Editor's note: This text-based course is a transcript of the webinar, An Occupational Therapist's Perspective On Visual Deficits in Pediatrics, presented by Subah Gupta, MHS, OTR/L, SCLV, CBIS.
Learning Outcomes
- After this course, participants will be able to list the common conditions where visual deficits are encountered.
- After this course, participants will be able to describe screening for visual deficits in pediatrics.
- After this course, participants will be able to list appropriate intervention strategies for children with visual deficits towards independence in play and academic performance.
Introduction
Thanks to all of you today for taking the time to attend this presentation. I developed an interest in vision very early on. As occupational therapists, we often work with visual perceptual and integration disorders. Visual perception is the ability to interpret information as we see it, whereas the ability to act on these skills is visual-motor skills.
Over the years, I realized that there is more to it, and this is what we will be talking about today. I like to call these the foundation skills for vision. I am also hoping today to draw a line in the sand between optometry and occupational therapy to show how we are different, how we are alike, and how we can work with each other for the child's benefit.
Anatomy of the Eye
Let's briefly review the anatomy, as seen in Figure 1.
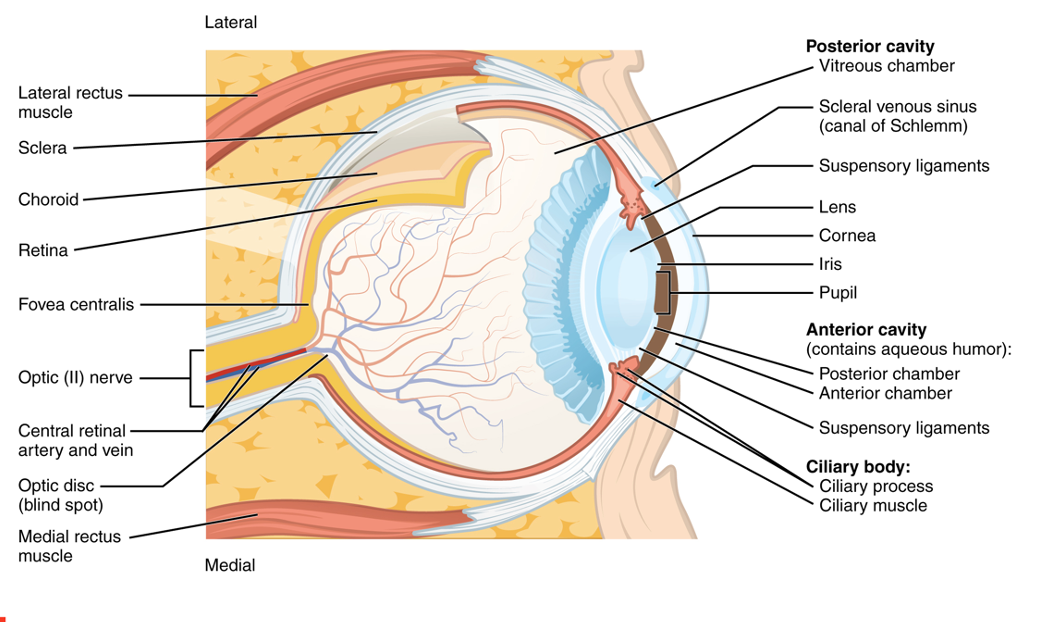
Figure 1. Anatomy of the eye. For an enlarged view, click here.
For today's presentation, we are primarily interested in the lens and the cornea in the front and the fovea (part of the retina) in the rear of the eye. The optic nerve leads from the fovea and takes the information or the image that we see to the brain.
Diagnoses Commonly Associated with Visual Disturbances
- Autism Spectrum Disorder
- Cortical Visual Impairment
- Optic Nerve Hypoplasia
- Ocular Albinism
- Down Syndrome
- Duane Syndrome
- Cerebral Palsy
- Retinopathy of Prematurity
- Low birth weight
- Concussions and Head Injury
- Spina Bifida
- Retinoblastoma
Here are some of the diagnoses that are commonly associated with visual disturbances.
Cortical Visual Impairment (CVI)
- Most common "low vision" diagnosis in children.
- Perinatal injury to visual processing structures (visual cortex with calcarine fissure) and pathways (optic radiation).
- The structures within the eye and optic nerve are not affected.
- It is a neurological impairment where it creates a "Swiss cheese effect."
- Decreased visual acuity ranging from mild to moderate impairment, visual field deficits, reduced contrast sensitivity function, and oculomotor abnormalities are also commonly present.
- Functional vision may improve with time (developmental neuroplasticity).
Cortical visual impairment is a common low vision diagnosis in children caused typically by a perinatal hypoxic-ischemic injury. Interestingly, the eye and the optic nerve structures are not affected. Instead, the optic tracts transfer the information from the eye to the brain and the visual cortex. Another interesting thing with CVI is that vision improves with time due to developmental neuroplasticity.
Refractive Errors
- Myopia
- Hyperopia
- Astigmatism
Let's now talk about some of the refractive errors.
Myopia (Nearsightedness)
- Light rays entering the eye focus in front of the retina
- Good vision for near, poor for distance
- Children adjust the reading distance either by moving closer to the object or squinting.
- Myopia is unusual for normally developing infants and preschool children.
- Many elementary school-aged children are now being diagnosed with myopia because of environmental factors (usually in 2nd or 3rd grade).
Myopia is nearsightedness, and as the name says, you can see well near, but there is difficulty seeing far. The light rays entering the eyes focus in front of the retina. If a child comes close to the blackboard to see what is written or squints to see things far away, they are probably myopic.
Hyperopia (Farsightedness)
- Light rays entering the eyes focus behind the retina.
- Vision is good for far but poor for near.
- Accommodation is by the contraction of the ciliary muscle, and small degrees can be successfully overcome. The child may pass a typical vision screen.
- Low to moderate degrees of hyperopia (1 to 3D) will have a significant effect on the child. The child tries to accommodate, which leads to eye strain, inability to attend and concentrate, headaches, and blurred vision.
- Many times excessive effort will lead the eye to turn in and lead to blurred vision.
Hyperopia, on the other hand, is the exact opposite. This is when light rays entering the eyes focus behind the retina. Thus, the individual's vision is good for distant objects but not for near. To accommodate, they contract the ciliary muscle, causing the eye lens to bulge and thicken. This can cause headaches, an inability to concentrate, and blurred vision.
Astigmatism
- The smoothness of the cornea is affected.
- Vision is blurred and distorted at both distance and near as light rays are unevenly refracted.
- Babies can be born with it.
Another one that we see is astigmatism, where the smoothness of the cornea is affected. Vision is blurred at near and far distances.
Muscles of the Eye
- There are 6 extraocular muscles.
- The superior, medial, inferior rectus, and inferior oblique are innervated by the third cranial nerve (oculomotor).
- The superior oblique is innervated by the fourth cranial nerve (trochlear).
- The lateral rectus is innervated by the sixth cranial nerve (abducens).
Three cranial nerves innervate six extraocular muscles (Figure 2).
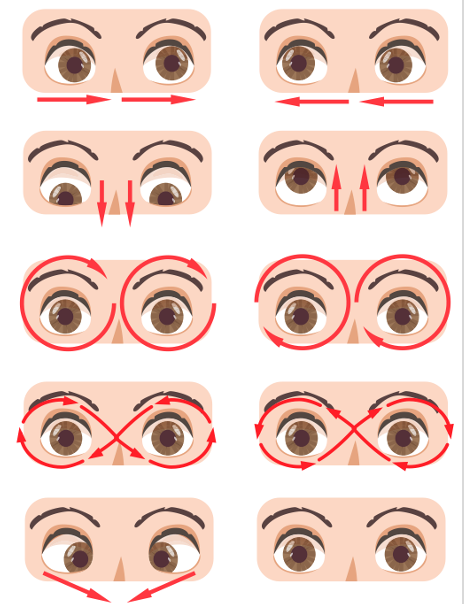
Figure 2. Muscles that Control Eye Movement. This work by Cenveo is licensed under a Creative Commons Attribution 3.0 United States.
The three cranial nerves exert control. If that control is adequate and the muscles have good strength, there will be efficient and accurate movement of the eyes, as seen in the pictures on the right in Figure 2. However, if the cranial nerves are involved, whether due to an aneurysm, stroke, head trauma, or a congenital disinnervation disorder, this may cause visual efficiency.
Visual Efficiency Disorders
- Ocular Motility Skills
- Saccadic Dysfunction
- Difficulty re-fixating eyes from one point of fixation in the visual field to another
- Dysfunctional movement is missing a target and/or over or undershooting the target.
- Pursuit Dysfunction
- Difficulty keeping eyes fixed on a moving target
- Dysfunctional movement is overshooting, undershooting, loss of target, random eye movement, eyes widening, and excessive head movements.
- Nystagmus
- Rhythmic involuntary movements of the eye
- Binocular Vision
- This refers to information processed from each eye. The images need to be the same size, detail, and form.
Ocular Motility
When we talk about visual efficiency, we refer to saccadic and pursuit eye movements. Saccades are the mind movements that change the line of sight from one object to another that catches our attention. These are rapid vital movements. On the other hand, pursuits are the ability of the eye to maintain a fixed image on moving targets. The speed of the moving target is what is matched by our eye to have that fixed image. If there is a deficit in the saccadic eye movement, there is difficulty with re-fixating eyes, and the child will over or undershoot. We will talk about this in a little bit more detail in a bit.
With pursuits, there are going to be many targets. With a visual efficiency disorder, a person may have excessive head movements, eye-widening, and random eye movements because they have lost the target and now are trying to find where it is. Nystagmus is a rhythmic, involuntary movement of the eye when the eyes have lost fixation. This is easily seen.
Binocularity is a slightly different term where the information processed from each eye needs to be the same in size, detail, and form. We have two eyes, but the image should always be one. When the eyes are not teaming, we get double vision.
Binocular Vision Disorder
When the eyes are not teaming, they can present, as seen in Figure 3.
