Introduction
I am so excited to be here today to talk about this topic because I have been stewing about it for the last few years, and I am ready to let it out. I hope it is enlightening for each of you. We need to start with a short history lesson because we have to really establish why we care so much about occupation and why it is still relevant.
History of Occupation in Practice
- Dates back to 1700 with Philip Pinel in France
- Incorporating documents of the profession 1917
- Adolf Meyer - philosophy of occupational therapy in 1922
- Mary Reilly – Slagle lecture in 1961
- Ann Fisher – Slagle lecture in 1998
- Glen Gillen – Slagle lecture in 2013
Our understanding and appreciation for occupation date far back to the 1700s when Philip Pinel in France recognized that the process of doing was health-promoting for his patients. It generated some of the initial ideas that doing could be used therapeutically to help people return to health. Ultimately, when our original founding fathers met in 1917, they infused a lot of these ideas into the incorporating documents for AOTA, which was then the National Society for the Promotion of Occupational Therapy. The ideas that were infused back then was that there was this very reciprocal relationship between occupation and health and that if you engaged in occupation, it could improve your health. If your health was not so good, it was more difficult to engage in occupation. And, if you did not engage in occupation, this could actually decrease your health. So, these ideas have been very long-standing.
Adolf Meyer, who was involved in our profession very early on wrote the original philosophy of occupational therapy. He was a very firm believer in this connection between occupation and doing. Back in the early days, it was not just about patients cooking in the kitchen, working in the fields, or doing some housekeeping around the hospitals, but rather any type of occupation even if it was leisure. As long as it was meaningful, it could be really health-promoting. He said in the original philosophy of occupational therapy that our role consists of giving opportunities, rather than prescriptions. There must be opportunities to work, opportunities to do and to plan and create, and opportunities to learn to use the material. Very early on in our profession, it was established that occupation was a therapeutic medium. We have had several leaders throughout the history of our profession who have continued to support this idea.
One of the most famous quotes in all of the occupational therapy literature was from Mary Reilly's Slagle lecture that she delivered in 1961. She said, "Man, through the use of his hands, as energized by his mind and will, can influence the state of his own health." She was saying that the actual doing and using your hands to engage are meaningful and important.
There are other people supporting these same ideas. Ann Fisher's Slagle lecture in 1998 included, "The term occupation conveys the powerful essence of our profession, enabling people to seize, take possession of, or occupy the spaces, time, and roles of their lives. Occupation is activity that is both purposeful and meaningful to the person who engages in it." Throughout the years there have been other Slagel lectures and other really critical writings, many of which I will talk about in this lecture, that really reinforce this idea. Glenn Gillen, in his 2013 Slagle, talked about the fork in the road. "We're at this critical juncture. Which way are we going to go? Are we going to move towards occupation, or are we going to go a little bit more towards the medical model? We have to pick our path. It makes sense for us to sort of hold on to our roots because it is what makes us unique."
Defining Occupation
- “The things that people do that occupy their time and attention; meaningful, purposeful activity; the personal activities that individuals choose or need to engage in and the ways in which each individual actually experiences them” (Schell, Gillen, & Scaffa, 2014, p. 1237)
- “the everyday activities that people do as individuals, in families, and with communities, to occupy time and bring meaning and purpose to life. Occupations include things people need to, want to, and are expected to do” (World Federation of Occupational Therapists, 2019, para. 2)
To understand and dig a little bit deeper, let's look at the definitions of occupation. If you read the AOTA Practice Framework, I believe there are around eight definitions of occupation in there. They are all listed. I have chosen some of my favorites to highlight the value of occupation and how it plays out therapeutically for us. The first definition is from the Willard and Spackman book. They say that occupation includes the following definitions: "The things that people do to occupy their time and attention;" "meaningful, purposeful activity;" "the purposeful activities that individuals choose or need to engage in;" and the ways in which "each individual actually experiences them." Some of the important language in this definition, and again, this is from the Willard and Spackman book, is that occupation includes meaningful and purposeful activity. That is the key as it is not doing for the sake of doing. It is meaningful to the person that is engaging and purposeful. It is those activities that people really choose or need to engage in.
