Tara: Hello, and thank you for having me. I am an occupational therapist, and I work mostly with children, who have autism or challenging behaviors, in the home, clinic, and school setting. I really enjoy talking about autism and giving tools and strategies for helping practitioners better serve individuals with autism.
What is Autism?
Autism is a spectrum disorder. One of my favorite quotes is, "If you've seen one child with autism, you've seen one child with autism." I have individuals who are non-verbal, some who never stop talking, and everything in between. A big point is that it is a brain-based disorder as their brain works differently. They use different parts of their brain for different types of information. It is not a behavior disorder. It is life long disorder with no cure. This does not mean they cannot learn and be successful individuals, but rather it means that those core characteristics of autism will affect them throughout their life.
It is evident during the first three years of life. We are going to talk in a little bit about screening tools to help identify individuals as early as possible. With it being a spectrum disorder, symptoms can range from mild to severe. I do not necessarily like the term mild or severe, because I have families who have children that we might consider "mild," but to them, it is a lot. There can be different skill levels, but I do not know necessarily that I would characterize them as mild or not.
Autism Prevalence (CDC, 2016)
One in six children have a general developmental disability. This is a lot higher than what I would have imagined. This ranges anywhere from speech to serious developmental disabilities like autism. One in 68 children have a diagnosis of autism. Every time the CDC statistics comes out, the prevalence increases. In 2007, it was one in 150. There has been a 172% increase in the '90s. These statistics are very alarming. It is distributed throughout the world in all races, nationalities, and social classes. It has no boundaries and is more common than pediatric cancer, diabetes, and AIDS combined. Some people would call this an epidemic. I think it shows that we need to do more research on autism and not necessarily as much about the cause anymore. The research is starting to look more at the best strategies and ways to support individuals, with a diagnosis of autism, and their families.
Figure 1 is a graph from the CDC on the surveillance year and how that prevalence has increased.
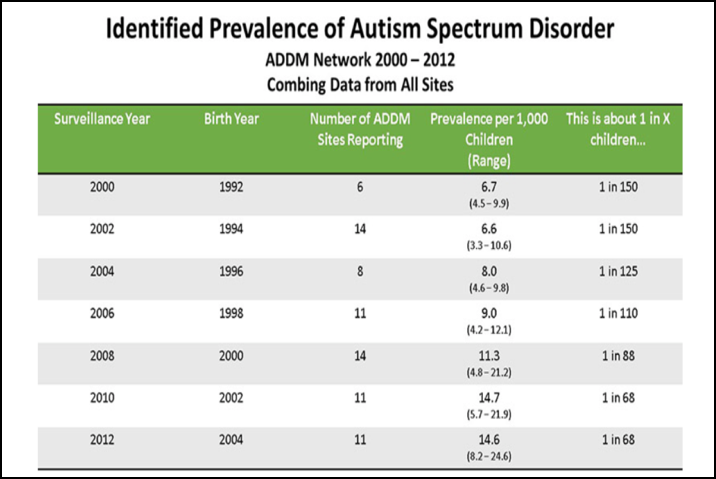
Figure 1. Prevalence of ASD.
When you look at 2000, it was one in 150. In 2012, it was one in 68. You can see by this chart how the prevalence of autism has increased.
Risk Factors
There are many risk factors for autism. There is a large range in identical twins at 36 to 95%. Fraternal twins are zero to 31%. Parents, with autism, have a risk from two to 18% of having a child with autism. Autism is more likely to occur in people with Down syndrome, fragile X, tuberous sclerosis, and other chromosomal disorders. I work with a few kids with Down syndrome who also have a diagnosis of autism. Approximately 44% of people with autism have an average to above average IQ. Thus, we cannot assume that just because an individual has autism, that they have a below average IQ. There is also a higher risk for older parents to have a child with autism. Finally, low birth weight is another risk factor for autism.