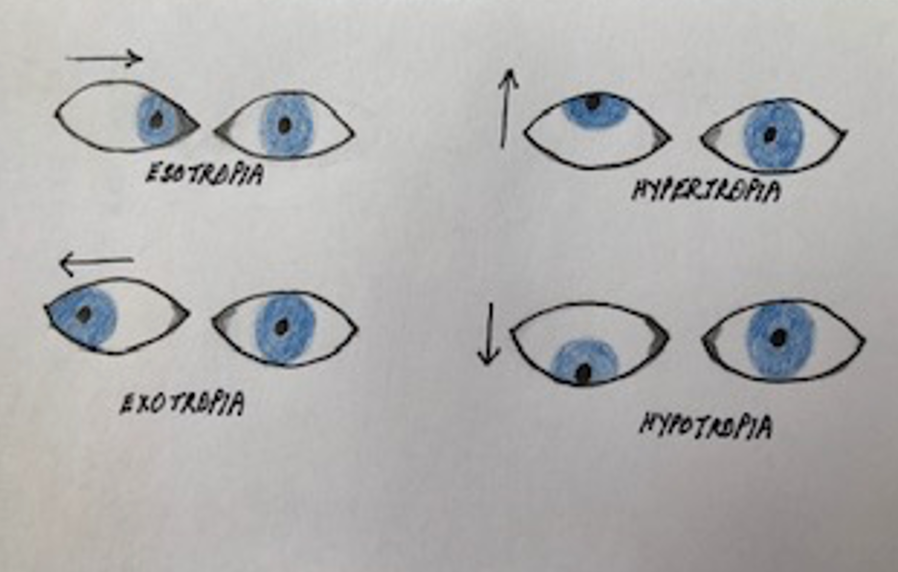
Figure 3. Examples of things that happen with binocular vision disorders.
The eyes can move inward, so the eyeball is towards the nose called esotropia. Exotropia is where the eyeball moves away from the nose. Hypertropia is where the eyeball is up, and hypotropia is where the eyeball is down. There can be a slight difference in terminology, but it has a substantial functional impact.
- Strabismus Disorder
- Exotropia – Eyes turn out
- Esotropia – Eyes turn in
- Hypertropia – Eyes turn up
- Hypotropia - Eyes turn down
- Non-strabismus Disorder
- A tendency for the eyes to turn in or out is controlled at all times.
- Esophoria: Eyes have a tendency to turn in
- Exophoria: Eyes have a tendency to turn out
- Hyperphoria: One eye has a tendency to turn up
The two terminologies that you may hear are exotropia or exophoria. Exotropia is when the eye turns out naturally, but exophoria is where the eye drifts out at the end of the reading or a writing task. With exophoria, the child can exert ocular effort to have single vision, but they may elicit it when they are tired, sick, or irritable.
Sequence of a Vision Screen
- Questionnaire - Clinical Signs
- Eye Dominance
- Visual Acuity
- Color and CSF
- Visual Field
- Eye Alignment and Convergence
- Pursuit screening
- Saccade screening
What do we do, and what do we see? Again, we do not diagnose conditions. We document our observations, findings, behaviors, and if need be, we refer the child to an eye care doctor.
Clinical Signs
- Head tilt
- Rubbing eyes, eye fatigue, closing one eye
- Holding objects too close
- Squinting
- Writing uphill or downhill
- Complains of eye pain or headache when completing near vision sustained tasks
- Reads slowly or rereads
- Skips words when reading
- Blurred, double vision, or complaints of a shadow
- Difficulty copying work from far to near
- Uses a finger to keep track of reading
You can create a questionnaire and give it to parents before an evaluation. I also like to start observing the child in the waiting area. As I greet the child and the parents, I look for a head tilt. If the child is in the waiting room and is reading a book, are they rubbing their eyes, squinting, or closing one eye? Are they trying to adjust the working distance? Then, during the evaluation, are they writing uphill or downhill? Are they complaining of their eyes hurting or reading slowly? Are they skipping words or using their finger to keep track of their reading?
Figure 4 shows an example of where the child is writing downhill.
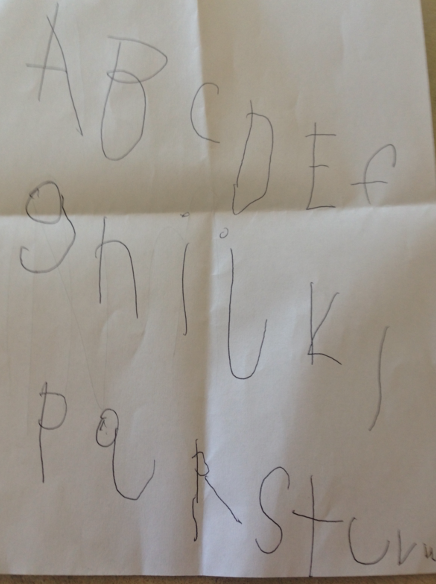
Figure 4. Example of writing downhill.
Figure 5 shows double vision and "ghosting."
Figure 5. Examples of double vision or ghosting.
The top image shows double vision, and the bottom shows ghosting. I have learned over the years that a child who has always seen double does not know any different. For them, it is normal. So if you ask a child, "Do you see double?" you are going to get a blank look. They will not notice anything unusual and cannot answer that question. I have learned not to ask those questions because we work in the habilitation frame of reference, not the rehabilitation. However, if you have a child whose development has been typical but now has issues due to a stroke or head trauma, they will see double. Double vision can also present as ghosting or shadowing of letters.
Eye Dominance
Always check for eye dominance. An easy way to do that is to have a toy telescope in your clinic and have them look through it.

Figure 6. Child looking through a telescope.
The eye that they use shows you their dominant eye.
Distal Visual Acuity
- Light source to be directed from behind the client
- Charts need to be held at the specified distance
- Chart needs to be evenly and adequately illuminated
- Test each eye separately and then together, wear glasses
We then move on to testing distant visual acuity. Snellen's a gold standard eye chart as seen in Figure 7.
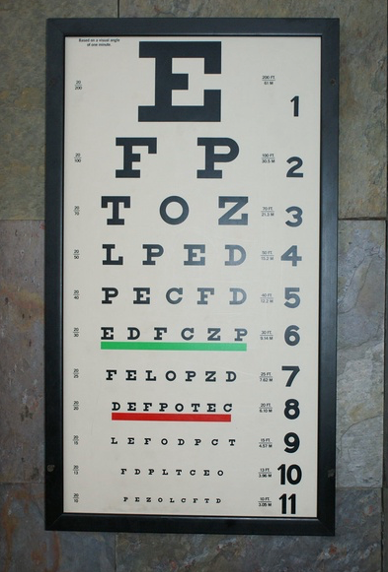
Figure 7. Testing Distance – 20 feet-Snellen chart.
Many people may be familiar with this chart. However, some children cannot identify letters, and you may need to switch to symbols charts. The other issue I come across with a Snellen chart, which may be specific to me, is that I do not have 20 feet. I barely have 10 feet. The cardinal rule when testing vision is that we have to maintain the distance. If it says 20 feet, it must be 20 feet from the eyes. Sometimes, I will use the CPAC because I can do testing at a distance of five feet.

Figure 8. Testing Distance – 5 feet
Each eye is tested separately, and then it is tested together. If the child is wearing glasses, try them on because what we are looking for is function after optical correction.
Near Visual Acuity
- Charts are usually placed 40 cm from the testing subjects
- Since reading is a binocular activity, the chart is read with both eyes
To test near visual acuity, charts are typically placed at a reading distance of 40 centimeters from the testing subject. And because reading is a binocular task, I test them with both eyes open. The Rosenbaum Pocket Vision Screener is shown in Figure 9.
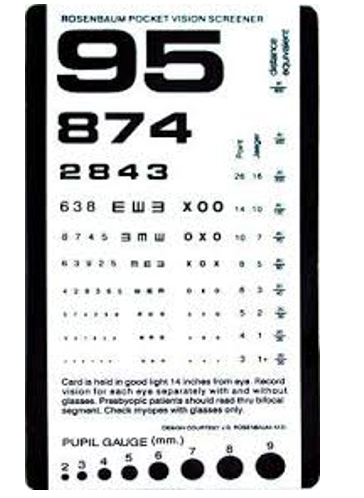
Figure 9. Rosenbaum Pocket Vision Screener.
Contrast Sensitivity Function
- Contrast sensitivity is a measure of how faded or washed out an image can be before it becomes indistinguishable from the uniform background.
Here are some examples of where I have seen reduced contrast sensitivity function in pediatrics. A child has difficulty identifying teacher A from teacher B as their eyes, nose, mouth, and ears are all the same color. Recognizing facial features when you have low contrast function is complicated unless the person has bright red lipstick or black mascara. Once this contrast is added, then the child can identify the teacher. Another area where they may be seen is the bathroom. They may slip on a puddle of water they do not see because of low contrast sensitivity function. They are also hesitant to walk into dimly-lit environments like school hallways or the school's cafeteria. They may also have difficulty reading, even though they have 20/20 vision. This is especially true with gray print on light paper, as there is reduced contrast. Two charts can be used to assess this. One is Hiding Heidi in Figure 10.
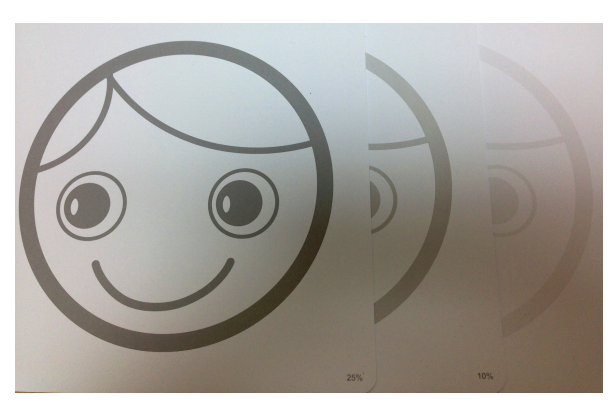
Figure 10. Hiding Heidi Contrast Sensitivity Test.