Another definition, which speaks to me, is from the World Federation of Occupational Therapists. "The everyday activities that people do as individuals in families and with communities." It really speaks to how micro or macro that engagement is. They go on to say, "Occupations include things people need to, want to, and are expected to do." Again, we see this important element about meaning and purpose. It is not doing for the sake of doing.
- “Activities . . . of everyday life, named, organized, and given value and meaning by individuals and a culture. Occupation is everything people do to occupy themselves, including looking after themselves . . . enjoying life . . . and contributing to the social and economic fabric of their communities” (Law, Polatajko, Baptiste, & Townsend, 1997, p. 32)
- “It refers to all aspects of actual human doing, being, becoming, and belonging. The practical, everyday medium of self-expression or of making or experiencing meaning, occupation is the activist element of human existence whether occupations are contemplative, reflective, and meditative or action based” (Wilcock & Townsend, 2014, p. 542)
Here are a couple more definitions that I really like. This is one of my favorites from our neighbors to the north in Canada. They define occupation as "Activities of everyday life, named, organized, and given value and meaning by individuals in a culture. Occupation is everything people do to occupy themselves, including looking after themselves, enjoying life, and contributing to the social and economic fabric of their communities." Again, in this definition, we are getting back into the value and meaning of occupation. This is a critical piece of how we define occupation. The bottom half of this definition, by the way, speaks to how the Canadians classify their occupations as self-care, leisure, and productivity.
Finally, a couple of theorists who I really respect, Ann Wilcock and Liz Townsend, state that "It refers to all aspects of actual human doing, being, becoming, and belonging. The practical everyday medium of self-expression or of making or experiencing meaning. Occupation is the activist element of human existence whether occupations are contemplative, reflective and meditative, or action-based." We have ideas about meaning and purpose, and there is some active engagement. These are some common threads in how we are defining occupation and some important elements. It is important to recognize what that is, be able to have a strong, confident definition, and have an appreciation for what occupation is. I tell my students that occupation is our secret sauce. It is what makes us different and unique relative to all of the other professions that are out there providing healthcare. We need to be able to express that unique perspective and unique value.
- ...“the therapeutic use of everyday life activities (occupations) with individuals or groups for the purpose of enhancing or enabling participation in roles, habits, and routines in the home, school, workplace, community, and other settings” AOTA, 2014, p. S1)
Not only is it a good idea to help explain what we do, but according to AOTA when they define occupational therapy, they point out at the very beginning of the definition of what occupational therapy is. "The therapeutic use of everyday life activities or occupations with individuals or groups for the purpose of enhancing or enabling participation in roles, habits, and routines." The early part of this definition is critical. This definition comes from the Occupational Therapy Practice Framework. It is important to note this because that document is written and explained so clearly for the purpose of outside readers, people like healthcare administrators and third-party payers. They will look at this document and they will say, "What is occupational therapy?" "What are the occupational therapists working in my healthcare facility?" Or, "What services am I paying for?" If a third-party payer reads this definition, it is their expectation that this professional is using occupation as their therapeutic medium. It is really important that we recognize the importance of how other people recognize occupation as well.
Therapeutic Approaches
How do we do this? It has been laid out and defined. There is an expectation that we are using occupation in practice. But, what does really that look like? There are several terms that are out there, some of which are used interchangeably. I want to point some of them because it will help us to wrap our heads around what our expectations are and also what is realistic.
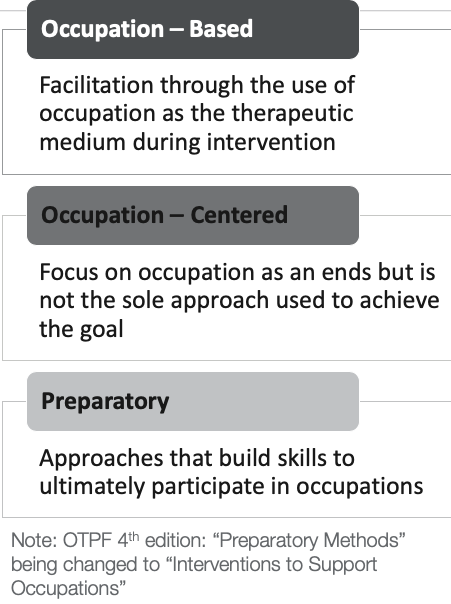
Figure 1. Therapeutic approaches.
