Introduction
I am excited to share with you guys a lot of great information in our one-hour webinar today. I would suggest getting a paper and pencil or print out the handout as we will do some fun activities and talk about some good strategies today. We will go through a little bit of review at the beginning, and then we will get into the nitty-gritty of sensory approaches. If you are a new OT, this will be something that maybe is new to you. But for more seasoned therapists, the beginning will be a review.
What Is Sensory Processing Disorder?
- Sensory Processing Disorder (SPD) is a complex disorder of the brain that affects children and adults. People with SPD misinterpret everyday sensory information, such as touch, sound, and movement. They may feel bombarded by information, seek out intense sensory experiences, or be unaware of others' sensations. They may also have sensory-motor symptoms such as a weak body, clumsiness, awkwardness, or delayed motor skills.
Dr. Lucy Jane Miller 2007
This is a complex disorder of the brain that affects both children and adults. People with SPD misinterpret everyday information, such as touch, sound, movement. They may also have motor issues, auditory processing issues, visual processing issues, tactile sensitivity, and all of those things. This can impede their ability to function within their day-to-day environment. This is why we call it a sensory processing disorder.
Who Is This Applicable For?
- Autism Spectrum Disorders
- SPD (Sensory Processing Disorder)
- ADHD
- Down Syndrome
- Cerebral Palsy
- Developmental Delays
- Motor Delays
- Gifted and kids who are 2E
- Anxiety
- Typical children
Today, this talk is applicable for all kids on the autism spectrum, those with SPD, kids with ADHD, CP, motor delays, gifted or twice-exceptional (2E), anxiety, et cetera. I hope that this covers a lot of the clientele that you may have on your caseload. I work with kids in the home. I am currently doing a lot of Zoom telehealth right now due to COVID. I also work in schools. Previously, I worked in a lot of different settings. Even though this is a sensory approach to home, many of these strategies can be utilized with your clients.
8 Sensory Systems
- The 5 Senses we all learned about as a child
- Taste – oral motor
- Touch- tactile processing
- Sight – visual motor/perceptual
- Sound- auditory processing
- Smell – olfactory
What are our eight sensory systems, and how do we portray these to parents? We often give parents so much information, including home exercise programs and training. We need to talk to these parents in a straightforward way and give them the scientific background of sensory processing and how this may affect their child.
There are the five sensory systems that we learned about when we were a kid: taste, touch, sight, sound, and smell.
The 3 Hidden Senses
- Vestibular – governs balance, where your head is in space, and how fast you are moving.
- Proprioception- input to the muscles and joints that tells us where our bodies are in space
- Interoception- a sense of internal organs
Then, we have what I call our three "hidden senses." These are vestibular, proprioception, and interoception. It may be hard for parents to understand these three hidden senses. I try to use examples of what this might look like in their home.
The Vestibular System.
- The vestibular system is governed by your inner ear and tells us where our heads are in space, whether right side up or upside down.
- It tells us how fast we are moving and helps with the balance and coordination of both sides of the body.
- It influences muscle tone, posture, and coordination between eye movements and head movements.
The vestibular system is governed by the fluid in the inner ear, which tells us whether our heads are upside down, right side up, and how fast we are moving in space. It influences our muscle tone, posture, and coordination between our eye and head movements. We may see kids that have visual perceptual or tracking issues. Obviously, this can be a part of the visual system, but it is also highly correlated to the vestibular system and the inner ear. I like to ask questions like, "Did they have a lot of ear infections when they were a kid?" "Did they have any medical procedures or surgeries?" I try to get a lot of that background to make sure that I am covering my bases and identifying any red flags.
The Proprioceptive System.
- The proprioceptive system is the input to our muscles and joints during heavy work. It tells us information about movement, position, and force exerted by muscles and joints.
- Tells where your body is in space
The proprioception system is input to the muscles and joints during heavy work activities. It tells us information about movement, position, and where our body is in space. You may see a child navigate through a busy environment and bump into things, or they appear clumsy. These behaviors may result from a motor issue, or they may be due to decreased body awareness.
Interoception- 8th System.
- Internal temperature
- The feeling of hunger/fullness
- Do I have to use the bathroom?
- Am I tired?
- Does my stomach hurt?
- Check out Cara Koscinski’s latest book
Interoception is the eighth sensory system. Am I hungry? Am I full? Am I hot? Am I cold? How am I feeling about that internal sense of self? There are several different resources out there about interoception. I love Cara Koscinski's book. She is the Pocket OT. She is a friend of mine, and I love her stuff.
I also want to touch base on these three and the main sensory systems, as taste, touch, sight, sound, and smell are still critical.
The Tactile System
- Your skin is your largest organ.
- The tactile system is the sensory receptors that sense pain, temperature, touch, and pressure.
- Light touch tends to be disorganizing to a child; most like deep pressure
- Some people pull away from light touch or are bothered by tags in a shirt or touching sticky things
- Others may crave or seek out touch
It is important to talk to families about the skin and the tactile system, the largest sensory system. It is the first to develop in-utero. Many kids do not like to touch sticky and gooey things. They also do not like certain foods or textures, or tags in their clothes. They may not like doing certain activities. These aversions to certain input impede their ability to get dressed, complete arts and crafts, or those kinds of activities. Some children crave touch called "sensory seekers."
SPD Subtypes
Figure 1 shows the sensory subtypes, and this is Dr. Lucy Jane Miller's model out of the Star Center and the Research Center in Denver, Colorado.
