This text-based course is an edited transcript from the live course, The ADLs You Didn't Know You Were Missing, presented by Jennifer Stone, PT, DPT, OCS, PHC.
Learning Outcomes
After this course, participants will be able to:
- Ask at least 3 questions to screen for impact on each of these ADLs in patients who are not primarily being seen for a "women's health" diagnosis.
- Identify at least 2 ergonomic practices and at least two good habits in these areas with patients with pelvic floor issues to maximize the impact of physical therapy.
- Participate in at least 2 behavioral retraining techniques with patients with pelvic floor issues.
Introduction and Overview
The goal of today's presentation is to provide you some tools and knowledge regarding how to help patients who may have symptoms of potential pelvic floor dysfunction, but who don't necessarily fall into the category of needing a full-on pelvic health physical therapist. There are a lot of things that you can do to help patients who have pelvic floor symptomatology that doesn't necessarily involve a detailed internal knowledge of the pelvic floor. The main ADLs that we will address today include breathing, toileting, sexuality, hydration, nutrition, and pediatrics.
Why Ask Questions?
Why should we be asking questions about the pelvic floor with our patients? I'm assuming that most participants in this course are probably not practicing in a women's health or a pelvic health-related clinic. You're likely seeing patients in a nursing home, an outpatient ortho clinic, or a similar setting. Orthopedic patients are not exempt from problems with their pelvic floors. In fact, there is a strong association between, back pain, hip pain, SI joint pain, and pelvic floor dysfunction. If you are not already aware of that, it's probably only because you're not asking about it. The vast majority of your patients with these types of problems do have some sort of symptomatology that would potentially impact their pelvic floor, or point to a pelvic floor component. The same is true for other fields as well. Geriatrics neuro patients have pelvic floors. Unfortunately, it's a portion of the body that we have marginalized, in a way, that we're forgetting that it could be a component with a lot of other patient types that we typically treat.
Many of the troubleshooting questions that are helpful with these patients are fairly easy and educational in nature. They don't require a lot of intimate pelvic floor knowledge. In my opinion, it's no different than helping people troubleshoot workplace ergonomics. If you're working with a neck pain patient, hopefully, you're asking them about their desk setup. By the same token, if you have a patient who you're seeing for low back pain, but they also have some constipation, for example, we should be comfortable giving them suggestions to help improve that.
As therapists, setting a good, comfortable atmosphere is our responsibility. These questions are only uncomfortable if we make it that way. It's our job to make it a routine part of our examination. When I do talks like this, particularly for therapists who are not interested in doing pelvic floor directed physical therapy per se, a common concern I hear is, "Isn't my patient going to raise some eyebrows or perhaps be offended if I ask them a question related to their comfort during intimacy or urination when they came in for back pain?" I understand that concern, however, I've found that the opposite is true. Patients appreciate being asked these questions because there may not be a lot of opportunities for them to discuss these concepts with healthcare providers. If anything, once you ask a question like this, the floodgates will open and patients will potentially give you far more information than you necessarily needed. But they're grateful to have the opportunity to troubleshoot these concepts with someone who's qualified to help them. It could be awkward if you make it awkward, but truthfully, for the most part, it is not.
Questions to Ask
There are some easy questions you can ask your patients if you would like to screen for some of these educational components to be included in their treatment session. I do still have patients who are simply not comfortable answering some of these questions. An easy way to get this information into your evaluation is to put these questions on your intake or screening form, where you have patients circle whether they have had a past history of a motor vehicle accident, or cancer, for example. That way, if the patient does indicate that on their form, you can circle back around and the concept has already been introduced.
Any problems with leakage of urine or stool?
I word the question exactly that way, using the word leakage and not incontinence. When people think of incontinence, they associate that with their grandmother who has to wear Depend undergarments, and when she stands up, she leaves a puddle. Any involuntary loss of urine or stool, even if it's just a couple of drops, is considered abnormal in almost all circumstances. Urine leakage is fairly self-explanatory. With stool, some people will say they can wipe and wipe and wipe and they can go to the bathroom, clean themselves off, and then the next time they go to the bathroom, even if they don't stool again, they've still got some that come off on the toilet paper (i.e., the "eternal wipe").
If they acknowledge any leakage, I will ask some additional, slightly more detailed questions to determine the severity. For example, I ask whether the leakage occurs with changes, such as when they cough, sneeze, laugh or jump. Or, it may be that when they have the urge, they have to go quickly or they won't make it in time. In other cases, some people have no idea the leakage is going to happen, and don't even necessarily know it did happen until they pull their underwear down. Coming up in the presentation, we'll talk more about implications for treatment and education.
I will also ask about the patient's fluid intake, what type of fluid are they drinking, and when are they drinking it. Finally, I ask if they know of any triggers that they've identified. Sometimes people recognize that leakage is more likely when they eat or drink specific things, or if they do a particular activity. Sometimes they can't identify a trigger. But if they know of any triggers, that can definitely be helpful.