The very first definition is occupation-based. This is the highest complete concentration of occupation used. This is when we are facilitating therapy through the use of only occupation as a therapeutic medium during intervention. I would consider occupation as sort of the Holy Grail. It is like a vision statement. This is a place where you want to get, but it is not likely that any of us will ever get there where we are only using occupation as our therapeutic medium. It is not very realistic. The other side of that spectrum (down to the bottom) is preparatory. Those are approaches that build skills to ultimately participate in occupation. The reason why we cannot only use occupation-based approaches is that sometimes we have to do preparatory work like a person's balance, strength, coordination, or cognition. We are working on those individual skills because they are not ready to do the occupation-based activities. Now, I am going to jump back into the middle now because this is a mixture of these approaches. This is where I have a focus on occupation as my end goal. It is not the sole approach that I use to achieve my goal. Occupation-centered is really the most realistic, and it is achievable by all of us. We are thinking about occupation as our end goal. Hopefully, we are also using some occupation as a therapeutic medium, but this is sort of a continuum. I do not know if any of you have read the proposed fourth edition of the OT Practice Framework. They will be voting on it in the spring at the next representative assembly meeting at the conference. The term preparatory methods are actually being replaced with "interventions to support occupations." That term preparatory will not be part of our lexicon anymore if they approve it.
How Occupation is Infused into Practice
- Activities holding personal meaning, and cultural and developmental relevance to the individual facilitates treatment of the “physical, cognitive, and psychosocial components of performance” (p. 358)
- To keep occupation at the center of practice, practitioners must infuse occupation into the therapeutic process
- Occupation as a means - incorporating occupation into the intervention
- Occupation as ends - the overarching goal of OT intervention
(McLaughlin Gray, 1998)
Julie McLaughlin Gray wrote in 1998 about how occupation is infused in practice. She acknowledged that anytime we use activities that hold meaning and cultural and developmental relevance to the client that facilitates our treatment and improvement. We should be using approaches and activities that are personally meaningful and culturally and developmentally relevant. She also states that we should keep occupation at the center of practice and that we should be infusing occupation into our therapeutic process. There are two real ways to do that. One is to use occupation as a means. So, we are incorporating occupation into the intervention. It is our therapeutic medium. It is the means to achieve our goals and also occupation as an end. My end goal is to support engagement and occupation. I might have to use several different approaches to get there, but occupation is always on our minds. It is lovely that we recognize the meaning and value of occupation, but we should not use occupation just because we have done it for a long time. We should be using occupation in practice because it works, and it is very effective at generating positive health outcomes.
Values of Occupation in Practice
- Participation in occupation has positive health and quality of life outcomes for older adults (Stav, Hallenenen, Lane, & Arbesman, 2012)
- Occupation-centered interventions yield:
- Better outcomes in those with mental illness (D’Amico, Jaffe, & Gardner, 2018)
- Reduced decline, improved performance, and enhanced behaviors among those with dementia (Smallfield & Heckenlaible, 2017)
- Social and emotional skills for children at Tier 1, universal, whole population level (Arbesman, Bazyk, & Nochajski, 2013)
- Improved cognitive performance after stroke (Gillen, Nilsen, Attridege, Banakos, Morgan, Winterbottom, & York, 2014).
I did a very really brief search of AOTA's evidence-based practice resources and systematic reviews. This is just a sampling from a very quick, 10-minute search of all the studies that recognize this link between occupation and positive health outcomes. The first systematic review looked not at occupation in a healthcare situation, but rather it looked at participation in occupations and activities among community-dwelling older adults. That systematic review had 99 articles and looked at a range of occupational engagement, religious activities, social participation, exercise, cognitive gains, et cetera. It also looked at a range of health outcomes including mortality rates, the use of healthcare resources, and progressions in dementia and depressive symptoms. In these 99 articles, all of them showed that by engaging in occupation there were positive health outcomes for every area of occupation except for caregiving. They found that the occupation of caregiving to be detrimental to your health. This is not child-rearing, but caregiving for an aging or ill spouse.