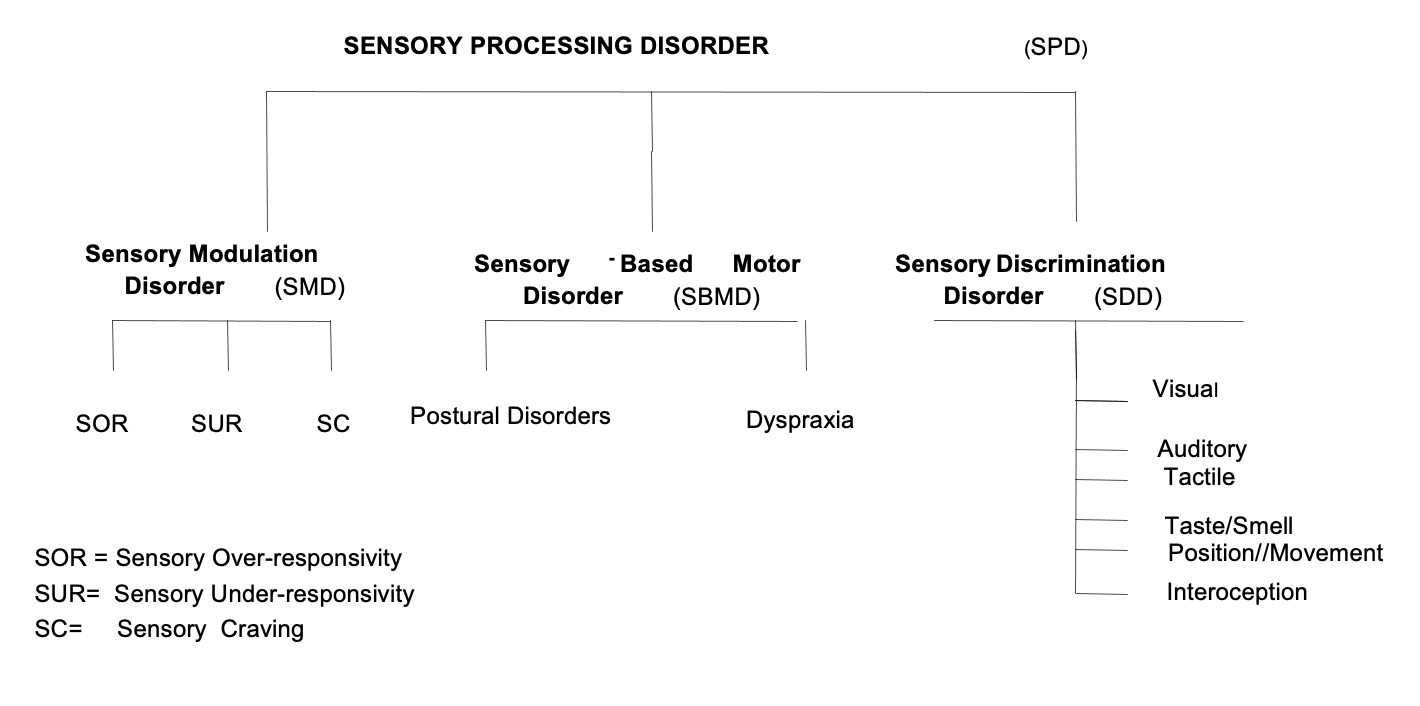
Figure 1. SPD Subtypes by L.J. Miller, 2007.
I worked there for several years. It is pretty amazing what all they are doing out of the Star Center. They have some other new research about testing for sensory processing, which is much needed. We need more standardized testing because it is hard to identify where kids are falling on this spectrum of SPD.
Let's now go through the subtypes. Sensory modulation disorder is broken down into three subtypes. We are also going to talk about a sensory-based motor disorder that is broken down into two subtypes. Then, we will talk about sensory discrimination disorder, in which you can have discrimination in any of the sensory systems.
Sensory Modulation Disorder (SMD)
- Sensory modulation is the ability to regulate and grade responses to the environment, so the responses to sensory input are appropriate to the demands of daily life. (Miller, Anzalone, Lane, Cermak, & Osten, 2007)
- 3 Subtypes
- SOR, SUR, SC
Sensory modulation is the ability to regulate and grade responses to the environment so that the responses are appropriate to the demands of daily life. There are three types: sensory over-responsivity, sensory under-responsivity, and sensory craving.
Sensory Over-Responsive
- SOR- these kids have responses that are too quick, too big, or last too long than typical kids
- It is hypothesized that their threshold is too low, and the therapist is working to raise that threshold.
- Examples: clinging to you when you try to toss your child into the air
- Tactile defensive to being barefoot in the grass or touching sticky and gooey things
- Covers ears when something seems too loud
Sensory over-responsivity is when kids respond too quickly, too big, or too fast. It is hypothesized that these kids' thresholds are actually low, and kids have a big reaction to sensory input, like a sound. As OTs, we want to raise this threshold to a more normalized setting. This way, the child will have a more typical response with incoming sensory input. You may see this in kids that you toss-up in the air, and they cling to you because they are fearful. Or, you put them on a swing, and they do not like it. They often do not like their feet being off the ground or walking barefoot in the grass. Touching sticky or gooey things is avoided. They may cover their ears or look fearful with loud sounds. As therapists, we want to make sure that we give these types of kids a certain specific input. This includes heavy work paired with movement to regulate and calm that sensory system.
Sometimes, the responses can be mixed. For example, a child may be over-responsive to auditory stimuli but in another category for tactile input. Thus, it can be a little bit challenging to explain to parents. We may still be figuring it out as we are observing and working with kids. "Today, it looks like they are more over-responsive because they are more dysregulated." Then, on another day, we might see that it is not as much of an issue. They also may be more of a sensory craver in another category. It can really be a mixed presentation.
Fight, Flight, or Freeze.
- When there is a sensation that our body registers (i.e., a loud siren), we process it in the brain, then our body has an adaptive response. Sometimes we register, “Ok, that is a siren. I am not in danger.” and move on. Others may register, “That is a siren. I need to run and hide,” or that loud siren sends the body into a physical reaction stage or shutdown mode.
