNF care, including therapy. Upon admission to the SNF, she had all three disciplines screen her, and both PT and OT established a plan of care with goals for her to return to that prior level of function. The OT goals were for her to be modified independent with her eating and grooming post set up, dressing and toilet and goals were set to supervision, and bathing was set to contact guard assist, knowing that the patient could be returned to her assisted living requiring some assist. (As a reminder, remember goals should be written for that next level of care.) In this example, we are writing our goals for that assisted living discharge and the lowest level of care they could handle as insurance plans are expecting us to be efficient and economic with our decision making. Thus, when we initiate that care, it is our responsibility to learn exactly what the level of assistance the patient has available for discharge planning, and this should begin from the date of the evaluation.
PDPM
- Patient-Driven Payment Model – PDPM
- Old system: Resource Utilization Groups (RUG)
- $ based on therapy minutes
- New system: As of October 1, 2019: PDPM
- $ patient classification
- 5 payment groups
- Old system: Resource Utilization Groups (RUG)
As of October 1st, 2019, the Patient-Driven Payment Model (PDPM) replaced the former RUG system. If you have not been in a skilled nursing facility for some time, this is a big change from the previous system for payment. The RUG system primarily relied on our therapy minutes to reimburse for payment and be skilled in a nursing home. This new payment model classifies patients into different groups based on mostly diagnosis characteristics to determine their rate.
PDPM Case Mix Groups
In Figure 1, you can see there are six case-mix groups, five of which are clinical.
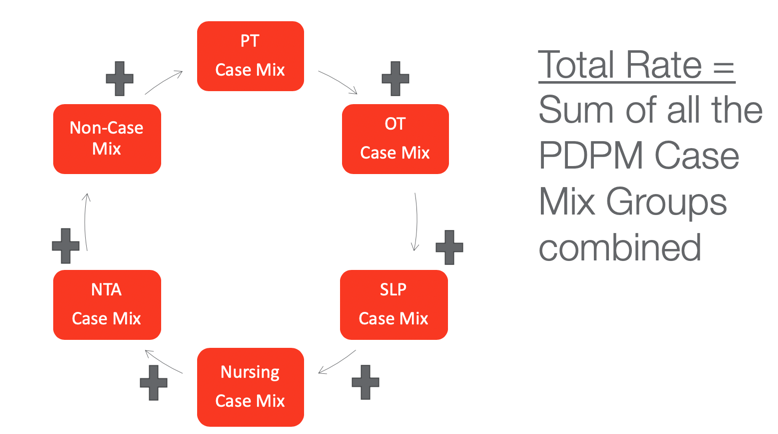
Figure 1. Six case-mix groups.
The groups are PT, OT, speech, nursing, the nontherapy ancillary (NTA), and a non-case mix group. This non-case mixed group is based on location, whether you are rural or urban, and what state you are in. When a patient is admitted to the facility, they are classified into these groups, and each group has a different associated rate. We add up all of those rates and that is what gives us the total rate per day for a patient to be in a skilled nursing facility.
Minimum Data Set
- Minimum Data Set (MDS)
- Detailed assessment
- Interdisciplinary
- Must be completed within 8 days of admission
- Must be completed at discharge
- Required by CMS (Centers for Medicare & Medicaid Services)
- Instructions are in the RAI Manual (Resident Assessment Instrument)
- √ RESOURCE: Resident Assessment Instrument
The information that we are gathering for those diagnoses and groups all come from what is called the minimum data set or the MDS. This is an assessment that is completed for every Medicare skilled patient and any insurance that is following the Medicare guidelines. It is a very detailed and long assessment that is required by CMS and the rules for coding this assessment are contained within a manual that is 1,300 pages long. We are definitely not getting into the details of that today, but I am going to do some reviewing because I do think it is important for us therapists to understand how we are contributing to the MDS, which then contributes to payment for PDPM. The MDS has to be completed within eight days of admission. It is completed again at the time of discharge. The latest version of the RAI manual was released in October of 2019 when PDPM was released. If you want to check it out, I have provided the link for you.