Other studies were done looking specifically at people receiving occupation-centered interventions that spanned multiple populations. With the mental health population, they found that using occupations in practice generated better outcomes. In folks who have dementia, they found that using occupation in practice reduced their cognitive decline, improved their performance, and enhanced their behavior. Similar findings were in the pediatric study with improved social and emotional skills when using occupations at Tier 1, universal, and whole population level. Thus, using occupation can have a more global outcome as well. The last one I am including was a study following stroke interventions. This found that occupation-centered interventions improved cognitive performance. Again, I am only highlighting those I found in a quick search. There are many other studies that support the value of occupation.
Current State of Occupation in Practice
- Occupational therapy has shifted to more medical-model based practice
- Barriers
- Limited equipment
- High productivity demands
- Time constraints
- Facility generated goals
- Physician orders
- Insurance companies
- Limited space (Che Daud, Judd, Yau, & Barnett, 2016)
- Lack of education and professional development
- Client opposition to occupation-centered care (Colaianni & Provident, 2010)
- Client acuity
Now that we have established what occupation is and how we can use it in practice, we have to take a step back and look a little bit at the reality. As a profession, we are really shifting more towards a medical model-based practice. This is true in other countries as well, not just in the United States. There have been some studies done as to why this is. One study that was done by Che Daud, Judd, Yau and Barnett (2016) stated that there were issues with limited equipment. The therapist did not have the appropriate materials needed to be able to execute occupation-based practice. Another barrier noted was high productivity demands. "My rehab manager expects me to be productive and it is just too difficult within the time constraints that I have." Sometimes people said that their facility dictated what their goals were. Often, in electronic medical records, there is a pulldown menu and a list of specific goals. This limits the therapist's ability to be client-centered and look at specific occupations. Physician orders were also a problem. Sometimes the insurance companies dictated what you could or could not do. Space was also a big issue and can limit participation in some occupations. Colaianni and Provident (2010) found barriers to be a lack of education and professional development. Therapists did not feel comfortable or trained in the use of occupations. Finally, there was some client opposition to occupation-centered care. The clients recognized exercise as being what was really important.
My colleagues and I did a couple of clinic makeover studies in an effort to try to increase the use of occupation-based practice. We went into a clinic and put away the weighted dowels, Theraband, putty, hand bike, and the range of motion arc. Instead, we brought in about $1500 worth of occupation-based materials. While in theory, this should have been really great, however, there were some issues. One of the barriers was this overwhelming culture of exercise and what therapists were accustomed to doing. They were sharing a gym with PT, and they actually felt like they were not doing as good a job because they were not doing exercises with their clients. We were using the FIM as our outcome measure, but the FIM was not sensitive enough to pick up on improvements. Therapists also said they did not really know what to do or how to document it. For a different study, we did something very similar, but we added an education piece to train the therapist on how to select the different occupations and how to document it. In this second study, we ran into pretty big issues as the landscape of healthcare is changing and patients with worsening acuity are coming into healthcare facilities and traveling out to the next level of care pretty quickly. The client acuity levels were so high that they just were not able to engage in occupation.
These studies show that there are lots of reasons why therapists might get stuck or have difficulty using occupation in practice.
Constructs of Occupation-Based Practice
Where do we go from here? A colleague of mine created this theory about occupation-based practice as seen in Figure 2.
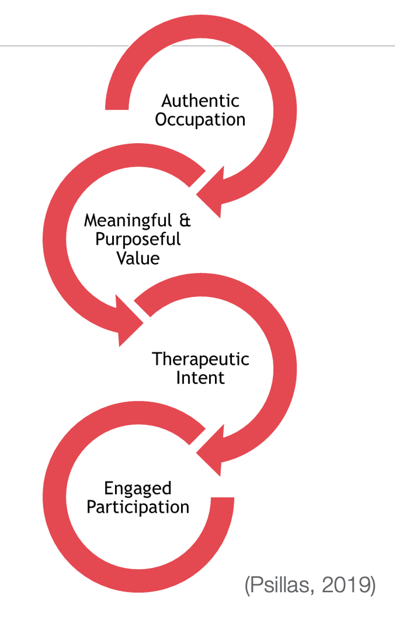
Figure 2. Occupation-based practice theory.