- We have to help our children with sensory challenges learn when and how they need to react and how to have the Appropriate Adaptive Response (for some children on the autism spectrum, this can be very difficult)
Kids that are sensory over-responsive may go into fight, flight, or freeze mode. When there is a sensation, our body registers it. Let's say we hear a loud siren. We process it in our brain, and then we have an adaptive response. "That's a siren, but my house is not on fire. I'm okay." Others may register that, "There's a siren. I need to run and hide." Or, they may have a physical reaction where they demonstrate fight, flight, or shut down (freeze). This is the same thing with kids who may just hear the sound of the flushing toilet and go into panic mode. It could be something as simple as someone lightly touching them.
SOR Video.
We are going to watch a little video about SOR. You will be able to hear this little boy who is very uneasy about being off the ground.

This child is about four and a half years old. He is so uneasy with his feet being off the ground, and he does not like to be climbing in and out of things. He also does not like to swing. Even when his mom picks him up, he clings to her. She says that he has a hard time when his dad wants to play rough with him and swing him around. He cannot tolerate it. Clearly, he is over-responsive to vestibular movements and where his body is in space. You can see him say, "I want a little bounce." However, he only wants one in the beginning. Then, he says he wants two. This is an excellent example of a kid that is over-responsive.
Sensory Under-Responsive (SUR)
- SUR: this kid feels things too late and too little. He is low and slow, almost lethargic.
- It is hypothesized that these kids have a high threshold, and therapists want to lower this.
- Examples: He doesn’t hear his name being called
- She falls and doesn’t cry or notice she hurt herself
- Hard to motivate to move
- Your child may not be able to tell whether the water is too hot or too cold.
The second subtype of sensory modulation disorder is sensory under-responsive. These kids feel things a little too late. They are low, slow, and kind of lethargic. The hypothesis that these kids have a high threshold. Thus, we need to lower this threshold so that that sensory input that comes is a more normalized response. You will often see a kid who does not hear their name being called or cry when they fall and hurt themselves. They may also be hard to motivate. They may not be able to tell when the water is too hot or too cold.
I worked with a preschooler, "Sarah." She would sit and listen, but she did not really sing any of the songs during circle time or participate. Her mother reported that she sang (the hello and cleanup songs) at home. Auditorily, she was absorbing the information, but it was just taking a while to come out. Eventually, she learned how to catch up and sing with the other kids, but it took her a long time to increase the processing speed.
SUR Video.

Here is a little video. This video is quiet. I want you to look at this little boy's posture. He and I are singing the ABCs. He has a very low tone and drools a lot. He is drooling everywhere, so I have a little towel. He has a visual schedule, and he will try to pick an activity that he wants to do next. I purposely gave him a lot of options to show you just how overwhelming this can be.
Here I am with a speech therapist. We are co-treating and trying to get him to keep his head up to work on core strength. "Let's do 10 on your tummy. One, two, three. Keep your head up. Four, five. Not only is he SUR, but he definitely has motor issues too. I saw this little boy a couple of years ago and he is probably 12 now, and he is doing phenomenally. He definitely still has some cognitive and motor delays, but he is doing well.
Sensory Cravers (SC)
- SC –Even if a child seems to be seeking deep pressure or input, we don’t want to give them too much as this will disorganize them.
- Examples: always on the go, constantly moving
- Crashing, giving hard high fives
- Spins a lot, jumps a lot
- Overstuffs their mouth with food
The third category of sensory modulation disorder is sensory craving. These kids seek out deep pressure, hard high fives, jumping and crashing, overstuffing their mouth, and are constantly moving.
- For this category of SMD – if a child constantly wants to spin, you don’t just let her spin and spin. She will eventually habituate to the input and will never quite “fill the sensory system up.”
- What you want to do as a therapist is to spin the child in one direction, pick up the ball, spin the other way, and throw to a target.
- You want to give them some input but interrupt it with a functional task.
- Also, if they are seeking out vestibular, give them auditory or proprioceptive instead. If they are seeking out auditory, you aren’t going to blast their music even louder. Instead, you would give them tactile or proprioceptive input paired with a functional task.
We do not want to give them what they are seeking. If we have a kid that wants to spin, we do not let them spin and spin and spin. This is going to spiral them out of control. Instead, we want to give them heavy work paired with movements like a sensory obstacle course or activities in a multi-rich environment.
Examples are crawling through a tunnel, throwing the bean bag to a target, jumping 10 times and crashing, and crawling through the tunnel again. This helps them to be calm and regulate. These types of activities can be helpful for kids that are over-responsive, under-responsive, sensory cravers, with decreased motor skills, all of those things. This is why in a clinic setting, it is important to have access to these things. You can throw a blanket over the top of a kitchen table in the home and make it a tunnel or have them crawl underneath chairs. The couch cushions on the floor can create a space for crashing. A mini trampoline is great. They can also bounce and roll an exercise ball.
For those sensory cravers that are seeking out vestibular input, give them auditory or proprioceptive input instead. If they are seeking out loud and intense auditory feedback, do not blast their music even louder. Instead, you would give them tactile or proprioceptive input paired with a functional task. We already know play is great, but you also want to make sure that they are doing their daily living activities.
SC Video.
Here is a video of a kid who is a sensory craver.

He wants to play and is trying to slow his body down, but he just cannot. His mom struggles at home with getting him dressed, sitting and eating a meal, or having him follow directions. They tried to put him in two different preschool settings, and he got kicked out. These kids can be hard to manage. You need to work with them and help train the parents and caregivers to follow through. I think this is one of the biggest challenges. We also need to work with the teachers and staff. Often, we only see a kid 30 minutes to 1 hour a week. We have to rely on other people to help follow through with the interventions. There may be times when you come home at night and think, "I tried my best. I have to leave it in the hands of other people to follow through."
Sensory Based Motor Disorders (SBMD)
- Dyspraxia – difficulties with ideation, sequencing, motor planning, and/or execution
- Postural Disorder – difficulties with the overall tone, trunk strength
Sensory-based motor disorders are broken down into dyspraxia and postural disorder. Again, if you are a seasoned OT, you already know a lot of this. I am going through all of this so that you have the background and can share it with your parents/caregivers/teachers.
