Erika: Hello! I would like to welcome everyone to my course. I am an occupational therapist and former adjunct professor. I founded Joy Energy Time in 2017, and I am the co-host of the Burnt Out To Lit Up podcast with my husband. He is a physical therapist. I experienced significant burnout during the first few years as a clinician, which inspired me to create this brand to help other healthcare professionals.
Burnout
Burnout begins with someone that is eager that enters the workforce with positive expectations and goals to be successful. No one thinks that burnout can happen to them. Over time, these positive qualities begin to erode into a sense of failure, ineffectiveness, exhaustion, and cynicism. We are strongly connected to our work and want to find meaning in that work. We want to seek satisfaction and fulfillment and have confidence in our roles at work. Burnout started to receive attention in the 1970s and it's now considered to be a huge problem in the modern workforce.
Three Components
Burnout consists of these three components.
- Emotional Exhaustion- The first one is emotional exhaustion. This is the strength dimension. Burnout depletes emotional resources, and the person is unable to give anything more at a psychological level.
- Cynicism- This means that a worker has a negative or depersonalized view towards those recipients of care.
- Low Efficacy- Low personal accomplishment makes a worker feel incompetent.
The most easily recognizable component of these three is exhaustion. In fact, people like to brag about exhaustion or how exhausted they are. They almost wear that like a badge of honor. However, people do not necessarily brag about cynicism because that carries a stigma. Cynicism can be viewed as unprofessional, and you can also feel distant not just from your patients but from your career as a whole.
Two Paths
What happens when someone is burnt out? There are two paths. The first path is that that person may leave their job or leave the profession entirely. And the second path is that the person stays at their job, and they continue to produce the minimum output. Overall, it is a negative experience for the person. They will experience depletion, irritability, fatigue, low ability to cope, and lowered morale. These are the two main paths that lead to burnout.
- Unmanageable Workload--Exhaustion--Greater Cynicism--Reduced Efficacy
- Mismatch Between Values--All Three Aspects of Burnout--Reduced Energy & Involvement--Efficacy
An unmanageable workload depletes a person's capacity to meet the demands of their job. Therapists are being asked to do too much with the same or fewer resources, and this scenario is consistent with burnout. If a therapist is dealing with an unmanageable workload, then that will lead to exhaustion and the two other components of burnout. With an unmanageable workload, it is not just the quantity of the workload, but it is also the quality of the workload. When therapists are being asked to do things outside of their scope of practice on a regular basis, it can be viewed as a strain for that therapist.
The second road is a mismatch between the values of the therapist and the organization. This can lead to all three aspects of burnout in full, reduced energy, involvement, and engagement which then can further lead to decreased self-efficacy. It can be a vicious cycle. Value conflicts and an unmanageable workload combined are the biggest contributors to burnout.
Personal factors, like personality traits and coping styles, do play a role in burnout, but they play a less critical role as noted in the empirical research. Situational and work factors play a bigger role in the development of burnout, which leads researchers to believe that burnout is regarded more like a social or group phenomenon more so than it is an individual one.
Statistics
There are a lot of stats out there on burnout in physicians and nurses, but not so much on occupational therapists. However, I did find some strong evidence that burnout is negatively impacting OTs. Forty-seven percent of occupational therapists found most days at work to be extremely stressful, and occupational therapists were ranked as the seventh most stressed healthcare providers behind nurses, medical lab technicians, specialists, and family physicians. Thirty-five percent of occupational therapists experienced high levels of emotional exhaustion, and 43% experienced high levels of cynicism.
High Work Engagement
High work engagement can quickly become work strain, secondary to work-life conflicts and health conflicts. Contrary to popular belief, burnout and engagement are not two opposite ends of a spectrum, but rather they can coexist. Engagement is independent of burnout, and although engagement has positive qualities like vigor, absorption, and dedication, an over-engaged worker can quickly shift from over-engaged to burned out.
Causes
There are many causes of burnout.
- High workload
- Low levels of psychological detachment from work during non-work hours
- Low frequency of belly-laugh
- Difficulties setting boundaries
- Low-income satisfaction
- < 10 years of experience
- Mismatch in values with the organization
- Influence of environment and context
- Funding
- Culture and broken community
- Lack of support
- Documentation demands
- Role discrepancy
- Glass ceilings
- Time demands
- Lowered morale over bureaucratic delays
- Lack of autonomy
- Unable to customize practice
- Policies and procedures of the workplace
- Juggling clinical and nonclinical duties
- Coordinating care
- Lack of respect and unfairness
I already touched upon the first one, a high workload or unmanageable workload. This can have some physical and mental health consequences. Low psychological level of detachment from work during non-work hours is another. Research has shown that psychological detachment is one of the biggest factors that contribute to recovery from work stressors, and we will get into that later on. Decreased belly laughing and difficulty setting boundaries were other factors in a study of occupational therapists and burnout. Low-income satisfaction has also been shown to be consistent with burnout. Therapists with less than 10 years of experience may not have time to fully develop coping strategies at work, or they may have lesser autonomy than those therapists that have been in the organization for long. I cannot emphasize value conflict enough. Values are the umbilical cord that connects you to your organization.