Remember, earlier on I talked about occupation-based as using only occupations. There are four constructs that were identified to help us to get there. They are authentic occupation, meaningful and purposeful value, therapeutic intent, and engaged participation.
Authentic Occupation
- Actual doing vs. simulated performance
- Use actual occupation items vs simulated materials or gesturing
- Performed in a context consistent with the occupation
The first construct is authentic occupation. This means that what you are doing should be an actual occupation versus a simulated performance. Ideally, you are using the materials and the items that are consistent with that occupation, not simulated materials or gesturing. So if you are working on brushing your hair, you use a hairbrush. And, the context in which it is performed should be consistent with the occupation. I want to share an example of a client who has a distal radius fracture with decreased pronation. I could choose an exercise like Figure 3 and put a weight in her hand to allow gravity to pull down on her forearm and increase her pronation.

Figure 3. Using a weight to increase pronation.
I might achieve my goal of increasing her pronation, but I really need to ask myself, "Is this an occupation?" The answer is no. The materials and context are not consistent with an occupation. We could take this up a notch and do something like have a person pour beads from one container into another as seen in Figure 4.

Figure 4. Pouring beads from one container to another to increase pronation.
Again, I am getting that increased forearm pronation. However, is this a real or simulated activity? Are there materials or items associated with the occupation? At this point, we cannot even identify what the occupation is. Pouring beads from one bucket into another is not really an occupation. If I take it to the next level, we have somebody repotting an orchid in Figure 5.

Figure 5. Repotting a plant.
We are again seeing that great forearm pronation in that right arm. In this scenario, there is actual doing. This person is pouring dirt to repot a plant as part of an authentic occupation. Are there materials being used? Are they consistent with the occupation? There is a plant, a pot, and dirt. The context is not perfect because we are still in a therapy clinic. Ideally, if I want authentic occupation to be fully realized, we would be outside in a garden or using a raised flower bed. This example shows how I can bring an authentic occupation into therapy and add meaning and purpose. This brings me to the next construct which is meaningful and purposeful value.
Meaningful and Purposeful Value
- Client identifies the meaning vs therapist chosen
- Creation of item or execution of task vs exercise
- Associated with client-stated goal
In this construct, the client identifies the meaning. This is in contrast to the therapist choosing the activity or convincing the client that it is important. It has some purpose. The person is either creating something or executing a task versus just carrying out an exercise. Finally, what is being done should be associated with the client's goal.
Let's walk through another case to illustrate these points. In Figure 6, this person has a brain injury and they are working on isolated finger control with Theraputty exercises.

Figure 6. Theraputty exercises.
Is this meaningful to the client? Probably not. Is the person creating an item or executing a task? No, they are just doing an exercise. Is this associated with the client's goal? It probably is because they are isolating their thumb and fingers and that is a part of their goal. However, I could make it a little bit more purposeful. I could pull up a very simplistic game on a phone (Figure 7) and the person could isolate digit movement by playing that game. Is this meaningful to the client? Did they identify with this?

Figure 7. Simplistic game on phone.
This is probably not meaningful as this is an adult client. Is the person executing a task or creating an item? They are playing a game and moving her thumb and digits so the part of the goal is being met. I can take it a step further and have my client engaged in a meaningful, competitive game with the therapist. Now does the client identify meaning? If the client chose the app and this is a game that they enjoy playing, then yes, the client generated that meaning.
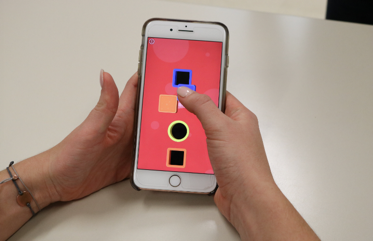
Figure 8. Adult game that is meaningful to the client.
Is there an execution of a task? Yes, because she is actually playing a game and getting authentic finger movements.