Diagnosis
You can diagnosis autism pretty reliably at age 2. We have to make sure that we are talking to families about what they should be looking for in an assessment. It is our role to make sure that parents are going to places that use the gold standard for diagnosing autism. Most kids are diagnosed after the age of four so we really want to try to get kids diagnosed as early as possible. Once a child gets to age four, they have already learned a lot of behaviors and have gotten into routines. If we can get kids diagnosed earlier, we can help them learn how to communicate and interact, thus the prognosis is much better. Most parents notice a developmental problem before their child's first birthday. There is a study where they are looking at videos from children's first birthdays to see how they are different. Some parents may miss the signs because it is their first child or they think they just have an easy baby. But looking back, they can see those signs at their first birthday. There are studies that are also going on here in Oklahoma where they are doing imaging of newborns' brains to see how their brain changes at different stages with and without autism. There is a lot of research going on to try and detect autism as early as possible to help them process information and teach them those early skills.
Costs
The CDC estimates that it costs approximately 11.5 to 60 billion dollars per year, and an average of $4,000 to 6,200 per year, per child. Annual Medicaid costs are around $10,000 per child, who has a diagnosis of autism. Behavioral interventions range from $40-60,000 per child. It is very expensive. Oklahoma finally passed insurance reform because in the past Oklahoma did not have to pay for any services for children with autism. They are now paying for those behavioral interventions, which can have a significant impact for individuals with autism. Families and schools need a lot of support. Here in Oklahoma, there is a state law that mandates that teachers up through second grade have to have two hours of autism training every other year, and for all new teachers.
Why The Increase?
Ten years ago, we were not talking about autism this much. There is a lot more awareness about it now. There are some movies and shows as well, like The Good Doctor and Parenthood. There are free tools that you can go online and use, and screenings are happening at physicians' offices at their well child checkups. There are also changes in how autism is defined according to the DSM, and we will review that in a minute. However, even after taking all these things into account, we are still uncertain about many things. We do not know why the increase is happening. We know there is some genetic and environmental influence.
What Does This Tell Us?
What does this tell us? It tells us that you are much more likely to encounter an individual with autism now than you did 10 years ago. I started working with individuals with autism 20 years ago, and the only thing anybody knew about autism was the character in the movie, Rain Man. When I would say I was an assistant for an individual with autism, they would ask, "Does he memorize everything?" Now, with the statistics being 1 in 68 kids, you are going to come across many more individuals with autism. For example, if you have 200 kids in a school, there are going to be 3-4 children with autism. It is not just our responsibility, special ed's responsibility, or the families'; we all have to know how to support individuals with autism. One of my good friends down the street has a son with autism, and he has been escaping from his house. We are going to talk about that later, but safety is a huge concern. She not only needs to know how to support her son, but the neighbors do as well. Because if he gets out of her house, they need to know how to safely get him back. This is the same in the schools. I am doing an intensive program with a school in Oklahoma, and we are not just targeting special ed teachers, but also the librarian, the bus drivers, the cafeteria workers, etc. We need to know how to support individuals who have different learning styles. It makes us much more empathetic for all different types children.
Red Flags
There are some red flags that you might see.
- Not responding to name by 12 months
- Not pointing
- Avoiding eye contact
- Delayed speech
- Upset by minor changes
- Obsessive interests
- Flapping hands
- Unusual reactions to sensory
One of the first signs is not responding to their name by 12 months. Many families think their child cannot hear. However, if you turn on the show Blues Clues two rooms over, they go running to find it. Not pointing is another red flag. Children start pointing by 12 months, with some earlier than that. When a child does not point to request something, that is concerning as pointing is social. Avoiding eye contact is another red flag. Delayed speech or odd development of speech is another. I have a friend with twins. One of the twins will not request her when he needs help by saying, "Mom!" But, he can spell all the planets at age two. In this instance, his speech is not delayed, but rather it was advanced in specific areas. There are also obsessive interests. I treated a little boy that wanted anything that would spin. He would just sit there and spin things over and over. It was an obsession that he could not stop. He wanted it all the time. There might be hand flapping or other odd motor patterns as well. Finally, they may demonstrate unusual reactions to sensory stimuli. Examples are going to the mall, getting a haircut, burshing their teeth, or taking medicine. They have a really unusual reaction to different sensory input.
Screening
The American Academy of Pediatrics recommends screening at 18 months and 24 months. Pediatricians have started to screen at well child checkups. They might point to things to see if the child will look. The will also see if the child is making eye contact and requesting things.
Identification of Autism
There are no biological markers. Individuals with autism do not look any different. It is a hidden disability. Remember, it is a brain disorder and based on behavior, history, parent interview, play conversations, play assessments, and input from others and family. The assessment tools should tap into the social and communication delays. One example of a good tool is the Autism Diagnostic Observation Schedule (ADOS). This is used to assess individuals with autism, but it also helps you better understand where their strengths and where their weaknesses are. You need to encourage families to get assessments done.