Dyspraxia/Motor Planning
- Individuals with Dyspraxia have trouble processing sensory information properly, resulting in problems planning and carrying out new motor actions.
- These individuals are clumsy, awkward, and accident-prone. They may break toys, have poor ball activities or other sports, or have trouble with fine motor activities.
- They may prefer sedentary activities or hide their motor planning problems with verbalization or fantasy play.
These are kids who have trouble with executive functioning. They may also have trouble coming up with ideas and planning how to get dressed and play on the playground. These kids may prefer sedentary activities or try to hide their motor planning problems with verbalization or fantasy play at times. They may also have trouble with fine motor activities.
Motor Planning/Praxis.
- Praxis is the ability to self-organize
- Starting with an idea (ideation)
- Sequencing how to carry out the idea (organization)
- Making your body complete the activity (execution)
- Examples –
- Crawling across the room
- Making a craft project (cutting, writing, etc.)
- Getting dressed
Motor Planning Activity.
I am going to have you complete a motor planning activity. This is something that I do with my families because I want them to understand what a motor planning task might be. I have the kids do this too.
Close your eyes. I want you to try then to bring your index fingers to your nose, alternating. You are probably familiar with this finger-to-nose task if you have administered the Bruininks (BOT-2) or other motor assessments. This is an example of motor planning and body awareness.
Another task in the BOT-2 is a jumping game where the child has to put a right hand forward, left hand back, right foot forward, left foot back, and then jump and switch. You can then have them do the opposite with the right hand forward, the left hand back, the left foot forward, and the right foot back. Most people have not done that pattern before. Many have done jumping jacks, but they have not done this sequence. This is switching the motor planning between the tasks. When I do this with parents and teachers, they think it is pretty fun and see a big reaction. "Oh, this is really hard." This helps them see that giving a child a seemingly simple task like putting on their shirt and buttoning it, even if it is age-appropriate, might be a challenge if they have a problem with motor planning. I also try to get them to do the finger to thumb task to look at coordination, motor planning, sequencing.
Can a kid come up with an idea to do a craft project? Can they gather all the materials that they need? Are they able to sequence that? This is also a huge part of executive functioning, which we will talk a little bit more about in a little while.
Postural Control
- Individuals with postural disorder have difficulty stabilizing his/her body during movement or at rest to meet the demands of the environment or a motor task, e.g., poor “core strength.”
- When postural control is good, the person can reach, push, pull, etc., and has good resistance against force.
- Individuals with poor postural control often do not have the body control to maintain good standing or sitting position, especially when attempting functional tasks.
Individuals with poor postural control have difficulty stabilizing their movement at rest to meet the demands of their environment. They may have poor core strength. To maintain a static posture, the child has to engage their core muscles. Many people have great dynamic movement. They can snow or water ski, but they cannot sit still in their chair because they do not have great static postural control.
Kids who have poor postural control tend to be more lethargic. They are working so hard to maintain their posture that they lose their focus or attention and have trouble with motor skills.
Discrimination
The last subtype of SPD is discrimination.
- Tactile
- Visual
- Auditory
- Taste/Smell
- Vestibular (position)
- Proprioception (movement)
- Interoception
Discrimination can happen in these different sensory areas: tactile, visual, auditory, taste, smell, vestibular, proprioception, and interoception.
- Identifying specific qualities of sensory stimuli and attributing meaning to them. They have problems determining the characteristics of sensory stimuli. The result is a poor ability to interpret or give meaning to the specific qualities of stimuli. (Do I see a “p” or a “q”? Do I hear “cat” or “cap”? Do I feel a quarter or a dime in my pocket? Am I falling to the side or backward?).
- Those with SDD have difficulty detecting similarities and differences among stimuli. They may appear awkward in gross and fine motor abilities and/or inattentive to people and objects in their environment. They may take extra time to process the important aspects of sensory stimuli.
Sometimes it is hard to identify if the kids are having processing speed challenges or the environment. You can reassess them in a calm, quiet environment and not put any motor demands on them to check this. I will show you a really great processing speed test to discern if it is a processing or a sensory problem.
How To Set Up Treatment
- Children with ASD often present with atypical responses to sensory stimuli (Reynolds, Lane & Thacker, 2012).
- Research shows us that patterns of neurophysiological response vs. isolated responses to individual stimuli may help us determine better subtypes and, therefore, better diagnosis and treatment planning.
- Children with learning disabilities and other co-existing diagnoses often show difficulties processing and integrating sensory information and struggle with effective motor planning and praxis skills (Aguilar, 2019).
- We need more research to look at the subtypes and how it affects our children with SPD and behavior-based sensory subtypes concerning neurophysiological response patterns (DeBoth, 2017).
How do we set up treatment for these kids? Children with autism spectrum disorder often present with atypical responses to stimuli. Research shows us that neurophysiological response patterns versus isolated responses to individual stimuli may help us determine subtypes better, therefore better diagnosing and treating planning. Children with learning disabilities and other coexisting diagnoses also show difficulty with processing and integrating sensory stimuli. We know a lot of this time this co-exists, and we really need more research to show how we can determine what is going on. As I said, sometimes I think I have it figured out. They may start to show a little more regulation in one area, but they become completely dysregulated in another area.
I am a feeding specialist and am SOS trained. Before a feeding session, I like to have them do some sensory movement or some tactile input and heavy work before eating. When we get to the table, they still may be over-responsive to tactile stimuli. It is challenging, and sometimes we have to think on our feet. There can be a lot of trial and error.