Therapeutic Intent
- Addresses skill or occupation in need of development
- Addresses relative weakness
- Therapeutically beneficial
The next construct is therapeutic intent. This means that you are addressing the skill or the occupation in need of development, rather than doing something else that is not related. You should be addressing a relative weakness, and it should be therapeutically beneficial. An example of this would be all the folks with different diagnoses and different skill levels lined up doing weighted dowel exercises in a skilled nursing facility. I have also seen people sitting in wheelchairs with their lower extremity elevated because of some orthopedic injury working on a puzzle. We have to be really careful that we are filling in therapy minutes with something that is intentionally therapeutic. Let me give another scenario. This is a client with impaired balance. One option is the person could play cards (Figure 9).

Figure 9. Playing cards.
Is this what the person needs to work on? It would fill some time, but it is not therapeutically beneficial. I could have somebody working in standing as in Figure 10.

Figure 10. Working on an activity in standing.
Or, I have a client playing a video game using the Xbox Connect where he has to move around, duck, step, and jump (Figure 11). Now, I am really working on impaired balance.

Figure 11. Working on balance with an Xbox Connect.
This is very intentionally therapeutic.
Engaged Participation
- Actively Engaged
- Coaxed or Intermittent Participation
- Passive
Finally, the last construct is engaged participation. This has to do with how actively engaged my client is. The reality is there are some interventions that just are passive. If we think about physical agent modalities, coma stim, or scar massage, these are things that the client passively receives. It is not ideal, and hopefully, you are doing some other things where there can be more active engagement. This is the final construct that helps us be more occupation-based. In this last scenario, a therapist is providing patient education about infant massage. In the first image, the mom is sitting there while the therapist demonstrates the infant massage (Figure 12).

Figure 12. Mom in a passive role while the therapist demonstrates infant massage.
In Figure 13, the mom is beginning to be more involved in the activity.

In Figure 12. the therapist is convincing the mom to engage and do some of the therapy.
At the highest level, our client is really actively engaged. The mom is doing the massage and the therapist is looking on approvingly (Figure 13).

Figure 13. Mom is completing the task while the therapist supervises.
These are the four constructs that you can use to figure out how occupation-based you are. Let's say you are working in a skilled nursing facility or inpatient rehab and it is in the morning. You go to the client's room and the first thing you do is transfer them from their bed to the wheelchair so you are providing some functional mobility training. This is the first therapeutic interaction you do. Then, you go down to the gym and their sitting balance is not great so you do some sitting balance exercises. This is another therapeutic interaction. And then because you need to work on balance, you could also work on lower body dressing using a dressing stick or a long-handled shoehorn. Training in adaptive dressing is a third therapeutic interaction. Lastly, you might provide some education about hip precautions. So, in that one therapy session, you have completed four different therapeutic interactions. Each one of these interactions can be viewed using this framework. For example, let's look at adaptive dressing. One, is it an actual occupation? The answer is yes. Is it meaningful to my client? If they said they want to be independent in dressing, then yes, it is. Is it intentionally therapeutic? If their goal is to be able to dress independently and I am working with them on dressing, then that activity it intentionally therapeutic. Finally, am I engaging my client? Are they the ones doing the dressing? In this instance, you are occupation-based even though something else that you did like the functional mobility may not be as occupation-based. We need to look collectively at our practice knowing that sometimes we might use a hot pack or have them do exercises. We need to look at our practice as a whole.
Assessing Your Own Practice
- Consider each therapeutic interaction in a session
- Functional mobility
- Sitting balance exercises
- Adaptive dressing
- Education to observe hip precautions
- Think about a single interaction and ask yourself:
- Is it an actual occupation?
- Is it meaningful to my client?
- Is it intentionally therapeutic?
- Am I engaging my client?
There is a practice spectrum. Starting at the medical model side where activities are not in an appropriate context, the materials are not related to an occupation, and the activity is dictated and lead and run by the therapist. This is a more passive approach. In contrast, on the other end, the participant is involved and the treatment is occupation-based.

Figure 14. Treatment spectrum.
Occupation-based treatment is where we want to get to eventually, although we may not ever get there all the time. Most of us exist somewhere here in the middle. The purpose of today's talk is to be conscious about moving toward the right side of the spectrum. If we stay too far on the left using activities aligned with the medical model, there is a chance that a third-party payer might say, "Is that occupational therapy? It could just be any other discipline."