PDPM: Therapy
- Section GG MDS: Functional Abilities and Goals
- Prior Function
- Admission Performance
- Discharge Goals
- Discharge Performance
*Most OTs are asked to contribute to this section for payment under PDPM
The skilled nursing facilities rely on OT and PT to contribute to section GG, which is the functional abilities and goals section. There is a lot of data that comes into the MDS, but specifically for section GG, they are looking at the patient's functional abilities and their goals. It includes the items that focus on prior function, how they are doing at admission, what their goals are going to be for discharge, and their discharge performance. The functional status is assessed for the need of assistance for both self-care and mobility, and this is why we see mostly OTs and PTs contributing to this.
The person who is responsible for submitting and completing this MDS assessment is the MDS nurse. She is the one who gathers and collects the data that is needed for all of the areas. Mostly PT and OTs are responsible for gathering the information and then giving it to the MDS nurse, or she can collect that off of our evals. This is why it is important for us to understand the rules behind this section so that we gather the correct information. In fact, a lot of the therapy software is now embedding this information right into our evals.
Section GG: Decision Tree
This decision tree is from the RAI Manual (Figure 2).
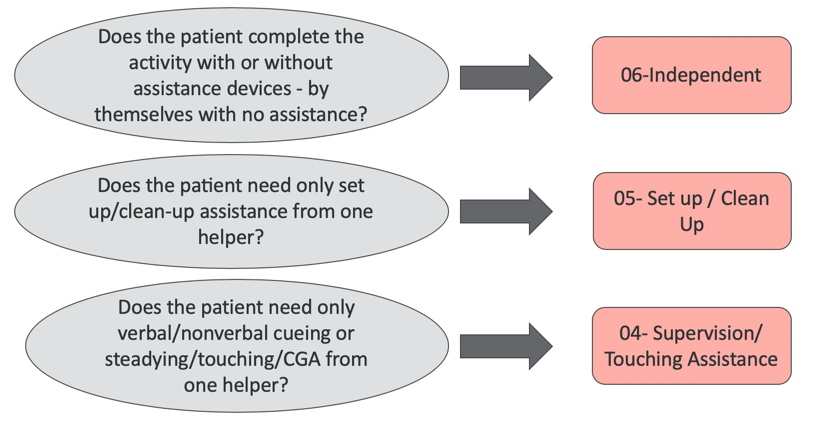
Figure 2. Section GG Decision Tree.
This is an easy way for us to code our residents in section GG. Obviously, we were trained as therapists through the physical rehabilitation model of using min, mod, max, and modified independent, as well as, contact guard. You should all be familiar with those words. What I want to point out is that the wording here is actually quite different. In the first area, does the patient complete the activity with or without assistive devices by themselves with no assistance? If you can answer yes to that, you would score them as 06-independent. If you would say no, then you move down here to the next question. Does the patient need only set up or clean up assistance from one helper? If you can answer yes, you code them as a 05-set up/clean up. If you answer no, you move to the last area. Does the patient need only verbal, nonverbal cueing, or steadying, touching, or contact guard assist from one helper? If the answer is yes, we code them as a 04-supervision/touching assistance.
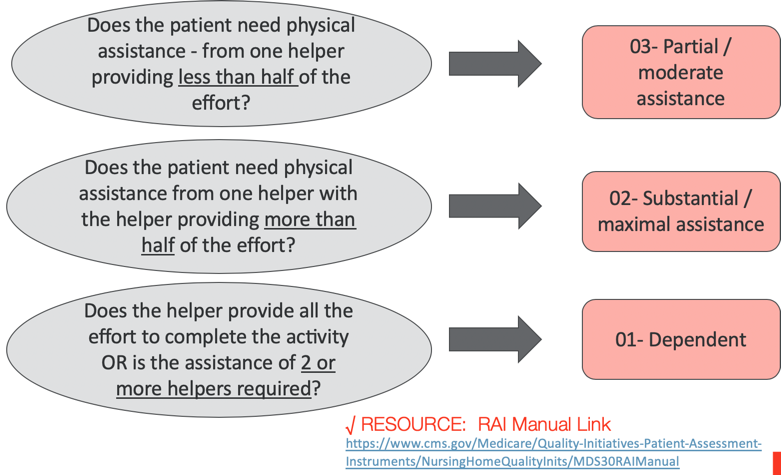
Figure 3. Section GG Decision Tree- Part 2.