Hiding Heidi is a picture, taking away from the cognitive load of identifying numbers and letters. LEA NUMBERS Low Contrast Test is a gold standard and easy to use.

Figure 11. LEA NUMBERS Low Contrast Test.
Color
The easiest way to test for color is to have some paint chips in the clinic and have the child match them. Figure 12 shows paint samples.

Figure 12. Paint samples.
Visual Fields
- Maturation of peripheral vision has been reported to occur as young as 5 years and as old as 13 years of age, with a range of peripheral vision maturities reported between these ages. Traditionally caution is exercised interpreting VF results of children younger than 13 years.
Visual fields mature anywhere between the ages of five to 13 (Figure 13).
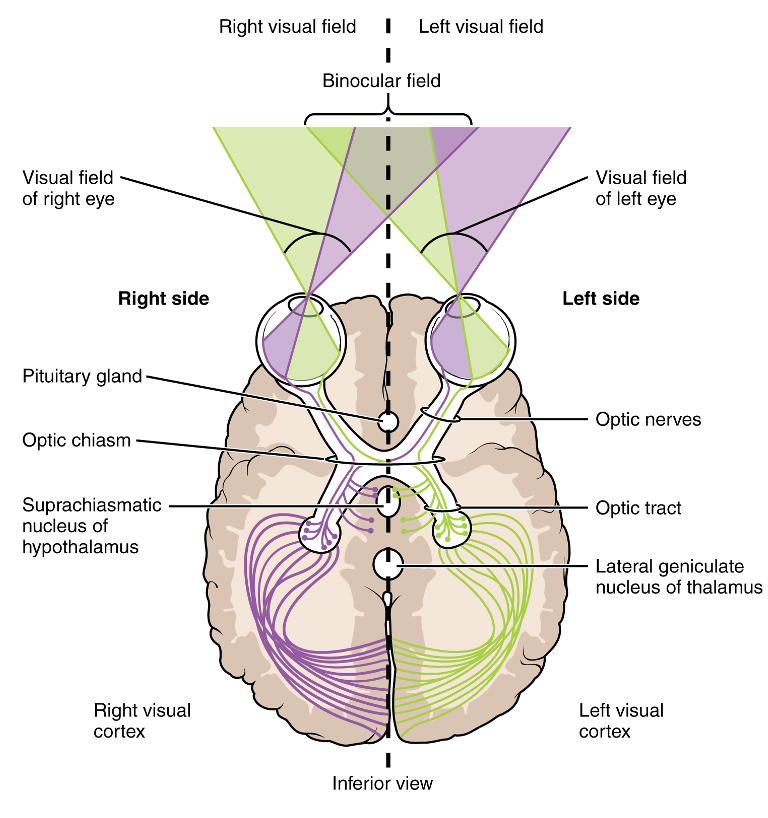
Figure 13. Illustration of the brain and visual fields (OpenStax College, CC BY 3.0 via Wikimedia Commons).
There is a wide range of maturation in this area. One example is a 16-year old post-gunshot to the right side that I evaluated one year after injury. I did my regular confrontation testing to test the visual fields. For confrontation testing, you sit opposite the child, and the child fixates on your nose. You raise your fingers in the four quadrants of vision, and they tell you how many there are. In this case, she passed it with flying colors. As a team, we were getting her back to school for half days. When I had her draw a face, this is what she drew in Figure 14.
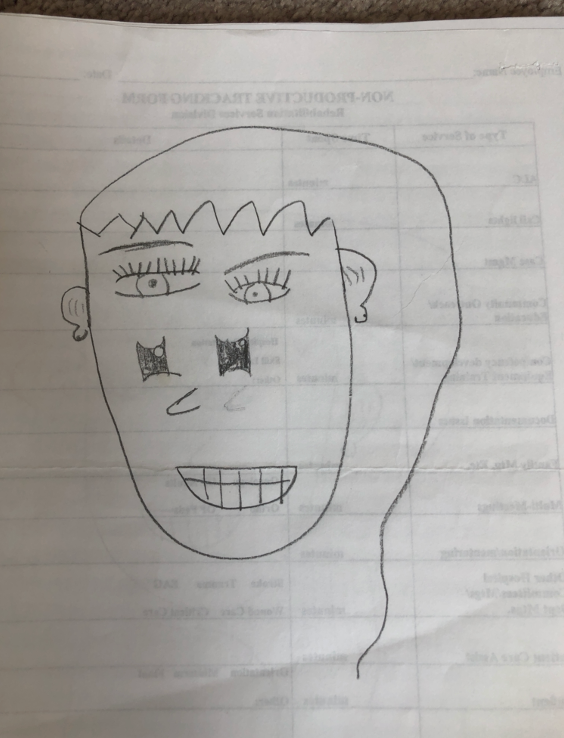
Figure 14. An image that the client drew.
I asked, "Why is the hair only on one side?" She said, "That's the hairstyle. I like it." Then I asked, "What is that under her eyes?" She was trying to draw a nose, and you can also see one that she erased. I gave her some multiplication problems, and she missed adding the hundreds column, as you can see in Figure 15.
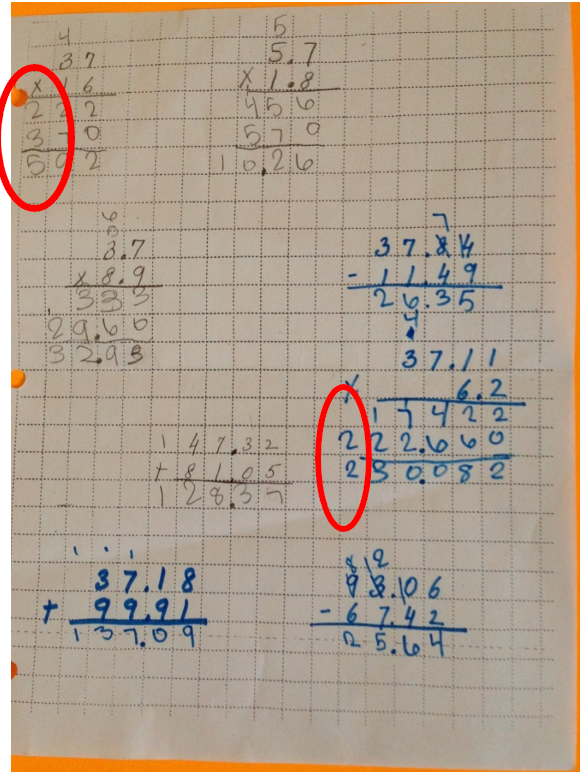
Figure 15. A math sheet with errors.
I used a blue marker to add contrast, and she missed carrying down the two. I sent this child for visual testing, and she had complete left hemianopia. My point is that even though we are doing all these screens, please be conscious of behavior and function. I had done confrontation testing on this child, and I missed the hemianopia completely because this child, for a year, had compensated so well. Everybody in the rehab hospital missed it.
Near Point Convergence
- The patient stands with feet shoulder-width apart in front of the examiner. If the patient cannot stand, have him sit with head erect and unsupported if possible; Eyeglasses on if the child wears them.
- Instruction set: "Watch the target as long as you can."
- Hold the target at eye level about 20 inches away from the face. Move the target closer to the nose.
- Watch the eyes. One eye usually drifts out (normally, this is between 2-4 inches), leading to double vision followed by recovery at 4-6 inches. The child should report double vision. Importance is placed on what you see over what is reported and on the effort required.
- A child should be able to repeat this test a few times without effort as reading for a period of time requires sustained convergence.
Convergence is the ability to follow a target towards the nose without breaking fixation. For this test, the child should wear eyeglasses if appropriate. The child sits erect with their head and neck unsupported. The target can be a finger puppet, a finger, or a thumbtack on the top of a pencil. You ask the child to watch it as long as they can as you bring it close to their nose.

Figure 16. Testing for convergence insufficiency.
If there is convergence insufficiency, the eye will drift out, and the child may report seeing double. OTs work on near-vision sustained tasks. It is essential to do this test a few times. Repeat this test a few times because reading and writing require sustained convergence.
Pursuits Testing
- The starting position is the same.
- Hold 1 target 16 inches from the face. Sixteen inches should not pull in convergence.
- Instructional set: "Watch the green tip as it goes around. Don't take your eyes off the tip".
- Move the target clockwise and then counterclockwise for 2 rotations each. Keep the target slightly beyond the circumference of the face. This should not pull in head movement.
- The pace should be neither too fast nor too slow.
Observe for smooth eye movements with very few re-fixations. Eyes should move an equal distance in each direction. Then, we look for pursuits or the ability to maintain the image of a moving target, fixed or stationary.

Figure 17. Testing for pursuits.
The starting position is the same. You keep the target 16 inches from the subject's face because you do not want them to pull in convergence. You want them to move the target clockwise and counterclockwise, two times around the circumference of the face. You are looking for the quality of the eye movements and if they are equal in both directions. Observe for spontaneous, effortless, quick eye movement that lands precisely on target and movement of head or body.
Saccades Testing
- The starting position is the same. No instructions as to or not to move the head are given.
- Two small targets are placed 16 inches from the patient's face, with each target 4 inches from midline.
- Instructional set: "When I say red, look at the red. When I say green, look at the green. Remember, do not look until I tell you."
- The patient makes 5 round trips.
In saccades, there are two targets that the child toggles between.
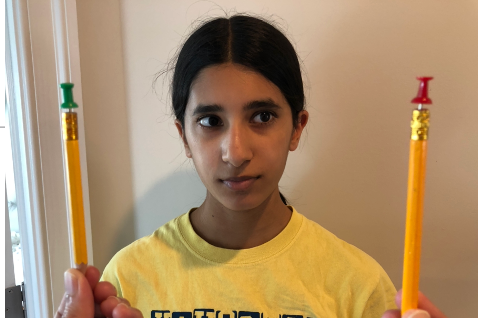
Figure 18. Testing for saccades.