Sensory Processing 3-Dimensions Scale
- SPD-3 a performance-based measure for assessing sensory processing
- Research out of STAR Center and Research Institute
- Measures 3 primary dimensions 1. sensory modulation 2. sensory discrimination 3. sensory-based motor abilities
- Children ages 3-13 years old
- Still being researched and developed
This is some new research from the SPD Institute at the Star Center and Sensory Research in Denver. The SPD-3 is a performance-based measure for assessing sensory processing. It measures three primary dimensions: sensory modulation, sensory discrimination, and sensory-based motor abilities from children ages three to 13. This is something to keep an eye out for on the Star Research Center's page.
I get many questions from parents about the differences between SPD and autism and SPD and ADHD. I wanted to give you guys a couple of slides on here because this helps me when I am talking to my families.
SPD Vs. ADHD
- Many children who are SPD and are sensory seekers/cravers may look like they have ADHD. Also, those with poor postural control can look like a child with ADD.
- Often, we think these kids are acting out, not listening, or not paying attention. They get sent to the principal's office and get labeled the “behavior kid.” We need to look deeper into the underlying issue.
With ADHD and SPD, it seems like a chicken or the egg scenario. Are they not focusing because they have ADHD/attention issues, or are they having trouble focusing because they have poor postural control and cannot maintain a static posture to get their work done or follow directions?
Is it auditory processing, or is it attention? I think most kids under the age of five have attention challenges. They are little and have to learn what is expected of them. A three-year-old is not going to sit down and focus for 20 to 30 minutes with no movement. That is pretty hard for them. And if your kid does that, then they may be more of a low, slow-to-respond kid. Could a 10-year-old with weak core strength, poor postural ability, and poor focus have both ADHD and sensory issues? Maybe. What is really going on? Where is this starting? Many times, people think these kids are acting out, not listening, and not paying attention. They get sent and labeled as a "behavior" kid, but we need to look deeper into the underlying issue is.
ADD (Inattentive Vs. Hyperactivity)
- One of the most common neurodevelopmental disorders of childhood
- It is typical for all children to struggle with attention from time to time
- Extreme difficulty paying attention
- Impulsive behaviors
- Staring off into space
- Talking too much
- Trouble taking turns or waiting to speak over others
Attention Deficit Disorder (inattentive versus hyperactivity) is one of the most common childhood disorders now. I get a little bit worried that it is over-diagnosed, especially in our kindergartners. Yes, I feel that there is a place for medication and therapy. Again, there is also a lot of trial and error. However, I think there are things that we can do to help these families go through the process and see what is really going on before they try the medication route. Some families are really interested in doing this as they do not want the medication. They want to try everything until they can exhaust all other options first.
These kids may have extreme difficulty paying attention, impulsive behaviors, and may stare off into space or talk too much. They may have trouble taking turns and waiting to speak. I have a newly turned five-year-old, and I have a little ADD myself. I have always struggled a little bit with it, but it has always worked to my advantage as an OT. I also think my daughter may have it. Now that she is five, we are doing many OT strategies at home like mindfulness and yoga to work on her emotional regulation, her inability to take turns and wait her turn to speak. She says, "Mommy if I do not ask you right now, I am going to forget what I want to say." I tell her to store it over here on this side of her brain and then bring it back up here (front) to your prefrontal cortex, and then you can tell me. She totally gets it.
Drawing Activity
Please get a piece of paper and a pen or a pencil. I would love for you to quickly draw or write a short description of your favorite childhood activity. I also want you to draw or write a few little notes about your favorite thing to do when you were a kid. Give me some examples. Here are some of the results:
- Parachute activity
- Jump rope
- Roller skating
- Swimming
- Coloring contest
- Playing with Barbies
- Ride a bicycle
- Played on the playground
- Climbed trees
- Dancing
- Swinging
- Playing in the woods
- Building a fort
- Gymnastics
- Ride horses
- Cooking with mom/grandma
Everybody mainly listed outdoor activities. Where are our kids right now, especially during COVID? However, even pre-COVID, our kids are inside. I do not want to discount anybody like the person that said their favorite activity was coloring, playing with Barbies, or cooking with mom or grandma. Those are phenomenal things. Did anyone tell me their favorite childhood memory was playing a video game? Most of us have a memory that is sensory-rich and physical activity. It is cooking with mom. It is pretend play with Barbies. It is outside swimming, playing a parachute activity, and climbing trees. What are our kids doing right now? Our young kids are inside on iPad or phones. Schools are taking away recess sometimes for behavior issues. When I present to teachers and schools, I always implore them not to take away recess. If there is a consequence needed for behavior or not getting their work done, figure something else out.
There is a place for an iPad, a game, and other educational activities. If kids are on Zoom or virtual school, that is fine, but then get them outside. Some of my favorite childhood memories are also swimming, playing in the woods, and climbing trees. We lived with woods behind our house. That was a big deal for us.
Do this activity with your families because it is much more impactful than telling them to take their kids outside.
Creating A Sensory Lifestyle
- We don’t use the term “Sensory Diet” anymore.
- A Sensory Lifestyle is how you incorporate the sensory tools that you have into everyday life.
- It is not a specific “diet” for a child because every child is different.
- We will talk about activities and strategies, but it's best to learn what works best for the child you are working with through trial and error.
Hopefully, you guys know that the term sensory diet is not really used as much anymore. I still hear it occasionally. We want to get away from that term because diet means food and is very specific. It usually means a regimen that one is following. Creating a sensory lifestyle is about utilizing your sensory toolbox and pulling from that. As I said, that is why being a little ADD is probably good for some of us OTs or being an "out of the box" thinker. Some people are even better at it than I am. They can create these amazing adaptations for kids. I always yearn to learn more from those therapists. They are so flexible in their thinking.
Today, we are going to talk about activities and strategies. However, you still may have to go through trial and error with each child. Sometimes, we go through A, B, C, D, E, F activities and then go back to B as something may only work for a little while. For example, a brushing protocol may help with regulation and tactile defensiveness. A weighted blanket might help with calming, and crunchy and chewy foods can help for oral motor seeking, but then it stops. You then have to add some more activities back in. I may need to remind parents, "Hey, let's go back to doing some more of those chewy and crunchy foods," or "Start calming and mindfulness activities before bed again." Remember that you can go through your list and come up short and then go back to something that might work for the child.
