Editor's note: This text-based course is a transcript of the webinar, Overview of Prematurity and Associated Conditions, presented by Rhonda Mattingly Williams, EdD, CCC-SLP.
Learning Outcomes
- After this course, participants will be able to:
- list 3 short-term complications associated with prematurity.
- recognize 3 long-term complications associated with prematurity.
- identify 3 ways early experiences of the premature infant impact development.
Introduction
Today, we are going to talk about prematurity and the various diagnoses that can co-occur, but also the impact of this phenomenon on the child and family.
Before I talk to you about this at-risk population for prematurity, let me define prematurity for you. A premature infant is born less than 37 weeks gestation, so if they are born at 36 weeks and six days, they are considered premature. If they make it to 37 weeks gestation, they are considered term. Most pregnancies are anticipated to last 40 weeks, but anything 37 to 40 is considered term delivery.
There are several reasons that the content today is important to you as a therapist. Even though this is not a topic in which we are discussing therapeutic evaluation and intervention strategies specifically, it impacts a great number of clients that you and I both see. If we want to understand how and why a child is presenting a certain way on our caseload, then we need to understand their diagnosis. And if prematurity is part of that diagnosis, that is very important information to know.
Secondly, we need to understand why the caregiver's parents are behaving in certain ways, what they have gone through, and how they interact with that child. Again, this is going to make us more successful. We want to help these folks have less stress, which automatically is going to help them participate.
Lastly, we need buy-in from caregivers. If you want to get buy-in, show caregivers that you understand, as much as you possibly can, what they and their child have gone through.
At-Risk Populations for Prematurity
- Low income
- Women of color
- Women younger than 20; older than 40
- Women who were born prematurely
- Women with a h/o a previous premature delivery
- Women with multiple pregnancies
- Women with uterine/cervical abnormalities
There are several at-risk populations for prematurity, including women of low income, women of color, women younger than 20, women older than 40, women who were born prematurely themselves, women with a history of previous premature delivery, women with multiple pregnancies, and women with uterine and cervical abnormalities.
As I was researching for this talk, one of the studies that I found talked about the fact that Black women in the US are still over 50% more likely to have a premature delivery than White women. Other studies attributed this to racism-related stress, not only in the woman that has a premature baby but also in previous generations. I thought this was interesting because we know that stress has a huge impact on the body and the mind.
Additional Risk Factors for Prematurity
- Smoking, alcohol, substance use
- Infection
- Stress
- Trauma
- Unintended pregnancy
- Chronic health conditions
- In-vitro conception
- H/o repeated miscarriages/spontaneous abortions
Additional risk factors are things like smoking, alcohol, substance use, infection, stress, trauma, unintended pregnancy, chronic health conditions, like diabetes and high blood pressure, in vitro conception, and then a history of repeated miscarriages or spontaneous abortions. All of these factors place someone at a higher risk of delivering a premature infant.
Incidence
- Estimated to be 11 percent of births (average) worldwide
- Translates to 15 million preterm infants born per year
- 1 in 10 infants born preterm
It is estimated that 11% of births worldwide are premature. This translates to about 15 million preterm infants being born per year, and one in 10 infants. The incidence ranges from about 5% in parts of Europe to 18% in parts of Africa.
Additional Statistics
- Associated with approximately 1/3 of infant deaths in the U.S.
- Accounts for ~ 45 % of children diagnosed with CP
- Accounts for ~ 35 % of children with vision impairment
- Accounts for ~ 25% of children with cognitive & hearing problems
Prematurity is associated with approximately 1/3 of infant deaths in the US, and it accounts for about 45% of children diagnosed with cerebral palsy. It accounts for about 35% of children with vision impairment and about 25% of children with cognitive and hearing problems. If you think about these statistics, a good bit of your caseload probably has a history of prematurity.
Classification-Gestational Age
- Late Preterm Birth – Between 34 (0/7) and 36 (6/7) Weeks GA
- Very Preterm Birth – Less than 32 Weeks GA
- Extremely Preterm Birth – At or Below 28 Weeks
A late preterm infant is born between 34 weeks and 36 and 6/7 days weeks gestational age. I remind you that most people will say term birth is 40 weeks, but anything 37 weeks and beyond is considered term. Before, we used to think that late preterm births had no issues, but over the past few decades, we have realized that this population also has some issues down the road. We cannot say, "They are 35 weeks, no big deal."