You will have the child look to the right (green) and then to the left (red). You watch for spontaneous, effortless, and quick eye movements that land precisely on the target. What do you do when you have gathered this data?
- The NSUCO Method of Scoring Saccades and Pursuits Ability
- https://drboulet.com/wp-content/uploads/2012/08/NSUCO-Oculomotor-Test-via-PUCO.pdf
For both pursuits and saccades, I use the NSUCO method. I have provided a link for anybody interested. This scoring gives minimally acceptable scores by age and sex. We refer the patient if their scores are below the norm after the screening.
Test for Binocular Vision
- The child wears red/green glasses with the red lens in front of the right eye and the green in front of the left eye.
- If the right is suppressing, the red dots or the red figure will not be seen and appear black, if the left is suppressing, the green dots or the green figure will not be seen and appear black.
- Pegs of red, green, and black color can also be used.
Binocular vision needs to be tested because it can have a high functional significance, especially in gait and mobility. The child wears red/green glasses and then looks at a flashlight with three pictures, as shown in Figure 19.
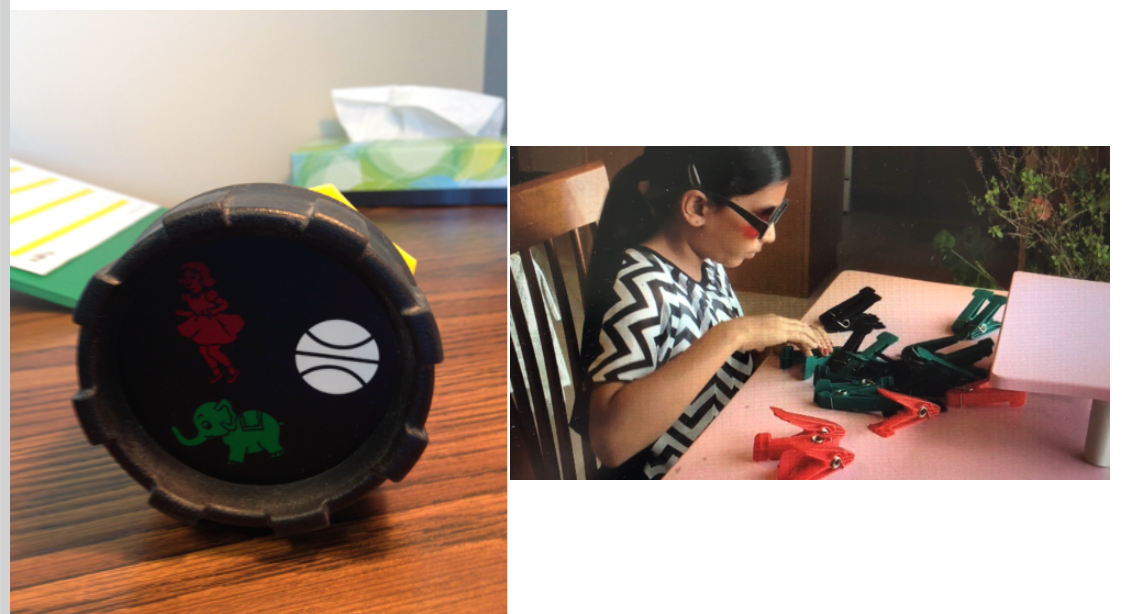
Figure 19. Testing for binocular vision.
If the child is suppressing information from the right eye, the child will only see the green elephant and the white wall. If the child is suppressing information from the left eye, the child will only identify the red goal and the white wall. This means that even though both eyes are open and look normal, because there is a disparity of images coming from both eyes, the brain cannot get a single fused image. The brain stops processing information from the dysfunctional eye.
I do a lot of neurological rehabilitation, and it is interesting to me how a child who has had suppression pans out into an adult. I would like to share a story to show how behavior evolves with vision as we grow older. I was interviewing a husband and wife. The wife who had had a stroke was a principal. During a vision screen, I asked her, "Do you ever go to an IMAX theater? She replied, "Yeah, all the time." I asked her if she appreciated the experience because my testing told me that she did not have binocular vision. She sheepishly said no, so I asked her, "Why do you go then?" She answered, "Because if I don't go, my husband will not go." Binocular vision is critical and not just for IMAX. Functionally, the child will have issues with perception.
Goal Writing
- Child will be able to compensate for his/her vision loss to engage in academic tasks where accuracy and speed are improved by 10%, for example from 70% to 80%.
- Child will improve the speed and accuracy of saccadic eye fixation by decreasing the time to copy 2 words from the blackboard by 5 seconds.
- Child will improve the speed and accuracy of pursuit eye movements for improving upper extremity coordination for catching a medium size ball thrown to him 5 consecutive times.
- Child to be able to complete meal preparation with minimum assist of one where he/she is able to set the dial on the oven using a handheld magnifier with 100% accuracy 2/4 trials.
Here are some examples. I have been doing this for 20 years and have not had any issues yet. I always try to make my goals reflect vision and function.
OT Intervention
The human brain makes predictions based on the information coming in depending upon the context and environment. For example, Johnny will use a prone scooter board to figure out spatial relationships and his position in space. In this context (hallway) and environment (therapy gym with other kids and therapists), Johnny has to make predictions and figure out how to turn his scooter to make it from point A to point B without any accidents. If Johnny does that, he has a successful outcome. If he is not successful, what is the next step? We can have Johnny go from point A to point B in an empty hallway, or Johnny can go from point A to point B between stationary chairs. You are changing the environment from dynamic to static. Based upon the OT Practice Framework, we make adjustments to the task. Eventually, these tasks become more advanced, like driving a car.
For Visual Acuity: Wear Glasses/Contact Lens
If the child needs to wear glasses and contacts, please encourage them to do so. I did this exercise shown in Figure 20 with one of my clients.
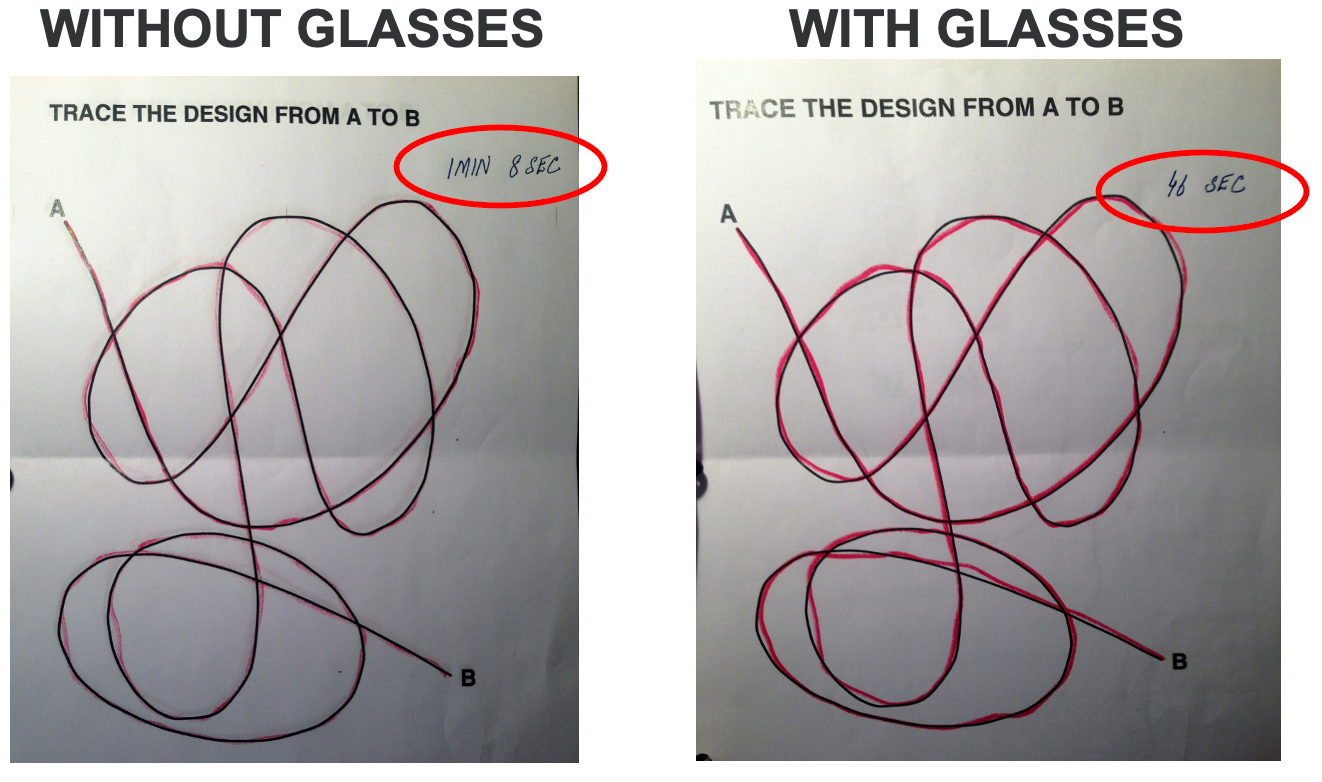
Figure 20. Example of a task with and without corrective lenses.
When she wore glasses, a simple tracing task took 46 seconds, but a simple tracing task took one minute eight seconds when she did not wear glasses. If a child wears glasses, do not assume they are 20/20. Best-corrected vision when wearing glasses can be 20/40, 20/60, 20/80, or 20/100. I have a dear friend who is an occupational therapist with an eight-year-old. Her daughter wears glasses, and her best-corrected vision is 20/80.
Be Aware of Font Sizes for Reading
If the best-corrected vision is 20 by 100, our job is to make sure that the print size of what they are reading is appropriate. As you look at this chart in Figure 21, feel free to use this information in your practice. For example, 20 by 100 requires 16 point font. We can use this information to educate the client, caregivers, teachers, and administrators.