There is also the influence of the environment and context. This can play a huge role in occupational therapists' decision-making. Therapists are often asked to do more with the same or fewer resources. Having a strong community and social support can act as buffers against burnout. Decreased supervisor support can cause an employee to have decreased self-efficacy, whereas lack of co-worker and colleague support can lead an employee to feel increased exhaustion. There can be many documentation demands and different expectations depending upon the documentation systems. A role discrepancy can make a person feel purposelessness or aimless in their career. They may feel as though they are stuck which leads to the concept of a glass ceiling. Many OTS and PTs have expressed to me that they feel like they have limited ability to advance as compared to other healthcare professionals. This is also echoed in information that I have seen online. For example, there are certain roles in a healthcare setting that are only available for nurses and physicians. Many therapists feel that the only way they can move up is by opening their own practice. Many therapists do not want to do this.
There can also be time demands. Lowered morale over bureaucratic delays. In one study, many therapists reported feeling the need to constantly justify the length of treatment and their recommendations for a patient. They feel like they have a loss of autonomy. High work pressure and high work stress compared or paired with low autonomy and a low sense of control for an employee is a perfect recipe for burnout. Having low or no autonomy for therapists can cause exhaustion. It can cause increased stress and anxiety. Inability or limited ability to customize practice is another issue identified by therapists. For example, a facility may subscribe to a certain protocol or intervention, but a therapist may not feel it aligns with their vision for every patient. This type of situation can cause stress. This goes along with many policies and procedures in the workplace. Another example is a meeting that could have been an email versus a meeting. There can be many irrelevant and redundant rules that are more cumbersome to performance rather than useful. Another problem is juggling clinical and non-clinical duties. Occupational therapists, in one study, referred to this as filling the gaps. Not only are OTs responsible for clinical duties, but many times they are asked to do additional tasks like getting authorization, a prescription from the doctor, cleaning the facility, and managing the schedule. Therapists can start to feel that they are being spread too thin. The therapist's attention is constantly being diverted from clinical care. Therapists often coordinate care with other team members and help to plan discharges. If a therapist's recommendations for the length of treatment is either cut short or extended, this may cause stress.
And then lastly, there can be a lack of respect and unfairness. People value fairness in and of itself, and they see fairness as an indication of a genuine concern that an organization has for its employees. Later, we are going to get into workplace bullying and strategies to navigate that.
Outcomes
There are complex physical and mental health outcomes that result from burnout. In fact, poor health leads to burnout and burnout can contribute to poor health. There are two types of outcomes: personal and professional.
- Personal Outcomes
- Headache
- Chronic fatigue
- Gastrointestinal disorders
- Muscle tension
- Hypertension
- Cold and flu episodes
- Sleep disturbances
- Depression
- Anxiety
- Irritability
Many of the personal outcomes are related to exhaustion. What is interesting to note is that research has shown a constant, consistent relationship between burnout and insomnia. There was a study done on a Finnish population, and they found that 90% of the participants that were burnt-out also had another condition. The most common conditions were depressive symptoms and musculoskeletal pain.
- Professional Outcomes
- Job dissatisfaction
- Low organizational commitment
- Absenteeism
- Poor job performance
- Intention to leave a job
- Higher rates of turnover
- Decreased patient satisfaction
If one is experiencing burnout in the workplace, it also has negative implications for colleagues. Since burnout is regarded more as a social and group phenomenon when someone experiences burnout at work, this can be contagious and that can disrupt the work of others. Nurse burnout has been linked to decreased patient satisfaction. Additionally, nurses experiencing higher levels of burnout were judged by their patients to provide a lower level of care. The risk of patient mortality and infections were also higher when nurses had a higher patient workload and were experiencing greater burnout.
Models for Burnout
There are two models that I found to be applicable when looking at burnout in healthcare. The first one is the Model of Effort-Reward Imbalance (Figure 1). This assumes that work strain and burnout lead to an imbalance between high effort and low reward.