Next is a very preterm birth that is less than 32 weeks gestational age. An extremely preterm birth is at or below 28 weeks gestation. The risk of complications increases with that degree of prematurity. Those born at or before 25 weeks have the highest mortality rate of about 50%.
Classification-Birth Weight
- Low Birth Weight – birth weight is less than 2500 g
- Very Low Birth Weight – birth weight is less than 1500 g
- Extremely Low Birth Weight – birth weight less than 1000 g
If the child is born at 5.5 pounds (2500 g), then they are considered low birth weight. To put that in perspective, this is about how much a two-liter soda bottle weighs. A very low birth weight infant is about 3.3 pounds at birth or 1500 g. This is about the weight of a steam iron at your house. Extremely low birth weight is 2.2 pounds or less than 100 g, which is about a quart of orange juice or a quart of milk.
Even if an infant is not preterm or premature, low birth weight is associated with many problems down the road. It depends on why that is. For example, I have seen tiny babies in the NICU that have petite parents. We need to take this into consideration, and dieticians look at these factors as well.
Adjusting for Prematurity
- Determine gestational age in weeks
- Subtract the gestational age from 40 weeks
- Subtract the weeks of prematurity
- Example:
- Olivia – born at 30 weeks gestation
- 40 weeks-30 weeks = 10 weeks premature
- Olivia – currently 16 weeks chronologically
- 16 weeks (chronological age) – 10 weeks premature = 6 weeks adjusted
Some places do not adjust for prematurity in terms of their early intervention system, and some places do. Here is an example of how to adjust for prematurity. Olivia was born at 30 weeks so we take 40 weeks and subtract 30 weeks to find out that she is 10 weeks premature. Olivia's actual age is 16 weeks chronologically (how long she has been out of the womb). Thus, her adjusted age is 6 weeks old. This matters a great deal because if she is treated like a 16-week-old, then we would expect much more from them, like introducing solids.
I have had people over the years say, "I've got this baby that is not doing anything I expect them to do." Once you research this a bit, you realize that they are premature. This child should have been in utero for a little bit longer.
Again, some early intervention systems do not adjust for prematurity.
Associated Diagnoses: Impact on Feeding Development
There are associated diagnoses that will impact feeding development. I say feeding development, but as we go through this presentation, it impacts the overall child.
Short-term Complications of Prematurity
- Hypothermia
- Respiratory complications
- Cardiovascular abnormalities
- Intraventricular hemorrhage (IVH)
- Necrotizing enterocolitis (NEC)
- Infection
- Retinopathy of prematurity (RoP)
I am going to describe each of these.
Hypothermia
- Rapid heat loss
- May contribute to metabolic disorders
- Associated with increased mortality in preterm infants
- Associated with IVH and pulmonary insufficiency
Hypothermia, rapid heat loss, is prevalent in the NICU population, may contribute to metabolic disorders, and can be associated with increased mortality in the preterm infant. It is frequently associated with pulmonary insufficiency and is more likely to occur with lower birth weight infants and if that infant was born via C-section.
One thing I have seen in the NICU for decades is when a baby is trying to regulate and keep warm, they are put in an incubator, which is all well and good. We then take them out of the incubator as they progress to being able to maintain their temperature. They are now in an open crib. Now when we do their feedings, I would say almost 99.9999% of the time. In my colleagues and my experience, we see a decline in feeding. They may have been taking 30 ccs, and now it is less. The infant is saying, "I can do both things, but it just takes a whole lot of effort."
Respiratory Complications
- Respiratory distress syndrome
- Bronchopulmonary dysplasia
- Apnea of prematurity
Respiratory Distress Syndrome
They can have respiratory distress syndrome, which is caused by a surfactant deficiency. Surfactant is a mix of fat and proteins made in the lungs that coats the alveoli and keeps them from sticking to themselves. When the infant exhales, they can do so without having their alveoli stick together creating an easier breathing pattern.
Respiratory distress syndrome is something that a lot of infants will have early on, and the earlier they are born, the more likely. They can present with tachypnea with grunting, retractions, and many things based on this respiratory distress syndrome.
Surfactant is typically made around 24 to 28 weeks in utero. An infant born around 34 weeks typically has adequate surfactant to breathe. In the late '70s and early '80s, artificial surfactant was developed to help preterm infants survive and is still used. Surfactant prevents alveoli from sticking together and helps them exhale comfortably.