If it is no, then we move down to the next question. Does the patient need physical assistance from one helper providing less than half of the effort? That is key. If the answer is yes, we code them as a 03, or partial moderate assistance. If we can say no, the next question is, does the patient need physical assistance from one helper with the help of providing more than half of the effort? If the answer is yes, we code them as a 02-substantial/maximal assistance. If the answer is still no, then we come down to the final area. Does the helper provide all of the effort to complete the activity or is the assistance of two or more helpers required? If at any point they require the assistance of two or more helpers, then they are coded as a 01-dependent. I put in another resource checkmark at the bottom.
Steps for Assessment
- Activities may be completed with or without assistive device(s)
- Assessment should be conducted prior to the resident benefitting from treatment interventions in order to truly reflect the patient’s baseline
- Do not record the patient’s best performance
- Do not record the patient’s worst performance
- Record the patient’s usual performance
I also pulled out some of the steps of this assessment. Activities can be completed with or without assistive devices and should not affect the coding of the activity. Also, we should be assessing the patient for this coding prior to giving them our interventions. As therapists, we like to give cues and implement compensatory strategies via words or hands to help the patient. We should let the patient perform the activity without our help first so that we can record their usual performance. This is an assessment that needs to be completed within that first three days.
- Assess self-care performance based on direct observation
- The patient should be allowed to perform the activity as independently as possible, as long as they are safe
- A “helper” is defined as facility staff
- helper assistance is required because of a resident’s performance is unsafe or of poor quality
Continuing on, we want to assess their self-care based upon our direct observation. What did we see? We need to allow the patient to be as independent as possible, as long as they are safe.
Finally, a helper is defined as facility staff. Helper assistance may be required because a resident's performance is unsafe or of poor quality without it.
Define Helper
- Per the RAI Manual, a helper is defined as facility staff. This includes:
- Rehab Staff (including contract therapy staff)
- Nursing Staff (including agency staff)
- This does not include:
- Hired individuals
- Hospice staff
- Students
Again, these definitions come from the RAI Manual. A helper is defined as facility staff and that would include rehab staff, nursing staff, agency staff, and contracted staff, as long as they are rehab or nursing. It does not include privately hired individuals, hospice staff, or students. Gathering this information for the assessment is supposed to be via an interdisciplinary approach. It is supposed to be both nursing and therapy gathering information about the patient within the first three days. Again, the MDS nurse is then responsible for coding it. I know this process probably varies from facility to facility as far as who exactly is the driver, but I do know that a lot of evaluating therapists are being asked to contribute to this.
Language Translation
- Therapy and Nursing have different languages about coding assistance
- It is very important for the therapists to understand the nursing language to code Section GG
- The RAI Manual is the guide for coding Section GG, not as described in our textbooks, ie: Physical Rehabilitation
√ RESOURCE: RAI Manual Link
When it comes to coding levels of assist, nursing and therapy speak different languages. If you are going to be working in a skilled nursing facility, it is important that you understand the rules behind coding this section. As an example, you might have noticed that in the example I gave earlier six is independent, but where is modified independent? That was not in the decision tree. This is because a modified independent level falls under an independent level because an assistive device can be used here.
Other Areas of MDS
- Section C: “BIMS” Brief Interview for Mental Status
- Cognition screen
- Section D: “PHQ9” Resident Mood Interview
- Mood interview
- Section F: Daily Preferences
- Daily preferences and activity preferences interview
- Section G: Functional Status
- Another section that looks at ADL performance, normally done by nursing
- Section J: Pain
- Pain interview
There are quite a few other areas of the MDS that I am seeing therapists being asked to contribute to. Section C has the BIMS, which is a Brief Interview for Mental Status. This is an interview with very specific instructions to help to assess their cognition. So, if you are being asked to contribute to section C, I would make sure you have the instructions from the RAI Manual on how to perform the BIMS. Section D is the PHQ9, and this is a resident mood interview. It also has very detailed rules and guidelines. Some OTs are being asked to perform this as well. Again, you want to make sure you get those guidelines. Section F looks at daily preferences. Section G looks at functional status. This is not to be confused with section GG, but this is another area. Most of the time, it is nurses that gather this information on their ADL performance. Section J is a pain interview. We can also contribute to this area as long as we follow the guidelines.
- Section K
- Swallowing/Nutritional status
- Therapeutic diets
- Parenteral/IV Feeding
- Feeding Tube
- Mechanically altered Diet
- Speech Therapy Assessments help
- OT likely could contribute to this area too
Section K is quite an impactful area right now under PDPM, and a lot of speech therapists are being asked to contribute to this area. However, there is some overlap in our OT scope of practice here. I would not be surprised if you are asked to pick up some information in this area.