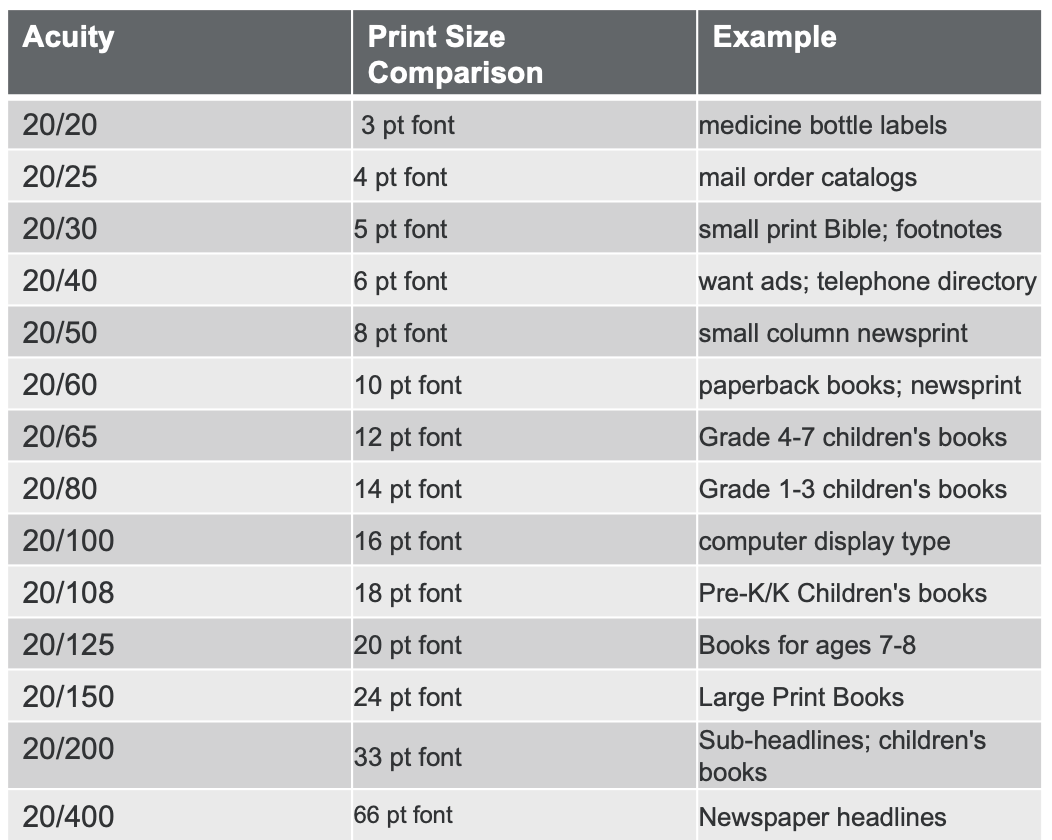
Figure 21. The following is a list of environmental print that correlates to the acuity on a Near Vision Snellen Test Chart
Convergence Insufficiency
- Enlarging the font or using large print will increase the focal distance and reduce the need for convergence. Use magnifiers if the font size cannot be adjusted.
- Each magnifier has a focal distance, and if the object is outside the focal distance it will appear upside down
- The magnifier can be held anywhere in relation to the eye, the object to be viewed must be within focal distance
- The weaker the magnifier, the bigger the field of view; the stronger the magnifier, the smaller the field of view
Convergence is the ability to fixate a single target as it comes towards our nose, as discussed earlier. For convergence insufficiency, we can help by enlarging the font. Font can be enlarged like we just talked about by changing the size of the optotype to get from eight-point to 16-point, or it can also be done with the use of magnifiers.
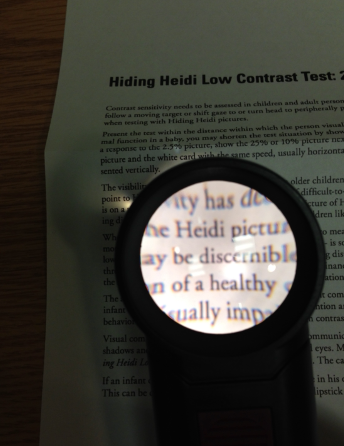
Figure 22. A magnifier enlarges the type on a page.
I have a handful of kids that are use magnifiers in the clinic and school. Usually, the optometrist or ophthalmologist recommends the optimal magnifier, and the family buys the magnifier before they come to me. I then work with the child to ensure they know how to use it. If it is not used at the proper distance or is upside down, the magnifier will end up in the trash can.
There are different kinds of magnifiers. One is a bar magnifier with a line guide (Figure 23).
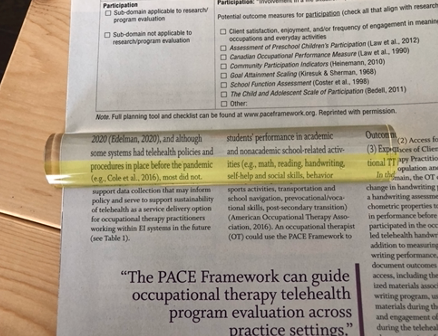
Figure 23. Example of a bar magnifier.
With this option, you do not have to adjust the focal distance because it is already built-in. If the bar magnifier does not provide enough magnification, hand and stand magnifiers would be the next level. They will only be able to read a little within that lit circle, as in Figure 22.
Activities Facilitating Convergence
- Forward ball pass
- Prone - Blow pens
- Masks and Glasses
- Scratch and sniff stickers or pencils
- Have the patient supine on an exercise ball and then have him track the clown nose (level of difficulty – hard)
These are different activities that can facilitate convergence. My favorite is the forward ball pass (Figure 24).
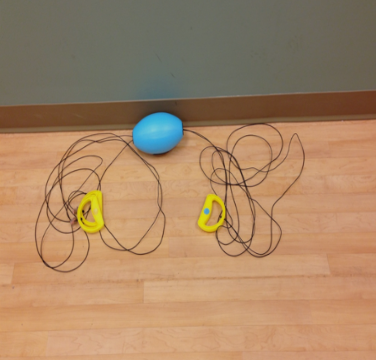
Figure 24. Forward ball pass.
With this, you stand at one end, and the child stands at the other end. When you abduct your arms, the ball is sent down the rope to the child. As the ball is coming towards the child, their eyes will converge. This activity works on pursuits as well.
An activity you can do in a prone position will help with convergence insufficiency. Using blow pens is an example. Children also love dressing up, and wearing different noses or masks can work on convergence (Figure 25).

Figure 25. Examples of costumes.
The red or big brown nose encourages convergence. You can have the patient lay prone on an exercise ball, and they can reach for your clown nose. Scratch and sniff stickers and smelly pencils are also great.
Choose Alternate Positions for CI
Choosing alternate positions for convergence insufficiency can be seen in Figure 26.
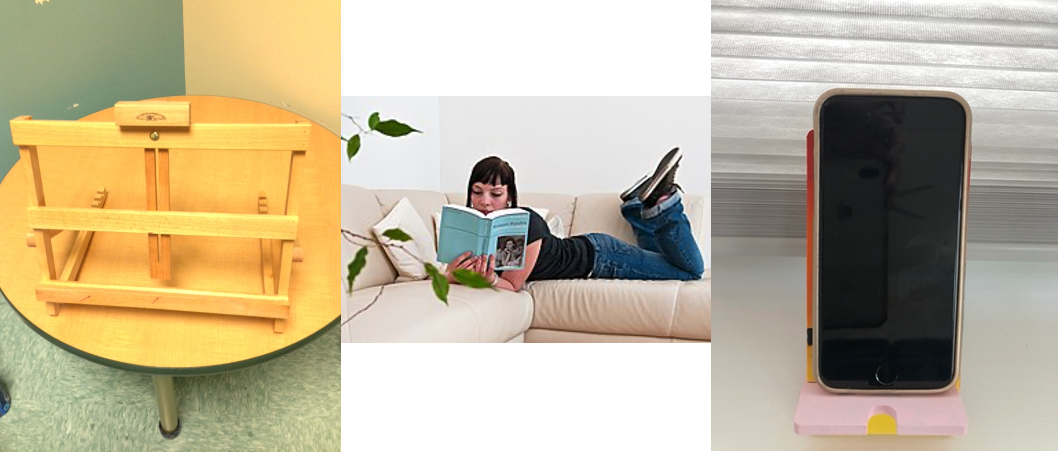
Figure 26. Examples of alternative positions to encourage eye convergence.
Prone positioning is helpful, as are vertical stands. I use book stands all the time. Looking up reduces the need for convergence while looking down requires more convergence.
Light/Good Illumination
- Increase task as well as ambient lighting within the room. Avoid fluorescent lights, use halogen, LED, or full-spectrum light. Halogen light has good luminance; hence it is great for task lighting but can get too hot. Full-spectrum lighting is best if glare sensitivity needs to be addressed.
- Always have a reading light placed behind the dominant eye.
- Use gooseneck or swing arm lamps, adjust the height for task lighting.
No matter what the visual deficit is, good lighting is essential. Many different types of lights are out there. Some examples are in Figure 27.
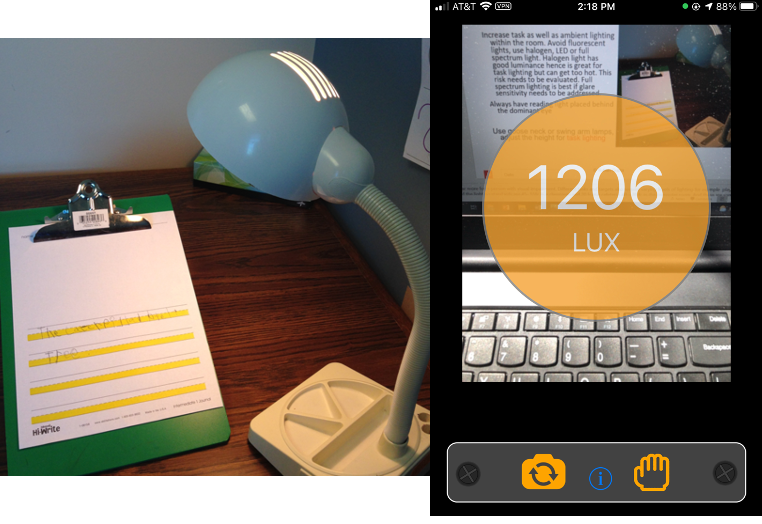
Figure 27. Examples of lighting.