Bronchopulmonary Dysplasia
Bronchopulmonary dysplasia is a disorder of the respiratory system caused by treatment for respiratory distress. Bronchopulmonary dysplasia is sometimes synonymously used with chronic lung disease. It is a later respiratory complication from the infant having 28 days of supplemental oxygen. There are various criteria for the diagnosis, but in general, there is scar tissue from the extra oxygen.
Apnea of Prematurity
Apnea of prematurity is in about 25% of the premature population. They stop breathing at various times of the day for up to about 20 seconds at a time.
Respiratory Diagnoses: Impact
- BPD is associated with adverse neurodevelopmental outcomes at 9-12 months and is more prominent in preterm infants with the diagnosis vs those without (Lin et al., 2017)
- Well-documented feeding difficulties (Mizuno et al, 2007)
- Pre-term infants with BPD compared to healthy pre-term infants without BPD had higher respiratory rates with larger decreases in 02 saturation & lower performance on sucking measures (Barlow, 2009)
One study looked at nine to 12-month-olds and adverse neurodevelopment outcomes that were more prominent in preterm infants with PBD than those without PBD. It is also well-documented to be associated with feeding difficulties. Infants need to suck, swallow, and breathe in a coordinated way to feed properly. It makes sense that they would have feeding difficulties if they are working hard to breathe.
Preterm infants with PBD compared to healthy preterm infants without PBD had higher respiratory rates with larger decreases in O2 saturation and lower performance on sucking measures. This is another study that shows that infants with PBD have difficulty breathing, lasting longer than a week or two. This is going to impact all of their function, especially feeding.
Cardiovascular Abnormalities
- Patent ductus arteriosus (PDA)
- Systemic hypotension
- Population-based study revealed premature infants 2x as likely to present with congenital heart defects (higher for anomalies of ventricular outflow tract) (Laas et al., 2012)
Infants with prematurity have cardiovascular-related comorbidities with long-term effects, like patent ductus arteriosus, which we will discuss in a moment. There can also be systematic hypotension or a decrease in blood pressure throughout the infant's function. A population-based study revealed that premature infants are two times as likely to present with congenital heart defects, and they have a higher prevalence for anomalies of ventricular outflow tracts. What I want you to take from this population-based study is that premature infants have a much higher risk of having cardiovascular problems on top of respiratory problems and being in the hospital.
Figure 1 shows patent ductus arteriosus.
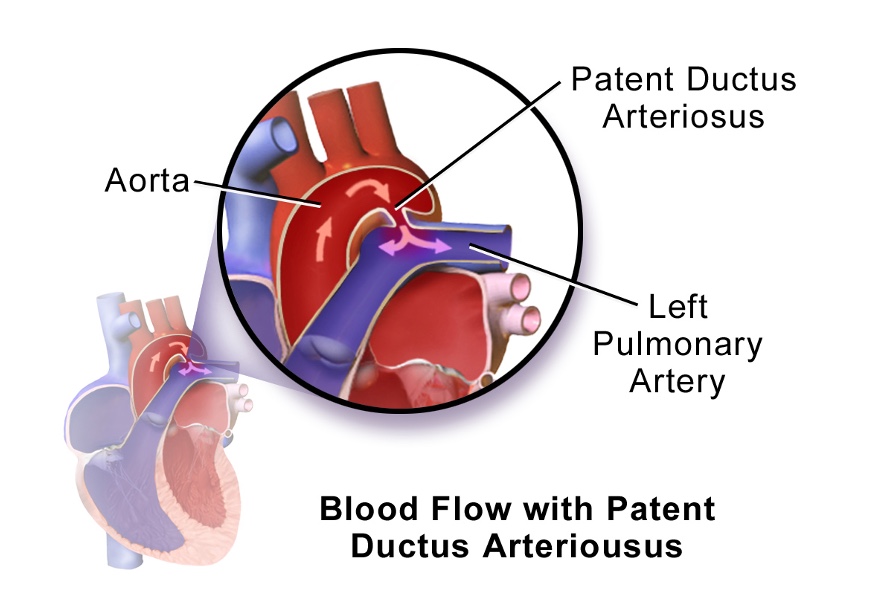
Figure 1. Patent ductus arteriosus. (Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436., CC BY 3.0)
Ductus arteriosus is the most common and least severe heart problem in premature infants. It is the path the blood goes through in utero because the lungs are not in use. Once the infant is born, this path closes after birth, and then the blood flows the proper way and goes through the lungs, where it is oxygenated. However, since these babies are born early, sometimes it does not close as quickly. A physician may have to go in and give medication to encourage it to close, and in a worst-case scenario, they can do a surgical procedure.