- Section 0: Special Treatments, Procedures, and Programs
- Collects PT, OT and ST minutes and days
- Individual minutes
- Concurrent minutes
- Group minutes
- Co-Treatment minutes
- Total days of therapy administered
- Therapy start and end date
Finally, Section O is mostly data analytics. Most of the time this is information that is coming directly out of our therapy software, and you do not really have to do anything with it. I just wanted to point it out because CMS looks at this information.
Overall, Section GG is definitely the area where OTs are contributing the most to the MDS. As I just mentioned, there are a lot of areas where we could be asked to contribute. My advice to you is that if you are being asked to contribute to these other areas, make sure you have gotten the training or are asking your therapy manager or your corporate resource person for more information. You are also welcome to reach out to me.
Long Term Care Therapy
- Medicare Part B
- 80% coverage for Therapy Services
- Managed Care Part B
- Varies - may only approve a certain number of therapy visits
- Medicaid
- No therapy coverage
Another area that you are definitely going to have to get used to when working in a nursing home is treating the long term care patients. These are the patients who reside in the nursing home who are no longer under that skilled Medicare benefit. They may be pay privately or use a longterm care insurance plan. There are different benefits for their therapy needs.
Medicare Part B is very common in the nursing home for the longterm care side of OT services. What I think is important for you to know is that all three disciplines, PT, OT, and speech, are only covered for only 80%. The remaining 20% might need to be paid out of pocket for your residents. Secondary insurance might pick up some of that other portion or maybe even all of it. Facilities typically have some sort of internal policy of how we go about making sure that there is payment for that other 20%. If you are new to the SNF industry, I would add this to your list of questions. Find out what the company policy or specific procedure is for when someone has Part B therapy services. Do we need to contact the family or can the patient sign off on it and give it the okay that they are going to pay that remaining 20%?
There is also Managed Care B that has a huge variety of coverage options. If a patient has a Managed Care Part B, like those commercial insurances like Aetna or Humana, whether they are a replacement plan or commercial insurance, we typically have to provide them our evaluations. They then tell us what they will approve. I have seen as little as four visits being authorized, and if you are lucky, you might get 10 visits. Another question for your facility manager is what is the process? Who is responsible for finding out what is covered? Who is responsible for submitting that evaluation to the insurance company? And if we do not hear back, who is responsible for following up? Most of the time that falls to the facility or somebody at the facility, perhaps the business office manager. You need to know how to ask for coverage and who is responsible as well as what is the process for treatment. Do you have to wait to treat the patient until you have heard it has been approved? Or, are you okay to start treating and have your fingers crossed that the insurance company approves your plan of care?
Another payer that is very common is Medicaid. When a patient is living inside a nursing home, their services for therapy are not covered through Medicaid. This is going to be an expense to the facility and that is something important for us to know as the facility might have a specific process in place. The facility administrator may approve how many visits that we can provide to them.
Regardless of the payer, it is important to be efficient and effective with our treatment plans and documentation so support our skilled service.
Documentation
- Part A vs Part B
- Part B: Requires a therapist visit every 10 sessions or every 30 day whichever comes first
- The therapist must treat the patient for at least 15 minutes
- The therapist must write a progress note summary, update goals as needed and adjust the plan of care as needed
- Review skilled interventions
- Review COTA notes / collaborate with COTA
- Part B: Requires a therapist visit every 10 sessions or every 30 day whichever comes first
*Know your employer’s expectations for documentation
There are different requirements for the skilled population than there are for the Part B population. specifically, Medicare Part B. One requirement is that you need to document every 10 sessions or every 30 days, whichever comes first. In order to meet the guidelines, you also must treat the patient for at least 15 minutes, but I recommend longer. I suggest doing a progress note with them, updating their goals and plan of care, and reviewing the skilled interventions that you have written in your order. If you are collaborating with a COTA, how is it going? How is the treatment? Are they progressing? Do you need to make any changes to that plan? Make sure that when you write this note, you are covering that span of the last 10 sessions or 30 days. As a side note, this is a requirement for Part B, but I am seeing in many facilities that they use this for other payers. While I am only presenting the Medicare requirements, you might find that your facility has stricter guidelines. You need to determine what their documentation expectations are. We will be diving deep into documentation on Part Two of our series on skilled nursing facilities.