Tips to Enhance Practice with Occupation
- Administer an occupational profile on each client
- Identify occupations commonly engaged in by the clientele
- Create occupation “kits”
- Plan ahead
How do we get there? How do we make our practice even more occupation-centered? There are several things you can do. We need to consider where we want to end up so we can figure out where to start. Stephen Covey, who wrote "The Seven Habits of Highly Effective People", states that one of his habits is to begin with the end in mind. If the end for me is to help support a child's occupational engagement, then I have to find out what occupations to work on. I need to figure out who they are as an occupational being and their occupational goals are. The first step can be as simple as administering an occupational profile on each client to discover what occupations are meaningful to them. Another thing I can do is to think globally and identify occupations that are commonly engaged in by the clientele in my area of the country or world. Certainly, in different areas of the country, there will be some different interests. For instance, if I am located in a retirement community in Palm Beach County, Florida, many people golf. This is an occupation commonly engaged in by the population in this area. Thus, I might want to make sure that I have materials in my clinic to simulate golf activities because I know that will be meaningful to my clients. Another example might be skiing simulation activities if I am treating in the mountains of Colorado. This might be accomplished via a video game like a Wii or an Xbox Connect. You want to identify what people engage in so you know what equipment and materials to get. You can then create occupation kits. The two pictures depicted in Figure 15 are pictures from our first clinic makeover study.

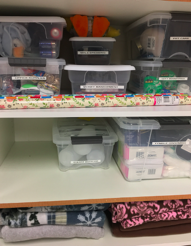
Figure 15. Clinic makeover pictures.
You can see that on the left there is a laundry station. We had the ironing board, the iron, laundry baskets, clothespins, and clothes hangers all gathered in one area. We also had a rope that we strung up so people could hang up laundry. We also put together several little kits like one for women's grooming, money management, pet care, and gift wrapping. We had several different kits that we created, and we labeled each bin.
Professional Goal Setting
- How can you change your practice?
- Tomorrow?
- One month from now?
- How can you change practice beyond you, extending to your clinic or facility?
I want you to think about what you are going to do to change your practice. I am going to share some of the responses from our live audience.
- Using actual classwork from the student's teachers in our sessions. That's a great idea. In this way, you are not choosing an activity just for the sake of it. They have to do that classwork anyway so why not do something that is meaningful to them. This can also be productive and helpful to that child.
- I would like to offer cooking kits. Cooking kits are a great idea. When we did our clinic makeover, we went to Walmart and bought five shopping carts full of things. We also worked with dietary to make sure that we were always stocked with eggs, bread, butter, and cheese. We also bought pudding mixes and cans of soup. This allowed us to have the staples for simple meals. You can actually save money by getting some of the food from dietary as well.
- I like a rolling pin to roll out putty for cooking. If you are rolling out putty like cookie dough, that is a simulated task. What would take that up to the next level is actual dough. You can even buy the refrigerated cookie dough. This can provide extra sensory feedback from the smell and texture. There has also been research about that extra olfactory sense adding a little bit more authenticity to the movements, and it is also the right consistency for rolling.
- Some facilities have washing machines and patients do their own weekly laundry. It does not get more purposeful than that. Having people do their own laundry is fantastic.
Many other things that people mentioned were materials that you would want to bring into the clinic. I would say a great way to make that happen is by using your students and really challenging them to create occupation-based kits that are appropriate for the clients in your setting. This might be an assignment they have to do for school. If it is something really specific to a client, I have found that family members are happy to bring in supplies. Examples include quilting supplies or a fishing pole and tackle box. Clients also like to engage in those meaningful occupations associated with the holidays. You can have people make decorations, make certain holiday foods, or wrap presents.
The most important thing is to be intentional. Ask the person what is important to you? We all have those folks that say, "I want to walk," when you ask them about their goals. That is great, but what else do they want to do? One of the most ideal settings is in-home care because you have all the materials, you have the space, and it is the most realistic context that you possibly could conjure.
In summary, we want to start off by asking the right questions and having the materials that we need. What can do beyond your personal practice that might affect everybody in your clinic or everybody in your facility? How do you make that change happen? System change may be more about changing the documentation system or changing policies. However, you might be able to take some small steps by adding in the kits or by starting to use occupation-based assessments, like the Canadian Occupational Performance Measure or again the Occupational Profile. We really need to get involved to make systemic changes.