Sometimes it is not closed as there are certain congenital heart defects. They will leave this open on purpose because the blood flow is altered. Depending on what those defects are, they may wait.
Cardiovascular Diagnoses: Impact
- Children with CHD have an increased incidence of deficits in intelligence, VMI, and psychosocial functioning (Sterken et al., 2016).
- 1 in 5 children with CHD had delays in multiple domains (Mussatto et al., 2015).
- Predictors of poorer developmental outcomes in the CHD population-longer hospital stay, poorer linear growth, feeding problems, & socioeconomic risks (Mussatto et al., 2015)
- Children with CHD have an increased risk of neurodevelopmental impairments, but intelligence appears to be WNL (Massaro et al., 2008).
Children with congenital heart defects have an increased incidence of deficits. One study found increased deficits in intelligence, visual motor integration, and psychosocial functioning.
Another study showed one in five children with congenital heart defects had delays in multiple domains, and there were predictors of poor developmental outcomes in children with CHD population. They have longer hospital stays, poor linear growth, feeding problems, and socioeconomic risks.
Lastly, children with CHD have increased risk of neurodevelopmental impairments, but this study found intelligence to be within normal limits.
What I would like to point out beyond what the research says is that most parents are not focused on their child's development. This occurred to me one day when a mother said, "I was worried whether my baby was going to live," because the congenital heart defects that her infant had were so severe. If they are worried about their child's medical issues, they may not recall other details.
The other thing is that if you have ever seen an infant after surgery, they are very weak and have gone through so much. It is not at all surprising to me that they are going to have a more challenging time developing in a typical way because they are just trying to survive. Obviously, they will have feeding problems like reflux due to weakness. Our bodies can only do so much.
Intraventricular Hemorrhage
- Most common neuropathological lesion of a preterm infant
- Rarely occurs at birth – typically within the first 3 days of life
- Occurs more frequently in infants born before 32 weeks ega (estimated gestational age)
Intraventricular hemorrhage is bleeding into the ventricles and is most often seen in premature babies, as their blood vessels are not fully developed. Their blood vessels are thinner and fragile. Intraventricular hemorrhage usually does not occur at birth but in the first few days of life. It is a common neuropathological lesion of the preterm infant, and it occurs more frequently in infants born before 32 weeks estimated gestational age.
- Grade I (Mild) Bleeding confined to germinal matrix
- Grade II (Moderate) IVH occupies 50 percent or less of lateral ventricle volume
- Grade III (Severe) IVH occupies more than 50 percent of lateral ventricle volume
- Grade IV (Severe) Hemorrhagic infarction in periventricular white matter ipsilateral to large IVH
Intraventricular hemorrhage involves four levels: grade one, and grade two, grade three, and grade four. The more severe the grade, the more likely we can expect poorer outcomes. However, I have read some studies over the past few years stating that we cannot rule out that infants with grade one or two intraventricular hemorrhages do not have long-term damage. There can be some damage, but it may not be as overt. Certainly, there are severe problems in the three and four levels.
Intraventricular Hemorrhage: Impact
- IVH diagnosis is associated with significantly lower mean psychomotor and mental development indices and increased incidence of CP and visual impairment
- IVH diagnosis born less than 28 weeks gestational age poorer outcomes than those born 28 weeks gestational age or later
- Outcomes worse with grades of IVH
- Lower grades of IVH associated with higher percentages of negative outcomes compared to controls without IVH
- (Klebermass-Schrehof et al., 2012)
The impact of IVH depends on which level. An IVH diagnosis has been shown to be associated with significantly lower mean psychomotor and mental development indices, and an increased incidence of CP and visual impairment.
An infant with an IVH diagnosis that is born less than 28 weeks of gestational age is also going to have poorer outcomes, than those born at 28 weeks of age or later. If you think about what we have talked about so far, an infant at 28 or less is going to have problems with their heart, respiration, and everything.