Areas of treatment
- Decline in ADL
- Splinting / contracture management
- Wheelchair seating/management
- Referring to restorative
For longterm care, most referrals are for the above-bulleted areas. They may show a decline in dressing or feeding themselves. We might see them for splinting or contracture management. You may need to check with your facility whether they prefer prefabbed or custom splints. Do you have the equipment to make the splints? Regardless, you are going to be setting up splint schedules with either option. Another very common area is wheelchair seating and positioning. You want to find out what your facility typically does and what vendors they work with. In long term care, you will need to know how to do a seating eval. If you are not familiar with this area, then I would recommend you seek out another CEU on wheelchair seating and positioning, and OT.com has some great resources for this. Finally, restorative is another area that is very facility-specific. A restorative program is a great way to carry out our plan of care to the next level of care. Common restorative programs include the walk to dine, feeding, toileting, and range of motion programs. Thus, I would ask your facility, what is your restorative programs, and what is the process to refer someone to restorative.
Case Study
- Mr. Smith
- PLOF (Prior level of function):
- Mod I / set up: feeding; grooming
- Mod I / set up: Dressing and Bathing Upper Body
- Dep: Dressing and Bathing Lower Body, Toileting
- Min - Mod: transfers
- OT: Plan of care
- Goals
- Treatment approaches
- Recommendations for D/C
- PLOF (Prior level of function):
Let's take a moment and do another case study. Mr. Smith is a longterm care resident. He resides at the Silver Springs Nursing Home, and he has a history of COPD and end-stage renal disease. He is able to perform his eating and grooming with modified independence post setup. Prior to the onset of this recent change of condition, he was able to dress and wash his upper body at a wheelchair level but was dependent for lower body care and toileting. He also required assistance for transfers and the amount of assistance (min to mod) depended upon his dialysis schedule. He has had a change of status noticed by the nursing staff with a decline in his ability to dress and wash his upper body. He also requires more assistance with transfers. The nurse has documented that his strength appears to have also declined. An order for OT was placed by the physician in hopes to return him to his baseline.
As the occupational therapist, we would want to establish a plan of care that is meaningful for Mr. Smith, and one that takes into consideration his prior level of function. Due to the fact that he lives in a nursing home, he can be provided with around the clock care and has a history of being dependent for certain areas of care. We want to make sure that our plan of care focuses on the areas that have had a recent decline. Thus, we would write goals to improve the upper body dressing and bathing. We could also have him work on transfers and overall upper body strengthening to complete these activities. However, your frequency and duration for longterm care patients cannot be at a skilled level, and typically, therapy is less than five times a week. An example might be two to three times a week for four weeks. Examples of treatment interventions would be ADL training, therapeutic exercise, and therapeutic activity. Our focus would be on getting him back to his prior level of function.
A Therapist's View of Compliance
- Medicare Benefit Policy Manual: Chapter 8, Section 30.2
- Medicare Benefit Policy Manual: Chapter 15, Section 222.0
√ RESOURCE: Medicare Benefit Policy Manual
We are now going to talk a little bit about compliance and how skilled nursing facilities are monitored and surveyed by government entities. The Medicare benefit policy manual is a 16-chapter manual with detailed instructions of these guidelines, rules, and directives. Chapters 8 and 15 have a lot of details about therapy. We are going to dive right into some of those expectations. But first, I want to just mention to you where you can get some resources on billing practices because we are not going to get into that too much today.
- Billing Practices
- Local Coverage Determinations (LCD)
- National Coverage Determinations
- Documentation
- The documentation must support the medical necessity
- SNF Primer 2 will cover this in detail
√ RESOURCE: Local Coverage Determinations
https://www.cms.gov/Medicare/Coverage/DeterminationProcess/LCDs
If you are looking for a resource, the local coverage determination can be found at cms.gov. This breaks down the requirements for each CPT code that is billed. You can also ask your facility manager for resources on CPT codes and billing practices. As I said, we are going more into documentation in our second presentation.
Reasonable and Necessary
- Services are not considered skilled just because a therapist/assistant provided.
- If a non-skilled person or a patient can safely and effectively administer a task, it is not skilled.