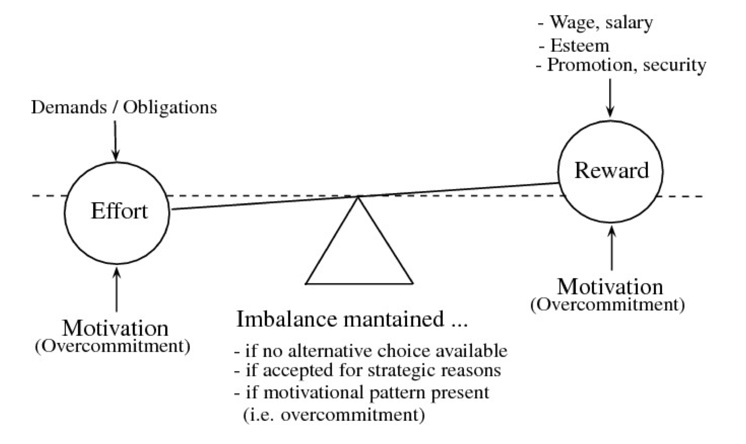
Figure 1. The Model of Effort-Reward Imbalance. (Written permission granted by Johannes Siegrist, (1996). Retrieved from: Siegrist, J. (2017). The Effort-Reward Imbalance Model. In C.L. Cooper & J. Campbell Quick (Eds.), The Handbook of stress and health: A guide to research and practice (36-56). Hoboken, NJ: Wiley Blackwell)
In this model, high effort refers to the extrinsic job demands and the internal motivation to meet these demands. Reward refers to salary, esteem, and recognition. We will get into the many types of rewards later on. When you have high effort paired with low reward, that can lead to some health consequences. Some of these consequences include increased stress, negative emotions, impaired cardiovascular health, impaired subjective health, and even mild psychiatric disorders. Overall, there is a high cost and low gain. I would like to point out that the effort can either be externally placed on the individual or it can be self-imposed on the individual. An individual that is an overachiever, or a Type A personality, can place all that effort on themselves. Regardless if the effort is externally placed or self-imposed, there can be a high cost and low gain for the employee, and there is a failed reciprocity.
The Job-Demands Resource Model, it is believed that job demands may exceed internal resources (Figure 2).
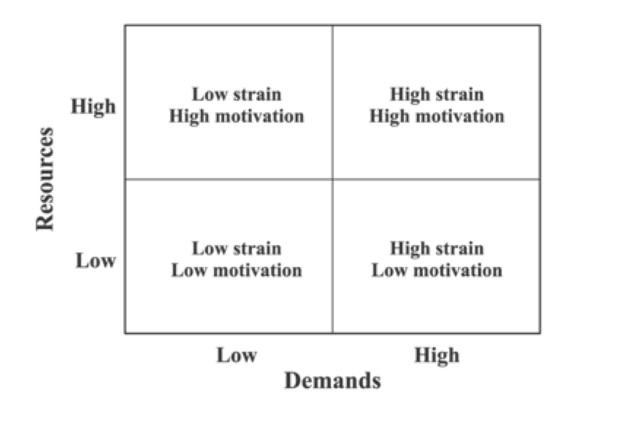
Figure 2. The Job-Demands Resource Model. (Written permission granted by Arnold Bakker. Retrieved from: Bakker, A.B., & Demerouti, E. (2006). The Job Demands-Resources Model: State of the art. Journal of Managerial Psychology; Vol. 22(3), pp. 309-328. DOI10.1108/02683940710733115
Job demands include documentation, working with patients, different tasks at work, and resources include supervisory coaching, performance feedback, and social support from coworkers. If demands exceed resources, then stress and burnout can occur. Outcomes associated with burnout, for example, are higher absenteeism and turnover. This chart depicts when you have high and low resources coupled with the low and high demands and the different outcomes that these combinations yield and how that impacts the individual.
Intrinsic Person Factors and Interventions
This questionnaire was adapted from the book, "The Stress-Proof Brain," by Melanie Greenberg. I highly recommend this book, and throughout the presentation, there are a few recommended readings sprinkled in. I like this questionnaire because, during particularly higher times of stress in your life, you can always refer back to this as a way to self-monitor where you are at, how you are dealing with stress, or how the stress is impacting you physically and mentally.
Key: Never 0; Occasionally 1; Sometimes 2; Fairly Often 3; Very Often 4
- Been upset because of an unexpected event or frustration
- Believe that you couldn’t control important life outcomes
- Felt on edge/stressed out
- Believed things weren’t going your way
- Believed that you had more to handle than you could deal with
- Felt irritable and impatient about small things
- Felt your heart racing or butterflies in your stomach
- Unable to sleep due to worrying
- Felt anxious when you woke up
- Difficulties concentrating because of your problems
Zero is never and four is very often.
The Stress-Burnout Relationship
Does stress always lead to burnout? There are several potential moderators of the stress-burnout relationship
- Successful coping strategies
- Personality variables
- Personal resources
- Job resources
- Post-work recovery from stress
Over time, chronic stress puts demands on a person's resources. The shift between stress to burnout involves a complex interplay between work stressors and insufficient recovery processes that occur during work, but also outside of work and even during sleep.
Modern Stress
What is one of the biggest causes of modern stress? The answer to that is time or lack of time. Time pressure and time scarcity significantly impact our behavior. Constantly being on the go combined with a sense of urgency can make even the most mundane of tasks pile up causing things to begin to slip like exercise or self-care.
- Getting caught up in being reactive all day
- Tension, pressure, and time constraints
- Unrealistic expectations on time and energy
- Putting up with daily hassles
- Having too much to do in too little time
- Running out of time, feeling rushed
There was a study done, in several countries, and they found that people even feel rushed during their free time. In an affluent consumer society such as the United States, there are so many competing opportunities for our time. Hence the phrase, so much to do in so little time.