Often, the question I get is, what lighting is the best. The answer is straightforward- whatever the child prefers. The key is having different lights available for the child to perform the preferred task. Fluorescent lighting is generally not preferred as it is made of compressed gas, often flickers, and can irritate those with low vision. Halogen lighting has excellent illumination, but it gets very hot. For children with sensory deficits, halogen lighting may not be optimal. Material can also burn if placed near this light source. LED lighting comes in different colors. There is also full-spectrum lighting. I have two daughters, and one loves LED while the other prefers halogen. Keep in mind to always have a reading light placed behind the dominant eye.
The image on the right is "1206 lux," as I was trying to measure the lighting when developing this slide. This is a good number as the industry standard is 500 lux. You are in good shape if you can get lighting up to 1,000 lux at the workstation. I let clients with iPhones or Androids pull their phones out and measure light using a Lux Meter app. This app can be installed after permission from the parents to measure the lighting in different settings. Flexible lamps can also be used to get optimal lighting. As the light source gets closer to the working surface, you should see a jump in that number.
Adding Contrast
- Increase contrast and reduce pattern by selecting workspace where there is minimum clutter and solid background
- Keep workplaces predictable
- Choose a workplace where glare is absent or minimum (avoid reflective surfaces or sitting against windows)
- Choose a workspace where light is from a direct source
Adding contrast, we know that kids have low contrast. What can we do about it?
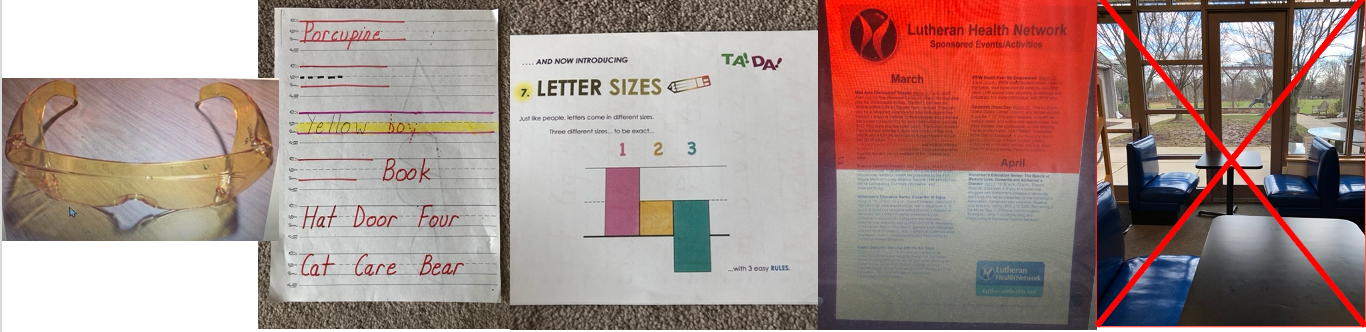
Figure 28. Examples of adding contrast.
To add contrast, we can use VR filters. Light-colored filters are preferable indoors, while dark-colored filters are preferable outdoors. You can also use overlays. Overlays can be of different colors. Highlighting paper can help with the sizing of letters. Keeping workplaces predictable with a direct light source with minimal glare is also vital. Those with reduced contrast sensitivity function are susceptible to glare.
General Treatment Principles
All activities support intervention by an optometrist; none are instead of visual skills training done by an optometrist.
- Saccades – large to small eye movements
- Pursuits – small to large eye movements
- Eliminate head movements - use weights on the head or have the patient tuck a ball under the chin and hold it
- Increase difficulty by using bosu, astroturf, balance beam, skateboards, metronome or adding cognitive tasks
- Move the child to a different environment – same demands with the same accuracy
- Let the child be the therapist. Can the child instruct you to complete the task?
- Always work on accuracy and then improve time
For pursuits, the level or the order of difficulty is small to large eye movements. Try and eliminate extraneous head movements. If the child is doing activities for saccadic eye function, movement of the head is not wanted. An easy way to do this is to have the child tuck a ball or plastic water bottle between their chin and chest to eliminate head movements.
You can also increase the difficulty level by adding or putting in some physical challenges like using a bosu ball, a balance beam, or AstroTurf. You can also add a cognitive layer by having them do a task to the beat of a metronome. You can also move the child to a distracting environment because the child has to perform in school where there are 20 other kids, pencils dropping, overhead pages, and teachers moving around. You want to see if there is a transfer of learning to school. Lastly, you can also work on accuracy and improving time.
Treatment Ideas for Saccades
- I Spy game – sitting
- Base flashlight games
- TPOT software
- Have the patient complete a letter cancellation task (one paragraph); the goal is less than 1 minute
- The symbol worksheet can also be used as needed
- Hart Chart
Progression is from large eye movements to small eye movements. It is easier for eyes to move from one end of a room to the other, but it is harder for eyes to read print or move in a letter cancellation task. Examples of saccade treatment ideas are shown in Figures 29-33.
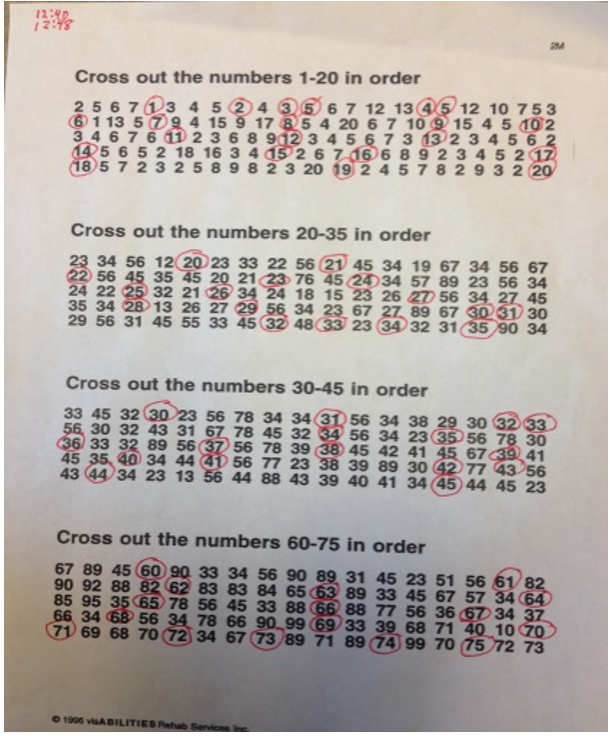
Figure 29. Letter cancellation task.
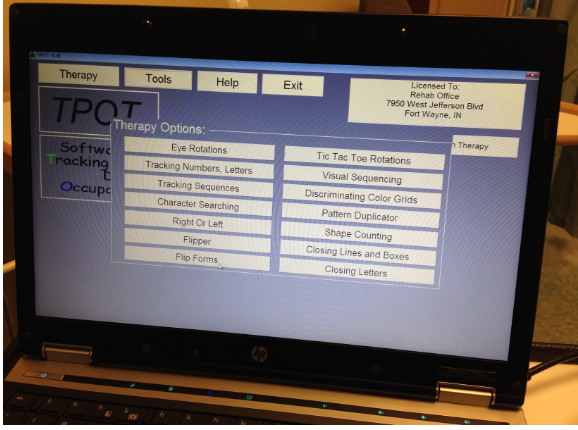
Figure 30. TPOT software.
 1.
1.
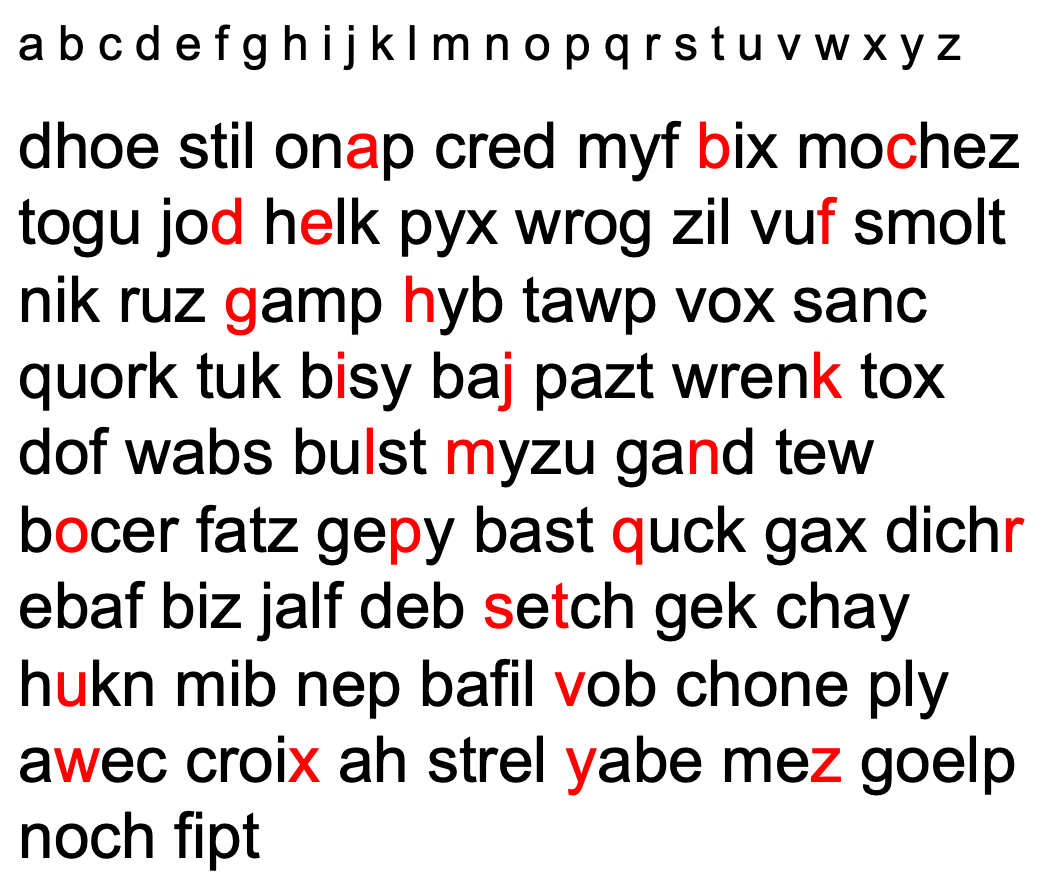
Figure 31. Letter search activity.