- The unavailability of a competent person to provide non-skilled services does not make it skilled when a therapist performs the task.
- General activities for the good of patients (to promote fitness, flexibility, motivation) are not skilled.
- Services provided that are not under a plan of care, are not payable.
- Services provided by staff who are not qualified (or supervised) are not payable.
√ RESOURCE: Medicare Benefit Policy Manual
30.2 - Skilled Nursing and Skilled Rehabilitation Services
What does it mean to be reasonable and necessary? We need to make sure that our documentation supports all of the aforementioned areas because this is what is required through that Medicare benefit policy manual. It is a reoccurring theme. Things have to be medically necessary, reasonable, and documented. Services are not considered skilled just because we provided them. What did we do that made it therapeutic? Did we grade the activity? Did we offer compensatory strategies? Those are the things you should be documenting. If a non-skilled person or patient can safely and effectively administer a task, it is not skilled. If we can pass the task to a therapy aid or a nurse's aid, or the patient can do it themselves, at this point, our services are no longer needed and therefore are no longer considered skilled. Three, the unavailability of a competent person to provide non-skilled services does not make it skilled when a therapist performs the tasks. I have seen this come into play when the patient is ready for discharge from therapy, but there is nowhere to discharge them. For example there may not be a restorative program. This is not a legitimate reason to continue to treat them under our services. General activities for the good of patients to promote fitness, flexibility, and motivation are also not considered skilled. I think this is pretty self-explanatory. Those are all good things, but they are not considered skilled. Services provided that are not under a plan of care are not payable, That is also very black and white. And finally, services provided by staff who are not qualified or not supervised are not payable.
- Necessary to:
- improve a patient’s current condition
- maintain a patient’s current condition
- slow further deterioration of the patient’s condition
Overall, necessary means that our services are improving a patient's current condition. Necessary means that we are maintaining a patient's current condition. It also means that we are slowing the further deterioration of the patient's condition. These are things to keep in mind when you are treating a patient. You need to either be improving, maintaining, or slowing that further deterioration for this activity to be necessary.
Case Study
- Mr. Johnson: PLOF
- Mod Assist Dressing, Bathing, Toileting
- Mod I: Feeding and Grooming
- Mod I: W/C Mobility
- Mod Assist: Functional Transfers
- Mr. Johnson: Evaluation Status
- Max A: Dressing, Toileting
- Dep: Bathing
- Min A: Feeding and Grooming
- Dep: W/C Mobility
- Max A: Functional Transfers
Mr. Johnson was referred to therapy due to a recent hospitalization. Prior to this, he lived in a longterm care facility requiring mod assist for dressing, bathing, grooming, and toileting. He would typically wheel himself to the dining room, and he could feed himself after setup. He was modified independent with grooming and a moderate assist for transfers. The OT eval was completed and goals were established to return him to his baseline. At the time of evaluation, he required max assistance for dressing and toileting and was dependent for bathing. He was unable to propel his wheelchair and was min assist now for feeding and grooming. Transfers were a max assist. He made great progress in the two weeks, and he really enjoyed his therapist and socializing in the therapy department and made good friends. In his 10th visit note with his occupational therapist, he was able to return demonstration of his home exercise program, and he returned to his prior level of function. The OT told him that his goals were met. He became very upset saying he loved therapy and did not want therapy to end. As there was no restorative program due to staffing, he begged her to keep him on therapy and said he would work extra hard to prove that it was needed. What does an OT do in this situation?
- Review the skilled criteria:
- Requires the sophisticated skills of a therapist
- Measurable, functional improvement toward PLOF
- Inherently complex services
- Plan of care under a physician
Remember, he was longer meeting skilled criteria, and he had resumed his prior level of function. The appropriate action is to discontinue therapy and let the nurse know that he should be encouraged to complete his home program and recommend that they incorporate that into their daily care plan.
Expectations of Therapy
- Address recovery, improvement in function, restoration of prior level of function
- Documentation is key
- Objective measurements
- Justify continued treatment
- Continued assessment and analysis
- Instruction for compensation
- Training to family and patient
The expectations of us under CMS are that we address recovery, improvement in function, and help restore their prior level of function. Our documentation must reflect that we are providing services that are reasonable and necessary, and we should provide objective measurements that show improvements in function. We must clarify that our treatments are justified to make impactful changes in their functional improvements and everything correlates to function. We have to provide ongoing education and instruction for implementing compensatory skills, and we should be training the patient, the family, and caregivers to augment the rehabilitation process. We need to make sure that we are documenting those treatment sessions with instructions and making sure that we progress those areas as well. As somebody progresses, we need to train the family on the next step. As you can see, our documentation is so important.