How Does Sleep Affect Your Child?
- Sleep is essential for a child and the whole family
- Consistent bedtime routine
- Comfortable bedding (weighted blankets)
- Calming music or lights (night light)
- Try to have the child sleep in their own bed
- Create a tent over the bed if needed
- Body pillows can be comforting
Sleep is vital for a child and the whole family. A consistent bedtime routine, comfortable bedding, calming lights, music, the child sleeping in their own bed are all essential, especially if they have sensory challenges. You can create a tent over their bed and use body pillows. We want to make sure that we are giving our families ideas on how to sleep better.
What About Diet?
- Eating healthy is also very important for your child
- If you have major concerns about your child’s limited food repertoire or “picky eating,” seek out a therapist who is trained by Dr. Kay Toomey SOS Approach to Feeding.
- Children need at least :
- 10 sources of protein
- 10 fruits or vegetables
- 10 other/starches
- A total of at least 30 different foods
If you have major concerns about your kids' limited food repertoire, look into a feeding course. I am SOS trained with Dr. Toomey. I have also done a couple of other feeding courses. I also have a ton of feeding resources. Feeding can really impact a lot of what else is going on. If you have a caregiver that is complaining about their child not getting the recommended 10 sources of protein, 10 sources of fruits or vegetables, and 10 sources of starch/carbs (a total of at least 30 foods) or their kid is only eating chicken nuggets five days a week. I would look into getting them some support with a feeding specialist.
Dinner Time Tips
- Family style dinner
- Make Eating Fun!
- Try different textures, colors, smells
- Have something preferred for after the child touches or tastes a new food
- Always present a protein source, fruit or vegetable, and starch at every meal/snack and one preferred food
- Don’t allow your child to “food jag” eat the same foods over and over again
- If they have chicken nuggets on Monday, they can’t have them again until Wednesday
Some tips for dinner time include creating family-style dinners, eating fun, using cookie cutters or colored toothpicks, and using different textures, colors, and smells. My daughter last night wanted to get flour, water, milk, apple sauce, spices, and add cornstarch to it to thicken it up and put it in the microwave. Then, she mashed it all up and played with it. I am all about getting messy, but this was right before bed. I let her as she was clearly looking for sensory stimuli. We spent 10 minutes doing that and a few minutes cleaning her and her brother (two and a half years old). They were a little bit later getting to bed, but everybody was more regulated. It is hard to do these things when there is much to do as a busy mom and you are exhausted. However, sometimes kids tell you what they need, and we have to remember that.
When you present food to kids, always present a protein source, a fruit or vegetable, and starch at every meal/snack. At least one of those needs to be preferred. Do not allow your kid to "food jag," which means they eat the same foods repeatedly. If they have chicken nuggets on Monday, they cannot have them again till Wednesday. I know some of you guys are thinking, "Well, I like Cheerios and strawberries every morning for breakfast." That is actually my mother-in-law. She loves Cheerios and strawberries Monday through Friday, and on the weekend, she eats pancakes. She is also 74, so she can do that. We need to try to get kids to eat a variety and not get stuck on the same foods over and over again.
How To Regulate A Child
- Watch their facial expressions and body language.
- Watch that you are not overwhelming them to the point of shut down
- Pay attention to their arousal level so they don’t get too wound up, and you can’t bring them back down
- If they are melting down, help calm them using whatever strategies seem to work for that specific child
Here are some thoughts on regulation.
Where OT’s Can Play A Part
- Among the psychosocial conditions, anxiety disorder is the third prevalent mental disorder affecting children aged 3-17 years (CDC, 2019).
- OTs are a great resource for therapy for implementing evidence-based mental health promotion.
- Emotional Regulation
- Executive Functioning
- Mindfulness
- Yoga and more!
This is where OTs can play a part. I know you are thinking of a kid in your mind right now that has meltdowns, emotion regulation issues, and behavior issues. You may have tried calming strategies, sensory movement, executive functioning activities, and mindfulness. I hope that I can give you some more ideas on how to work with those kids.
Finding The Just Right Challenge
- Zones of Regulation designed by Leah Kuypers, M. A. Ed., OTR/L - part of Social Thinking- Michelle Garcia Winner's program
- www.socialthinking.com
- www.zonesofregulation.com
- Too Slow- blue
- Just Right- green
- Fun Fast- yellow
- Too Fast- red
Finding the just-right challenge is significant. I hope that many of you guys are familiar with the Zones of Regulation. It is great for school, for home, for your own kids, and yourself as a parent and OT professional.
Social thinking is Leah Kuypers and Michelle Garcia Winner's program. They have four color zones, and I like this a little bit better than some of the previous color zone programs out there. Too slow is blue. Just right is the green zone. Fun/fast is that yellow zone. And, too fast is the red zone. If you go to zonesofregulation.com, you can go to their free downloadable handouts. I use this with almost all my kids, even the really young ones like three and four-year-olds if they are starting to get it. The blue zone is sad, sick, and tired. The green zone is happy, calm, focused, and ready to learn. Yellow is that fun fast zone feeling like at a playground or a birthday party. This is sill, wiggly, and excited, but it can also be frustrated and worried. The red zone is mad, angry, hitting, and out of control. It can also be elated, hyper, or crazy where they are out of control.
We cannot do therapy with a kid in the red zone not can we do much therapy with kids in the blue zone either. I like my kids to be green or yellow when I am working with them. If they are at either end, I have to work on strategies to get them back to where they are ready to learn. My daughter will say, "Mom, I'm green with yellow polka dots." Then she may say, "Mom, I'm yellow with red polka dots." This is when we need to talk about calming strategies. Sometimes, we get all the way to the red zone, and I missed it. This is when she is yelling, hitting, and losing patience. Zones can be beneficial to identify these moods.