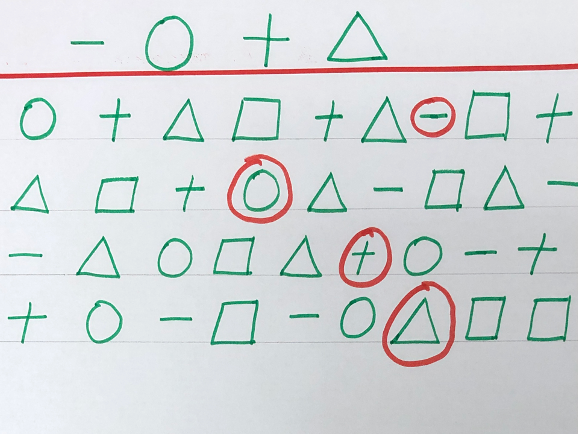
Figure 32. Shape and sequencing search activity.
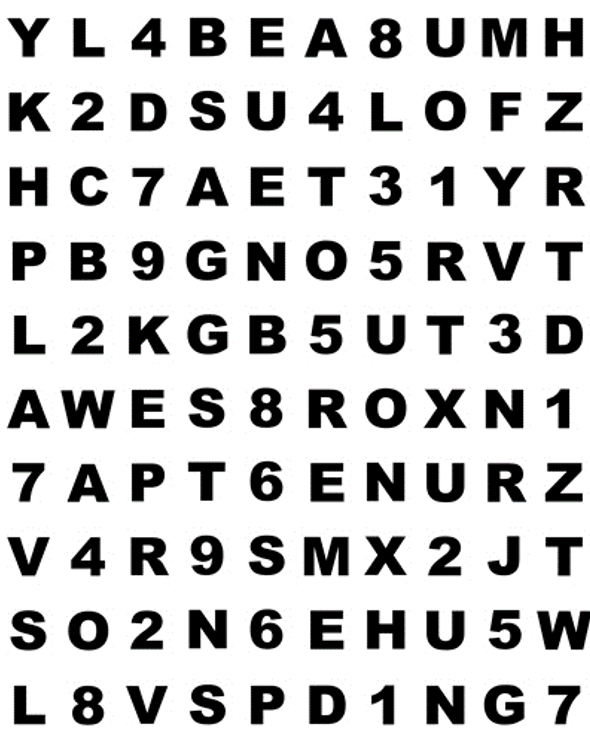
Figure 33. Hart Chart.
I like to use an I Spy game for lower functioning clients. I can have them start from one end of the room to the other and then progressively make it more difficult by finding objects closer to each other. Another activity uses masking tape to make "baseball bases" on the wall and turn off the light. The child has to shine a flashlight on base A, then B, etc. You can demonstrate the movements first. This movement encourages pursuits. TPOT software is an OT computer program that works on tracking and perceptual skills and addresses saccades, pursuits, visual closure, spatial orientation, and figure-ground.
Simple letter cancellation sheets are also options. Letters can be found and crossed out, or letters are identified in a sequence. For example, you have to find the A, B, then C, and so on. However, if you miss something in the series, you will not get A to Z in that paragraph. The endpoint for this activity would be that the child can do this within one minute with no errors. It is a challenging activity that I even use with some of my older kids. Some kids have difficulty naming letters in a sequence without auditory recall, like singing the ABCs. Other kids may not recognize optotypes, and for these cases, you can use symbol worksheets.
Tracking Materials - Ann Arbor Publishers have a vision tutor series that can come in very handy. I assume most of you have heard or worked with a Hart chart. You place the Hart chart five to 10 feet away, and the patient calls out a letter in the first column and then calls out the first letter in column 10. Looking at Figure 33, the sequence would be Y, H, K, Z, H, R, P, T, L, D, A, 1, 7, Z, V, T, S, W, L, and 7. They are making a saccadic eye jump from the left side to the right side of the page. If they can do this within 15 seconds with no errors, they have efficient reading saccades. You can challenge them by doing column two to column nine or make this activity more difficult by having them do it to the beat of a metronome. They can also do this activity on different surfaces.
Treatment Ideas for Pursuits
- Visual tracing workbooks/mazes
- Patient can use the pencil as a motor and visual aid
- Patient then uses the finger as a motor aid
- Patient has to use the eyes only
Pursuits, visual tracing workbooks, and mazes are often available online for free. You can print them out and grade them in the ways we just discussed. The child can use a pencil for a visual and a motor aid. Then you take the visual aid away, and the child can use their finger as a motor aid. Lastly, the child can either put their hands in their pocket or sit on their hands to complete the tracking task. An example is shown in Figure 34.
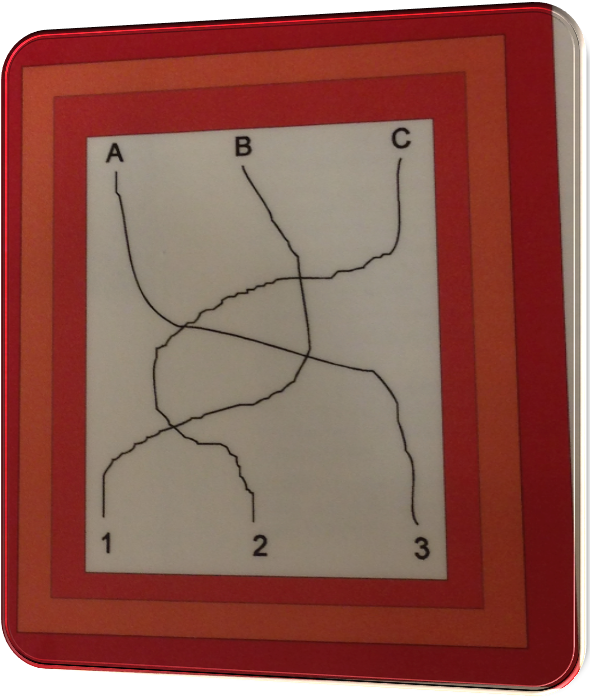
Figure 34. Example of a tracking task.
- Rotating pegboard
- Place stickers to make the task easier
- Place the peg in the hole in one smooth movement once the patient has found the hole
- Move the pegboard, the child keeps the peg over the respective hole for 1,2,3 rotations and then places the peg
You can also use a rotating pegboard, as seen in Figure 35.
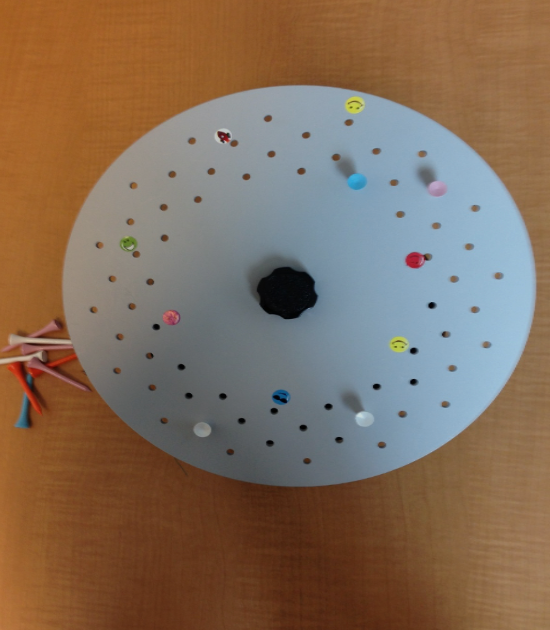
Figure 35. Rotating pegboard.
For example, I will put a pink sticker next to a hole, and the child is expected to place a golf tee in one smooth, coordinated movement. You can make that activity harder by placing the tee after one or multiple turns.
- Flashlight tag along with rain stick and forward ball pass are great activities to engage pursuits
Figure 36 shows a rain stick.

Figure 36. Example of a rain stick.
The rain stick can be placed vertically, and the child can track the bits that are falling from top to bottom. I mentioned an earlier flashlight task. You can also play flashlight tag, where the child has to superimpose his flashlight over yours. You can have two different color flashlights like red and green and tell them to catch you. Again, the forward ball pass is another excellent activity for pursuits.
We can also make some computer adaptations. Some examples are in Figure 37.