Outcomes worsen with the grade of IVH. We are going to see much worse outcomes with somebody who has a grade of four over a grade one.
Finally, the lower grades of IVH are associated with higher percentages of negative outcomes as compared to controls.
We used to think there is no problem, but several studies have now shown that is not necessarily true. If you compare them to controls without having any grade of IVH, they will present with some more problems than maybe what was recognizable before.
Necrotizing Enterocolitis (NEC)
- One of the most common GI emergencies in newborn
- Occurs 1 in 3 per 1000 live births
- Ischemic necrosis of intestinal mucosa
Necrotizing enterocolitis is one of the most common GI emergencies in the newborn. It occurs one in three per 1,000 live births. It is ischemic necrosis of the intestinal mucosa. It can occur in the term infant, but it is usually going to occur in a baby that is premature. If it happens in a term infant, it is going to be an infant that has some heart defects or something like that.
The incidence decreases with increased gestational age. You have less likelihood of getting it the longer you are in utero. Figure 2 shows what this looks like. It is necrosis of the intestinal mucosa.

Figure 2. Necrotizing enterocolitis in the baby (RadsWiki, CC BY-SA 3.0<https://creativecommons.org/licenses/by-sa/3.0>, via Wikimedia Commons).
What are some systemic signs?
- Systemic Signs
- Apnea
- Respiratory failure
- Lethargy
- Poor feeding
- Temperature instability
- Hypotension
- Bacteremia
- Abdominal Signs
- Distention
- Gastric retention
- Tenderness
- Vomiting
- Diarrhea
- Rectal bleeding
- Bilious drainage
Systemic signs include apnea, respiratory failure, lethargy, poor feeding, temperature instability, hypotension, and bacteremia, which is bacteria in the bloodstream. For abdominal signs, we may see abdominal distension, gastric retention, tenderness, vomiting, diarrhea, rectal bleeding, and bilious drainage.
I preempted this section with these problems that will impact feeding. However, I think we can all appreciate someone who's going through all of these things, presenting with all of these signs is also going to have their overall development impacted just in the fact that they're in the NICU for a longer a lot of times, and I'll give you a quick story about this.
Infants that have necrotizing enterocolitis cannot eat by mouth because they cannot have their gut being used. They work toward making this child heal before we start trying to feed them. There is a lot of ebb and flow in the recovery of an infant with necrotizing enterocolitis.
Again, it can certainly impact feeding and the child overall.
Necrotizing Enterocolitis: Severity
- Recurrence (4-10%)
- Mortality (15-63%%
- Intestinal Strictures (12-35%)
- Stoma Complications (50%)
- Short Bowel Syndrome (20-35%)
- Neurodevelopmental Impairment (30-50%)
- Growth Delay (10%)
The recurrence of necrotizing enterocolitis is about four to 10%, and mortality is 15 to 63%. You can see co-occurrence of intestinal strictures, stoma complications, short bowel syndrome, and neurodevelopmental impairment and growth delays, which are pretty high at 30 to 50%.
Necrotizing Enterocolitis: Impact
- Premature infants with NEC hospitalized 60 days longer if surgery required and 20 days longer if no surgery than unaffected preterm infants (Neu & Walker, 2011)
- NEC associated with worse neurodevelopmental outcomes than preterm infants without the diagnosis (Rees et al., 2007)
- Advanced NEC with need for surgery increase risk of neurological impairment (Rees et al., 2007)
- Approximately 50% of neonates with NEC have long-term neurodevelopmental problems (Rees et al., 2007)
- Infants with NEC at greater risk for motor impairment (Shah et al., 2008)
Premature infants with NEC are hospitalized for 60 days or longer if surgery is required and not treatable with IV antibiotics. That is 20 days longer if no surgery in unaffected preterm infants. There are also worse neurodevelopmental outcomes in preterm infants with NEC as opposed to those that are preterm. Infants with advanced NEC will need surgery which increases their risk of neurological impairment.
Additionally, about 50% of neonates with NEC have long-term neurodevelopmental problems with a greater risk for motor impairment.
Infection/Sepsis
- Late-onset sepsis (occurring after 3 days of life) – common complication
- Complications associated with increased risk of infection (BPD, PDA, NEC, prolonged intravascular access)
- Associated with longer hospital stays
Late-onset sepsis occurs three days of life. It is a common complication and can be associated with an increased risk of infection. Many infants with NEC, BPD, and some of the things that we have already talked about, will have a higher complication of infection, as it is associated with longer hospital stays.