Calming Strategies
- Taking Deep Breaths
- Drinking through a straw
- Sucking on hard candy
- Taking a break
- Lowering the lights
- Calming music
- Warm bath
- Talking in a soft voice
- Slow linear swinging/rocking
- Chewing gum
- Deep pressure/hugs/weighted vests, blankets
Here are some calming strategies. Drinking through a straw or sucking a water bottle can be calming. Smoothies are great because they give them more input. Other ideas are calming music, a warm bath, and lowering our voices.
How do you regulate yourself to then co-regulate that child? As babies, they do not know how to regulate themselves. Our job as a parent is to co-regulate our infants. Kids that we see in OT do not know how to regulate themselves either. We have to co-regulate them. I tell parents if they are in the red zone, they need to walk away. I have to tell myself this too. Walk away until you are calm, as you cannot work on co-regulation if you are both in the red zone. Sometimes, it is my child that brings me down. Partners can also help you to regulate. Chewing gum is another calming strategy if it is safe and appropriate. Slow linear swinging (not spinning or in big arches) or rocking can be really calming.
Executive Functioning
- Many children are being identified as having EF challenges
- Children have trouble with impulse control, organization of materials, keeping track of time, multitasking, planning and prioritizing, and work production
- Cognitive testing can show challenges in the areas of working memory with children who have ADHD and/or have EF difficulties
- EF is more of a cognitive process vs. praxis being a motor process
We talked a lot about motor planning and dyspraxia. How does that affect executive functioning? Children that have trouble with executive functioning may have trouble with impulse control, the organization of materials, keeping track of time, multi-tasking, and all of those things. Cognitive testing can also show challenges in working memory with children who have ADHD or executive functioning issues. I encourage you to take a course on executive functioning. I personally love Sarah Ward's executive functioning courses.
Executive Functioning Videos
These are some great video clips that you can watch and share with your families. These are a great way to show how executive functioning can impact a child. Use those tools and strategies shown.
Mindfulness
- Mindfulness is defined as a mental state achieved by focusing one's awareness on the present moment while calmly acknowledging and accepting one's feelings, thoughts, and bodily sensations. This is used as a therapeutic technique. This is all about living in the moment and taking every moment just as important as your last.
Mindfulness is my favorite strategy. Mindfulness is defined by our mental state, focusing on our inner self, our one's own awareness. If you have an ADD brain like me, close your eyes and take a deep breath to calm yourself. Currently, my brain is thinking that a guy is cutting the grass across the street. It is auditorily a little bit distracting, but I am trying to push through. I am also thinking, "How much time do I have left, and am I going to get through everything?"
How do you stop those thoughts and be still? How do you teach a kid to do that? It can be so hard. All we want them to do is to take a moment to be still and think. You can do this even with your little two-year-olds.
- Mindful Life For Schools/Home
- According to Kristen Race, PhD, Founder of Mindful Life ™, Mindful Body, Mindful Listening, Mindful Breathing, and Mindful Eating are important parts of becoming mindful. She created a curriculum for schools to train their teachers and staff in bringing mindfulness into the classroom. See chapter 11: Yoga in Schools for more information regarding her program.
Mindful Life for Schools and Home is a program that Dr. Kristen Race presents. She is the founder of Mindful Life. She talks about a mindful body, mindful listening, mindful breathing, and mindful eating. In my "Yoga for Schools" book, in Chapter 11, there is a lot of information about her program. She also has her own book and resources on a mindful life.
- Mindfulness Can Improve Our:
- Awareness
- Focus
- It helps change our brain
- Reduces stress and depression
- Helps build relationships
Mindfulness can improve our awareness and focus. It helps change our brain, reduces stress, reduces depression, and helps us to build relationships.
- Why Is Mindfulness Important?
- Children are experiencing more stress than previous generations
- 1 in 5 children ages 9-17 have some sort of mental disorder
- Increased diagnosis; depression, anxiety, ADHD, bullying, violence, etc.
- Stress on the brain and PTSD creates problems
More kids are getting diagnosed with anxiety, depression, ADHD. There is also violence and bullying that create so much stress on the brain and PTSD. According to the research, one in five children, ages nine to 17, has been diagnosed with some sort of mental disorder. And, COVID has added so much more stress. Thus, we need to work a little harder to get these kids regulated.
- Reaction to Stress
- Wear and Tear on Body Systems
- Reduced Optimum Health
- Increased Sensitivity to Stress
- Stressor
Stress creates wear and tear on the body and reduces the optimal level of health. There is then increased sensitivity to stress, causing more stress. I bet that every single person seeing this can raise their hand and say that they felt more overwhelmed and stressed during the last year. It has been challenging. Think of all the children who may have had many sensory and postural control issues and motor issues prior and now are in a home life that is not quite as calming and regulating. Put yourself in their position to say, what can we do to help them?
How many of you guys have seen a breathing ball? A Hoberman sphere? I love these things. These are phenomenal. These are all through the Mindful Life program and can be found online. You can use these for anything. These are great tools to work on breathing. There are big ones as well that the kids like to climb inside of. These are really inexpensive. I try to get families to buy one of these for home or get funding for those who cannot afford them. I also have this tone bar and a singing bowl that I use for mindful listening. This is something I use with my own kids and myself. There are some YouTube videos on singing bowls that you can check out. There are many resources online for breathing, mindful listening, mindful movement, and movement and yoga.
- Core principles of mindfulness
- Understanding the brain
- Attention and Awareness
- Emotion Regulation (part of Sensory Processing)
- Empathy/Compassion
- Cognitive Flexibility/Creativity
The core principles of mindfulness are understanding how the brain works, increasing our attention and awareness, and emotion regulation. It also includes empathy and compassion and creating cognitive flexibility and creativity. I have listed several articles that I found in AJOT. There was a lot on mindfulness and meditation to improve body awareness. That was in AJOT, and it was a great article. One, in particular, is the mental health benefits of a mindfulness-based prevention program on elementary-aged children. If you go into AJOT and type in mindfulness, you will find these articles. There is a lot of great information.