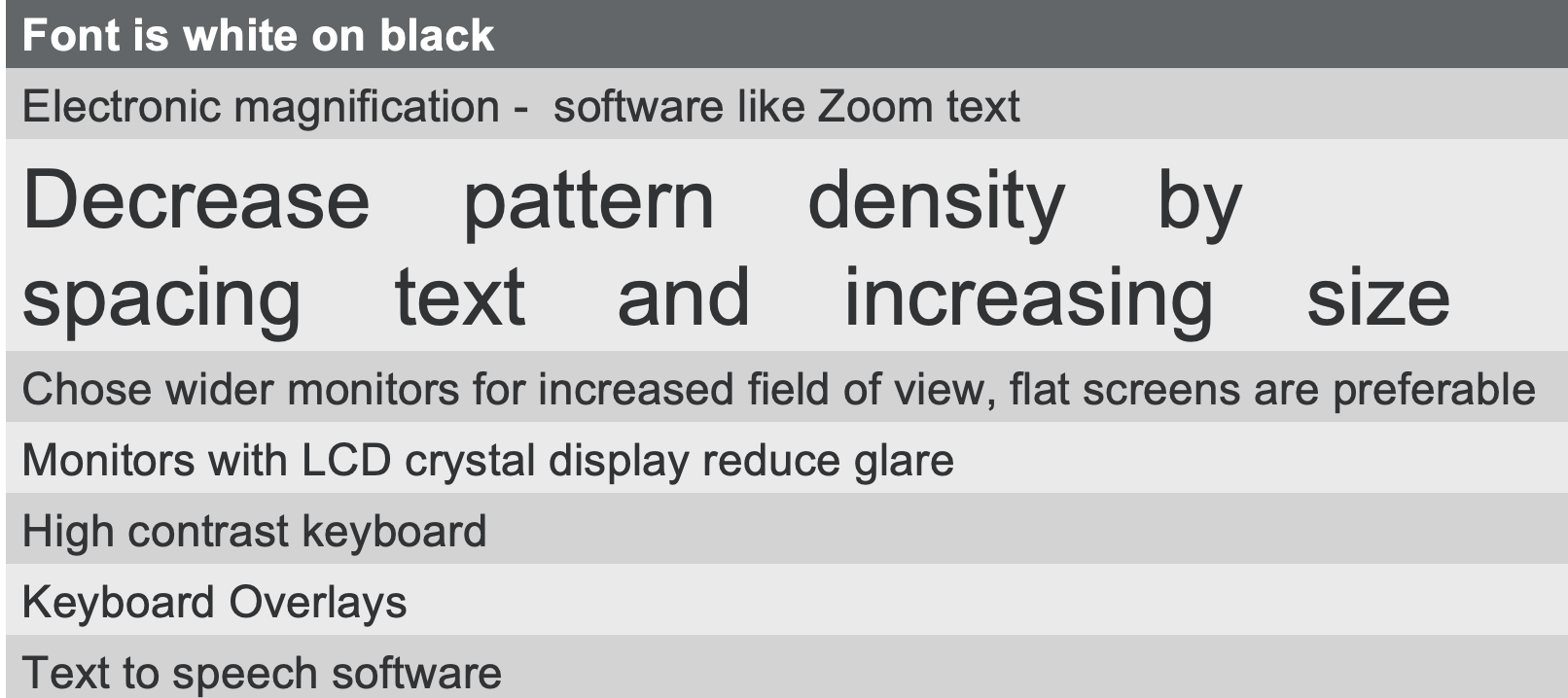
Figure 37. Some examples of computer adaptations.
We can change the font color or size, remove glare, use specific, simple fonts like sans-serif (Arial and Helvetica are examples), or color filters. Font size can range from 8-point to 20-point. You can enlarge the size of the cursor to decrease the child's frustration. You can also reduce the pattern density by spacing the text and increasing the size. I recommend LCD crystal displays, flat screens, and high contrast keyboards for families that can purchase a computer. An example of a high-contrast keyboard can be seen in Figure 38.
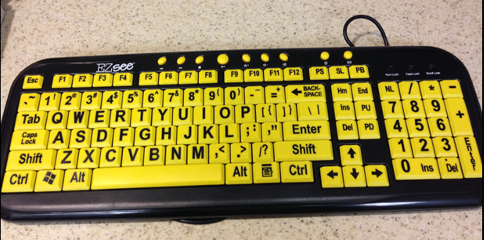
Figure 38. Example of a high contrast keyboard.
Text to speech software is also an option.
Occlusion in Pediatrics
I often get a lot of questions about occlusion. It should only be used if directed by an ophthalmologist or an optometrist because children can develop suppression and amblyopia, functional blindness. We, as therapists, do not occlude pediatric clients. Sometimes, I will occlude older clients who have had a stroke or a brain injury as the visual system is myelinated after nine or 10. Until the age of nine or 10, the visual system is still myelinating and developing, and we do not want to cause undue harm.
Questions and Answers
I use a rolled piece of paper and ask the child to look through it like a telescope as I do not have an actual telescope in my room. I love that you use a real one.
I do not have a real one; I use a toy telescope. If a telescope or paper is not handy, I often save paper towel or toilet paper rolls. You can also have them create a circle with their fingers.
Do you have recommendations for individuals that use eye-gaze as an access method for communication devices in terms of placing a light on the side of their dominant eye?
That is a good question, and I think that would need some kind of an evaluation done by an assistive technology practitioner. They will probably be using whatever eye movements are more substantial with eye gaze. It is crucial to identify what the dominant eye is and then place the light either on the side or behind the client. Never place the light in front as that creates glare.
What exercises do you recommend for a four-year-old child with alternating esotropia? The child is in vision therapy, but should OT be offered?
The optometrist can be working on retraining eye muscles, but the OT can help with compensatory strategies or modify the environment. Remember the OT Practice Framework where we talked about context and environment. When you have an esotropia, you will have double vision for distant vision. Exo is when you have difficulty reading, and eso is when you see double in the distance. We want to look at functional mobility with this child.
I currently work in a school system and have many issues with students who cannot form diagonal lines and letters such as X. What visual exercises would you suggest?
First, I would complete a visual screen. When doing diagonal lines, we are now moving to visual perceptual skills. Once you have established that acuity, contrast sensitivity, and eye teaming are all in place, let's start looking at gross motor activities, not just paper and pencil tasks.
What is the clinical implication if a student has right eye dominance and left-hand dominance?
The clinical implication is that it is normal. Mixed dominance happens all the time. The only issue might be a shadow of the child's hand when writing with the opposite side from their dominant eye. You may have to adjust the work environment to make it the best for the child.
What apps can I download and use with my tablet for visual perceptual and visual closure activities?
I do not necessarily have an app in mind, but I have a website, eyecanlearn.com. I have used that website like crazy during this COVID world. It is a free resource that does an excellent job of breaking down activities according to perceptual skills, tracking, saccades, pursuit, and so on.
Any recommendations for assessing dominance in individuals with limited motor skills?
You can ask the family to close one eye, and then you know what eye is the dominant eye. The dominant eye will always lead during fixation, which we can observe when looking and reading. We can also observe posture, head tilt, or interview the family.
References
Colenbrander, A. & Fletcher, D. C. (1995). Basic concepts and terms for low vision rehabilitation. Am J Occup Ther, 49(9):865–869.
Bellocchi, S., Muneaux, M., Bastien-Toniazzo, M., & Ducrot, S. (2013). I can read it in your eyes: What eye movements tell us about visuo-attentional processes in developmental dyslexia. Research in developmental disabilities, 34(1), 452-460.
Bennett, C. R., Bauer, C. M., Bailin, E. S., & Merabet, L. B. (2020). Neuroplasticity in cerebral visual impairment (CVI): assessing functional vision and the neurophysiological correlates of dorsal stream dysfunction. Neuroscience & Biobehavioral Reviews, 108, 171-181.
Bjerre, A., Codina, C., & Griffiths, H. (2014). Peripheral Visual Fields in Children and Young Adults Using Semi-automated Kinetic Perimetry: Feasibility of Testing, Normative Data, and Repeatability. Neuro-ophthalmology (Aeolus Press), 38(4), 189–198.
Cahill, S. M., & Beisbeir, S. (2020). Practice Guidelines—Occupational therapy practice guidelines for children and youth ages 5–21 years. American Journal of Occupational Therapy, 74, 7404397010. https://doi.org/10.5014/ajot.2020.744001
Crowdy, K. A., Kaur-Mann, D., Cooper, H. L., Mansfield, A. G., Offord, J. L., & Marple-Horvat, D. E. (2002). Rehearsal by eye movement improves visuomotor performance in cerebellar patients. Experimental brain research, 146(2), 244-247.
Frolek Clark, G., & Kingsley, K. L. (2020). Practice Guidelines—Occupational therapy practice guidelines for early childhood: Birth–5 years. American Journal of Occupational Therapy, 74, 7403397010. https://doi.org/10.5014/ajot.2020.743001
Hyvärinen, L. (1995). Considerations in evaluation and treatment of the child with low vision. American Journal of Occupational Therapy, 49(9), 891-897.
Loh, A. R., & Chiang, M. F. (2018). Pediatric vision screening. Pediatrics in review, 39(5), 225.
McDowell, N., & Dutton, G. N. (2019). Hemianopia and features of Bálint syndrome following occipital lobe hemorrhage: Identification and patient understanding have aided functional improvement years after onset. Case reports in ophthalmological medicine.
Occupational Therapy Practice Framework: Domain and Process—Fourth Edition. (2020). Am J Occup Ther, 74(Supplement_2):7412410010. https://doi.org/10.5014/ajot.2020.74S2001
Radomski, M. V., Finkelstein, M., Llanos, I., Scheiman, M., & Wagener, S. G. (2014). Composition of a vision screen for service members with traumatic brain injury: Consensus using a modified nominal group technique. American Journal of Occupational Therapy, 68(4), 422-429.
Rucker, J. C., & Tomsak, R. L. (2005). Binocular diplopia: A practical approach. The neurologist, 11(2), 98-110.
Scheiman, M. (2011). Understanding and managing vision deficits: a guide for occupational therapists. Slack Incorporated.
Scheiman, M., Gwiazda, J., & Li, T. (2011). Non-surgical interventions for convergence insufficiency. Cochrane Database of Systematic Reviews, 3. Art. No.: CD006768. DOI: 10.1002/14651858.CD006768.pub2
Taylor K., Powell, C., Hatt, S. R., & Stewart, C.. Interventions for unilateral and bilateral refractive amblyopia. Cochrane Database of Systematic Reviews, Issue 4. Art. No.: CD005137. DOI: 10.1002/14651858.CD005137.pub3
Tailor, V., Bossi, M., Bunce, C., Greenwood, J. A., & Dahlmann-Noor, A. (2015). Binocular versus standard occlusion or blurring treatment for unilateral amblyopia in children aged three to eight years. Cochrane Database of Systematic Reviews, Issue 8. Art. No.: CD011347. DOI: 10.1002/14651858.CD011347.pub2
Citation
Gupta, S. (2021). An occupational therapist's perspective on visual deficits in pediatrics. OccupationalTherapy.com, Article 5482. Available at www.occupationaltherapy.com