Acknowledgments
- Photography credit: Erica Smedberg
- Models:
- Gabriela Cesarino
- Brian Sheeran
- Erica Smedberg
- Theresa Tveit
- Melanie Vlasic
- Arno Van Vuuren
- Kendall Webb
I want to acknowledge the folks in the pictures. They are actually my students. Most of them served as models, and one was a very excellent photographer.
References
Some of my real favorite readings are in this reference list. Many of these strong philosophical ideas are what shape the way that I think.
American Occupational Therapy Association. (2014). Occupational therapy practice framework: Domain and process (3rd ed). American Journal of Occupational Therapy, 68, S1-S48. doi:http://dx.doi.org/10.5014/ajot.2014.682006
Arbesman, M., Bazyk, S., & Nochajski, S. M. (2013). Systematic review of occupational therapy and mental health promotion, prevention, and intervention for children and youth. American Journal of Occupational Therapy, 67, e120–e130. http:// dx.doi.org/10.5014/ajot.2013.008359
Che Daud, A. Z., Judd, J., Yau, M., & Barnett, F. (2016). Issue in applying occupation-based intervention in clinical practice: A delphi study. Procedia-Social and Behavioral Sciences, 222, 272-282. https://doi.org/10.1016/j.sbspro.2016.05.158
Colaianni, D., Provident, I., DiBartola, L. M., & Wheeler, S. (2015). A phenomenology of occupation-based hand therapy. Australian Occupational Therapy Journal, 62(3), 177-186. doi:10.1111/1440-1630.12192
Gillen, G. (2013). A fork in the road: An occupational hazard? American Journal of Occupational Therapy, 67, 641-652. doi: 10.5014/ajot.2013.676002
Gillen, G., Nilsen, D. M., Attridge, J., Banakos, E., Morgan, M., Winterbottom, L., & York, W. (2015). Effectiveness of interventions to improve occupational performance of people with cognitive impairments after stroke: An evidence-based review. American Journal of Occupational Therapy, 69, 6901180040. http://dx.doi.org/10.5014/ajot.2015.012138
Gray, J. M. (1998). Putting occupation into practice: occupation as ends, occupation as means. American Journal of Occupational Therapy, 52, 354-364.
Law, M., Polatajko, H., Baptiste, S., & Townsend, E. (1997). Core concepts of occupational therapy. In E. Townsend (Ed.), Enabling Occupation: An Occupational Therapy Perspective. Ottawa, ON: CAOT Publications ACE.
Meyer, A. (1922). The philosophy of occupational therapy. Archives of Occupational Therapy, 1, 1-10.
Smallfield, S., & Heckenlaible, C. (2017). Effectiveness of occupational therapy interventions to enhance occupational performance for adults with Alzheimer’s disease and related major neurocognitive disorders: A systematic review. American Journal of Occupational Therapy, 71, 7105180010. https://doi.org/10.5014/ajot.2017.024752
Psillas, S. (2019). Occupation-based practice in occupational therapy. (Unpublished doctoral dissertation). Nova Southeastern University, Ft. Lauderdale, Florida.
Reilly, M. (1962). Occupational Therapy can be one of the great ideas of 20th medicine: 1962 Eleanor Clark Slagle Lecture. American Journal of Occupational Therapy, 16, 2-9.
Schell, B. A. B., Gillen, G., Scaffa, M. E. (Eds.) (2014). Willard and Spackman’s occupational therapy (12th ed.). Philadelphia: Lippincott Williams & Wilkins.
WFOT. (2019). About occupational therapy. Retrieved from https://www.wfot.org/about-occupational-therapy
Wilcock, A. A., & Townsend, E. (2014). Occupational justice. In B. A. B. Shell, G. Gillen, & M. E. Scaffa (Eds.), Willard and Spackman’s occupational therapy (pp. 541-552). Philadelphia, PA: Lippincott Williams & Wilkins.
Citation
Stav, W. (2020). Occupation-centered practice. OccupationalTherapy.com, Article 5085. Retrieved from http://OccupationalTherapy.com