Billable Services
- Occupational Therapy Evaluation Codes
- 97165 Occupational therapy evaluation, low complexity
- A brief history including a review of medical and/or therapy records
- An assessment(s) that identifies 1-3 performance deficits
- Clinical decision making of low complexity
- Typically, 30 minutes are spent face-to-face with the patient and/or family
- CPT = Current Procedural Terminology
- 97165 Occupational therapy evaluation, low complexity
I want to now go over some CPT codes and billing practices. Back in 2017, they updated the evaluation codes for three different levels. The first one is 97165, which is a low complexity. It is a brief medical history review. You find only one to three performance deficits, and your decision making is of low complexity and according to the CPT code. This should take about 30 minutes to do this evaluation.
- OT codes continued
- 97166 Occupational therapy evaluation, moderate complexity
- An expanded review of medical and/or therapy records
- Identifies 3-5 performance deficits
- Clinical decision making of moderate analytic complexity
- Typically, 45 minutes are spent face-to-face with the patient and/or family
97166 is occupational therapy eval, moderate complexity. It takes it one step further with a more expanded chart review, identifying three to five performance deficits of the patient. You are making moderate analytic complex decisions for this patient, and typically, it takes about 45 minutes.
- 97167 Occupational therapy evaluation, high complexity
- Includes review of medical and/or therapy records extensive additional review of physical, cognitive, or psychosocial history
- An assessment(s) that identifies 5 or more performance deficits
- Clinical decision making of high analytic complexity,
- Typically, 60 minutes are spent face-to-face with the patient and/or family
The last one is high complexity, 97167. This includes an extensive review of the chart. It identifies five or more performance deficits. Your decision making is of high analytic complexity and according to the CPT code, we are spending at least 60 minutes or so with our patients.
- Common OT CPT Codes for SNF
- 97535 - Self-Care
- 97112 - Neuromuscular re-education
- 97110 - Therapeutic exercises
- 97530 - Therapeutic activities
- 97129 - Cognitive function
- 97542 - Wheelchair management
- 97010 - Hot or cold packs
√ RESOURCE: AOTA (members only) 2020-Selected-Occupational-Therapy-CPT-Codes.pdf
https://www.aota.org/Advocacy-Policy/Federal-Reg-Affairs/Coding.aspx
These are the most common treatment codes that I see used in the skilled nursing facility. It is important that you understand the guidelines behind these CPT codes, and I have put a checkmark there for a great resource for AOTA. If you are not a member of AOTA, join in Part Two and we will take a deeper look. I do want to mention that it is important as the evaluating therapist to select the CPT codes that directly impact the plan of care. You want to write your goals and then choose the CPT codes that best support that patient's individual needs. And, if you are a COTA, you want to treat the client based on your goals. That should always your guide. If you ever see a CPT code that does not really relate to your plan of care, then I would reach out to the OTR and have a discussion with them about that.
Maintenance Therapy
- 2013 class-action lawsuit
- Jimmo versus Sebelius Case
- “Improvement Standard” inappropriately applied
- Argued Medicare coverage should be based on need, not on the potential to improve
- Allows for a maintenance program to maintain the patient’s current condition and to prevent or slow further deterioration - as long as the beneficiary requires “skilled care” for the safe and effective performance of the program
There was quite a large case back in 2013 called Jimmo vs. Sebelius. In this case, the plaintiff alleged that Medicare contractors were inappropriately applying improvement standards. This is what confirmed that Medicare coverage should be determined based on a beneficiary's need for skilled care, not necessarily their potential for improvement. What does this mean for you? If someone in your facility is in need of skilled care but probably will not make any measurable progress, we want to make sure we are following the guidelines for maintenance therapy, and we are documenting the reason why the skilled sophisticated services are required to treat this patient. It is not something you will often see, but if you do have a patient who fits this description, make sure you are following the guidelines and documenting clearly why your skillset is needed.