Power of Positive Thoughts
- Negative Thoughts grows Weeds
- Positive Thoughts grows Flowers
- Gratitude (write down 3 things a day you are grateful for), Compassion and Kindness (doing something for someone else), RAK
One thing I like to do is have my kids draw a big sunflower. I draw the ground line and the roots. I talk about how negative thoughts grow weeds, and I draw some weeds around the flower. I also say that positive thoughts grow flowers. Talk to your kids, whether they are two, five, 10, 15, or even yourself. What is it that helps you with positive thoughts?
Gratitude is another area. Write down three things a day that you are grateful for. You can show compassion and kindness by doing something for someone else, like a random act of kindness. I grew up with a sister with special needs. I have seen life from my mom's perspective. This is something that I wish we had done a little bit more when I was younger. Write down things you are grateful for because when you have a child with special needs, autism, down syndrome, ADHD, sensory, gifted, two E, cerebral palsy, medically fragile, or whatever it is, there is a lot of stress. Caregivers can be bogged down with everyday struggles and forget to write down the positive things.
All of us love our kids and want to be positive for them, but many of these moms and dads need a break. Often, when they come to therapy, they are thankful and think this is the time for them to take some respite. However, we really need them to be there and be present to carry through what we are teaching them. I think that this is so important.
Yoga for Kids
- Yoga can be fun for kids. It does not have to look like what we think yoga looks like calm, quiet, etc.
- It can be silly and goofy or calm and organized depending on the child and their needs.
- Sometimes it takes a while to get a child to participate in yoga or other therapeutic movement ideas, and being patient is a great tool for parents and caregivers.
- You cannot force it. Sometimes, I will let children watch me, and then when they are ready, they can join.
Yoga for kids can be fun. It does not have to look like what traditional yoga looks like. It does not need to be calm and quiet. It can be silly and goofy, but it can also be calming if that is needed. You can help encourage kids by modeling the movement. And if they have a physical disability, you can gently help with the movements and positions. If they are not hurting themselves, I let them imitate me and do what they can to move their body. Again, if they have cerebral palsy, a physical disability, or low postural control, I might help them gently move through a position. You do not need to be a yoga teacher or have your yoga certification. This is just a strategy for you to use. You are not trying to teach them to do a perfect yoga sequence, but rather, you want them to move.
History of Yoga
- Deep breathing, meditation, massage, and yoga have been identified as the four complementary and alternative medicine therapies used by adults in the United States that significantly increased from 2002 to 2007, with deep breathing and yoga identified as the third and fourth most commonly used interventions with children during the same time period (Barnes, Bloom, & Nahin, 2008).
- The history of yoga started back more than 5000 years ago. The origins of yoga are speculated to pre-date Indian traditions, and many religions like Hinduism, Buddhism, and Jainism later adopted many yoga techniques. The literal meaning of yoga is “to add,” “to join,” “to unite,” or “to attach.”
- Yoga is not a religion; it does not have a set of beliefs or worship of a god. As an OT, I use yoga practice for therapeutic reasons to improve regulation, movement, strength, and coordination.
The history of yoga is about deep breathing, meditation, and massage. When I worked at a school, we were allowed to call it yoga. In other places, we had to call it mindful movement.
The Yoga System
- The yoga system was built on three main structures: exercise, breathing, and meditation. Exercise is for the body’s total health and strength; breathing is the source of life for the body, and meditation is to help quiet the mind and allow healing from daily stress.
The yoga system was built on three main structures, exercise, breathing, and meditation. Exercise is for the body's total health, and breathing is considered the source of life. Meditation is to help quiet that mind like mindfulness that we just talked about.
What Does Yoga Teach Us?
- Bodies – physical postures and exercise (called asanas) help bring strength and flexibility to our bodies. There are both active and passive asanas, and both benefit your mind and body for different reasons.
- Active poses help build strength, flexibility, and muscle tone. They also help move energy throughout the body and activate the brain and nervous system.
- Passive poses are mostly meditation and deep relaxation. These are typically done at the end of your yoga practice for 10-20 minutes.
Yoga teaches our bodies about physical postures and exercises called asanas. This helps us with strength and flexibility. There are active and passive poses. If you are moving through space, you are working on core strength, and passive poses work on relaxation. Typically, an adult would do a relaxing pose for 10 to 20 minutes. If I can get my kid to lie on the mat quietly, with some calming music or that singing bowl tone for 30 seconds, I feel like that is an accomplishment.
Breath
- Breath- breathing is a crucial part of life but do we actually take slow deep breaths effectively? Teaching a child how to breathe slowly and deeply (called pranayama) can bring calmness and energy to them. Pranayama is the formal practice of controlling our breath. We try to improve breathing patterns in children who are chest breathers to use a more diaphragmatic breathing technique. This type of breathing helps decrease stress and anxiety. Deep breathing helps us relax by de-activating the sympathetic nervous system (SNS), which produces stress hormones and activating our parasympathetic nervous system (PNS) instead. This helps lower blood pressure, decrease heart rate, and relaxes us.
You can do all kinds of different breathing like the breathing ball we talked about. You can also have the child blow a cotton ball with a straw after taking in deep breaths. You can have them blow dandelions. You can develop other ways to understand how to breathe deeply into their belly, up into their chest, and then exhaling. This helps the child to relax by deactivating the sympathetic nervous system, which produces the stress hormone. It activates our parasympathetic nervous system, the PNS, instead. This helps lower blood pressure, decreases heart rate, and promotes relaxation. Sometimes, I have them sit in my lap in a crisscrossed apple sauce position. I put my hand on their chest and their belly, and I just breathe. They will usually start to breathe with y