Any difficulty starting or finishing the elimination of urine or stool?
I ask questions like, "Do you have to strain to start your bowel movement or to start emptying your bladder? How long does it take? Do you feel like you've completely emptied when you're finished?" As a side note, whether or not people feel like they're completely empty may not be accurate and reflective of whether they are actually fully emptying. I'm interested in the sensation that they feel.
Any pain with intercourse?
If you're not comfortable with the term intercourse, you could substitute the word intimacy instead. Patients tend to know what you're getting at if you say either of those terms. If they acknowledge that they experience pain with intercourse, I will ask them additional questions. Does the pain begin when they become aroused? Does it happen with that initial penetrative attempt? Does it occur with orgasm? Or all of the above? Perhaps they cannot even get to the point of penetration. I am trying to understand at what point during the process of intercourse that their pain is occurring. I'll ask them if position matters. A lot of people won't know the answer to this because it hasn't occurred to them to try a different position.
Any trouble with constipation?
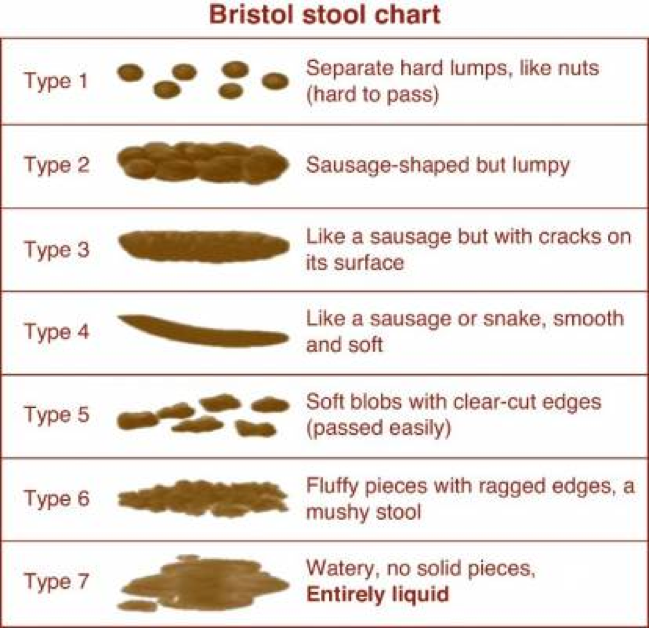
I would strongly encourage you to use something pictorial like the Bristol Stool Scale (Figure 1) when you're asking people about constipation. The vast majority of patients and even some healthcare providers don't necessarily know what constipation means. Constipation involves a lot more than simply the frequency with which you go. It also has to do with consistency and quantity. You can have a regular elimination, but still be very constipated. I think a lot of people interpret constipation to mean those people who only go once every couple of weeks.
I don't word the question as simple as, "Do you feel like you're constipated?" I'll show them the Bristol Stool Scale and ask them what they feel like most resemble their stool. We also have the Bristol Stool Scale on our intake form, and we ask patients to circle which one most closely resembles their stool. I also ask about the frequency with which they're going and whether they have to strain a lot to get started. That's very important in determining whether they're constipated or not. Again, I'm going to ask for their fluid intake, because one of the major factors that determine the consistency of the stool is fluid intake. We'll talk about that later as well.
Figure 1. Bristol Stool Scale.
The Bristol Stool Scale is a tool that I often use with my pediatric population. I see a lot of children for constipation and incontinence. In Figure 1, the first type of stool (Type 1) is the most constipated. On the bottom of the scale (Type 7), this type of stool is the opposite of constipation. It's diarrhea. Ideally, you want them somewhere in the middle range. There are very few of us who have exactly the same appearance of our stool every single day. You do want there to be at least some definition to it and not a lot of separation and lumpiness because that typically reflects a lack of hydration in the stool, which may not be the same as the person being dehydrated. The lower types on the scale (Types 6 and 7) often reflect some inflammation. It could be systemic inflammation or it could just be that they ate something that didn't particularly agree with them started having this GI inflammation.
For those of you who are treating orthopedic patients, particularly post-op patients, it is important to note that a lot of medications prescribed after surgery have the side effect of constipation, especially pain medicines. In that patient population, constipation does not necessarily reflect that they have a pelvic floor dysfunction. They certainly might, but it could truly just be a side effect of the medication. However, if it is not controlled well enough, their chances for developing some type of pelvic floor dysfunction significantly increase, because doing that kind of hard straining and the Valsalva pushing during a bowel movement is one of the main factors that lead to pelvic floor dysfunction. If it happens once in a while, it is not going to be a big deal, but if it's done over a period of time (several weeks to a month or more), then that can lead to some problems. I always ask about constipation in any type of post-op patient.