Non-Billable Services
- Documentation time – unless you are completing your documentation with the patient
- Family meetings - unless the patient is present, but only then can you count the time you spent providing skilled information/updates on POC
- Planning for a treatment session
- Screens
- Transporting a patient
There are also some non-billable services. When you are completing your documentation alone, it is not billable. If you complete the documentation with the patient, you can bill for that time. Family meetings are only billable when you are with the patient and during the time that you are providing a plan of care updates and educational instruction. You cannot bill for the entire time that you are in a family meeting, but you can bill for the time that you spend providing skilled information. You cannot bill for the time that you are planning a treatment session or completing a screen or chart review. Lastly, you cannot bill for your time with transporting patients to and from therapy.
Wrap Up
- Resources:
- OccupationalTherapy.com
- American Occupational Therapy Association
- OT state Organizations
- CMS.gov
- Medicare Benefit Policy Manual
- Local Coverage Determinations
- Resident Assessment Instrument
Thank you so much for your attention. I provided a list of resources that I used to prepare this talk.
Acronyms In This Presentation
- ADL: Activity of daily living
- AANAC: American Association of Nurse Assessment Coordination
- AOTA: American Occupational Therapy Association
- BIMS: Brief Interview for Mental Status
- CMS: Centers for Medicare & Medicaid Services
- COTA: certified occupational therapy assistant
- CPT: Current Procedural Terminology
- HMO: Health Maintenance Organizations
- LCD: Local Coverage Determinations
- MDS: Minimum Data Set
- OT: Occupational Therapy
- PDPM: Patient-Driven Payment Model
- PHQ9: Resident Mood Interview
- PLOF: Prior level of function
- POC: Plan of Care
- POS: Point of Service
- PPO: Preferred Provider Organizations
- PT: Physical Therapy
- RAI: Resident Assessment Instrument
- RUG: Resource Utilization Groups
- SNF: Skilled Nursing Facility
- ST: Speech Therapy
- W/C: Wheelchair
Questions and Answers
What is it meant by case-mix?
A case-mix can be a mixture of different diagnoses. Let's say someone has impairments in cognition, swallowing, and an acute neurologic impairment. All of this would fall under the speech case-mix category. This is getting a little bit deeper into PDPM than we intended for today's session.
Is there a yearly monetary cap for Part B?
They did release the cap, but there is still something that is called the threshold which automatically puts the patient into an audit through Medicare Part B. This means that we always need to make sure that we are providing the care that the patient needs. This is both efficient and economical. They are monitoring cases that provide an abundance of therapy to make sure that the documentation is there to support it. I have defended cases that have exceeded that threshold and they have been paid, but I have also defended cases that they have not been paid. Our documentation is always key.
Which I think is a great segue to encourage you to tune in to Part 2 of this series. We will talk more about that and how our documentation can support us.
References
American Association of Nurse Assessment Coordination, Copyright 2019, American Association of Post-Acute Care Nursing, d/b/a American Association of Nurse Assessment Coordination. All Rights Reserved. AANAC.org, Released Aug. 2019
Center for Medicare Advocacy; Nursing Home / Skilled Nursing Facility Care
Center for Medicare Advocacy: Medicare Cost-Sharing Rates (Premiums & Deductibles for 2019 & 2020)
Center for Medicare Advocacy:Toolkit: Medicare SNF Coverage and Jimmo v. Sebelius Toolkit https://www.medicareadvocacy.org/toolkit-medicare-skilled-nursing-coverage-and-jimmo-v-sebelius/Medicare SNF Coverage and Jimmo v. Sebelius Toolkit.pdf
CPT® Assistant February 2017 / Volume 27 Issue 2 New Occupational Therapy Evaluation Codes
CMS.Gov: Local Coverage Determinations: https://www.cms.gov/Medicare/Coverage/DeterminationProcess/LCDs
Medicare Benefit Policy Manual, Chapter 8, section 30.2 and Chapter 15, section 220: https://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/Internet-Only-Manuals-IOMs-Items/CMS012673
Resident Assessment Instrument: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/NursingHomeQualityInits/MDS30RAIManual; https://downloads.cms.gov/files/mds-3.0-rai-manual-v1.17.1_october_2019.pdf
Citation
Dwyer, K. (2020). Skilled nursing facility primer-Part 1. OccupationalTherapy.com, Article 5243. Retrieved from http://OccupationalTherapy.com