Screening Tools
Here's a list of some different screening tools for autism.
Developmental:
- Ages and Stages (ASQ)
- Communication and Symbolic Behavior Scale (CSBS)
- Parents Evaluation of Developmental Status (PEDS)
Autism specific:
- Modified Checklist for Autism in Toddlers (MCHAT)
- Screening Tool for Autism in Toddlers and young Children (STAT)
There are more developmental ones to see if the child has a delay, and then there are autism specific ones like the MCHAT and the STAT. The MCHAT is free and can be filled out with the family. It is a nice tool that outlines exactly how to do it. If the child has a certain score, then they are at higher risk for autism. You would then encourage the family to have their child get a full assessment for autism.
Diagnostic Tools
These are the tools that have the most research behind them for diagnosing autism.
- Autism Diagnosis Interview- Revised (ADI-R)
- Autism Diagnostic Observation Schedule – Generic (ADOS-G)
- Childhood Autism Rating Scale (CARS)
- Gilliam Autism Rating Scale- Second Edition (GARS-2)
The Autism Diagnosis Interview (ADI-R) is a thorough interview about development that the families fill out. That, in combination with the Autism Diagnostic Observation Schedule (ADOS-G), a play-based assessment, is the gold standard. The ADOS is very different than your typical standardized test. It is not copying a block pattern or doing a particular activity. One of the items on the test is pretending to have a birthday party. This is used to see how the child interacts. The quality of this interaction is scored. You have to go through a training to be able to test the ADOS. The Childhood Autism Rating Scale (CARS) and the Gilliam Autism Rating Scale (GARS) are two different types of rating scales. There is not as much research behind these as the ADOS and the ADI-R, but they are used a lot in the schools because there is no specific training on them, and they are a bit easier to complete.
Two Systems to Identify Autism
There are two systems used to identify autism. There is the clinical or medical diagnosis of autism. This is where we look at the DSM, or the Diagnostic Statistical Manual of Mental Disorders. We look to see if the child has the criteria set forth by the DSM-5. This has to be determined by a licensed professional, either a clinical psychologist, neuropsychologist, or a physician. Most of the time, children entering the school system already have a medical diagnosis, and they have been receiving outside services. However, I have also worked in schools, especially in rural areas, where many children do not have a clinical diagnosis of autism, but the school identifies concerns. The school can use the category of autism based on criteria from IDEA, or the Individuals with Disabilities Education Act. Students do not have to have a clinical diagnosis to qualify for school services. When you look at similarities between the two, they are more similar now than they used to be with the DSM-IV. Both include symptoms in the areas of social interactions, non-verbal communication, repetitive activities, stereotyped movements, resistance to change, and unusual sensory experiences. Both definitions indicate that symptoms need not be apparent before three and both use an umbrella classification.
Changes in Clinical Diagnosis
With the DSM-5, we now have a single classification of autism. In the past, on the DSM-IV, you could have a diagnosis of Asperger's or PDD-NOS. But now, if you meet the criteria for autism, you meet the criteria for autism. Then, we qualify that based on the level of support the individual needs. The is how the severity level is determined.
IDEA Definition
If you look at the IDEA definition of autism, it must adversely affect educational performance. Educational performance includes both academic areas (reading, math, communication, etc.) and non-academic areas (daily life activities, mobility, pre-vocational and vocational skills, social adaptation, self-help skills, etc.). It has an impact on their daily life activities. I say this because often schools say that a child does not qualify because a child's grades are good or their IQ is average. That is not what IDEA says. It is if it adversely affects their educational environment, which includes their social adaptation and self-help, these kids need support. Even if they have an average to above average IQ, they are probably missing out on social opportunities, having trouble making friends, having trouble fitting in, and finding things to do. All of this adversely affects them.
Characteristics of ASD
Let's look at the characteristics of autism. The two core areas are going to be the social interaction and repetitive behaviors. It looks at social skills, social interaction, and at repetitive behaviors.
Reciprocal Social Interactions
- Poor eye contact
- Limited range of facial expressions
- Failure to develop peer relationships
- Failure to share enjoyment with others
- Lack of social reciprocity