Infection/Sepsis: Impact
- Higher incidence of CP in children who had isolated episodes of early-onset sepsis and for those who had isolated episodes of late-onset sepsis when compared to those without either
- Higher incidence of CP in children who had both early and late-onset sepsis when compared to those without either
- No association was found between infection and cognitive impairment (Mitha et al., 2013)
What is the impact of infection and sepsis? You see a higher incidence of CP in children who have isolated episodes of early-onset sepsis, even for those who have a later initiation of sepsis when you compare it to children who have no isolated incidents of sepsis.
There is also a higher incidence of CP in children who had both early and late-onset sepsis when compared to those without.
There is no association found in this study between infection and cognitive impairment.
Retinopathy of Prematurity
- Developmental vascular proliferative disorder occurs in the incompletely vascularized retina of preterm infants
- Typically emerges around 34 weeks PMA
- Advances irregularly until 40-45 weeks PMA
- May resolve spontaneously
- May result in vision impairment
It still exists, but it has gotten better over time. It is a developmental vascular proliferative disorder that occurs in the incompletely vascularized retina of preterm infants. It typically emerges around 34 weeks and advances irregularly until about 40 to 45 weeks. It may resolve spontaneously, or it may result in vision impairment.
We did not know this back then, but years ago, they used to put oxygen hoods on these infants. They would load them up with oxygen, but then they figured out that that oxygen was causing retinopathy of prematurity issues. As such, they are very particular about how they use oxygen now. There are also constant eye exams in the NICU.
Vision Impairment (VI)
- VI may result in delays/deficits in motor, linguistic, cognitive, and social-behavioral development (Bartlett et al., 2002).
- VI interferes with gross and fine motor development (Prechti et al., 2001).
- Delay of head control (Prechti, 2001)
- Postural instability until 12-14 months (Prechti, 2001)
- Delay in hands to midline (Prechti, 2001)
- Increased tactile defensiveness
Vision impairment can result in delays, and deficits in motor, linguistic, cognitive, and social-behavioral development. It can interfere with gross and fine motor development and a delay in head control. This study showed postural instability until 12 to 14 months in infants with vision impairment, and it can delay hands to midline, resulting in or contributing to increased tactile defensiveness.
Long-term Complications of Prematurity
- Increased recurrent hospitalizations
- Increased long-term neurodevelopmental impairment
- Chronic health problems
- Growth impairment
- Impairment of lung function
Long-term complications include recurrent hospitalizations, long-term neurodevelopmental impairment, chronic health problems, growth impairment, and impairment of lung function. We are going to look at each one of these a little bit more in-depth.
Increased Recurrent Hospitalizations
- Most common causes
- Respiratory disorders
- Infection & asthma
- Gastroesophageal reflux & gastroenteritis
In the premature population, the most common reasons for recurrent hospitalizations are respiratory disorders. Additionally, we see infection, asthma, and gastroesophageal reflux, and gastroenteritis.
Increased Recurrent Hospitalizations: Impact
- Though weight gain/physical growth/medical stability achieved at time of discharge, child is vulnerable for developmental delays (Catlin, 2008; Pao, Ballard, & Rosenstein, 2007).
- Motor development may be impacted by restricted space.
- Hospitalized children may be further limited by vent or feeding tube dependence and exposure to invasive procedures (Glader & Palfrey, 2009).
- Stress in early childhood, such as frequent hospitalizations, reduces potential for brain growth (Holt & Mikati, 2011).
The impacts of increased recurrent hospitalization are weight gain, physical growth, and medical stability; however, the developmental delay risk is much higher for that person. For instance, motor development can be impacted. This is why I am always an OT wannabe. The OT looks at the interaction of an infant within their own environment to assess how that affects sensory function and fine and gross motor skills.
If this child is in the hospital every two or three weeks, they are going to be stuck in a small space and this is going to diminish the richness of their experiences like the feeling of the couch or dog, seeing familiar home items, smelling what your mom and dad are cooking, and things like that. Motor development is going to be impacted by that restricted space. A hospitalized child may be further limited by being attached to feeding tubes, ventilators, nasal cannulas, et cetera.
Stress in early childhood such as frequent hospitalizations is going to reduce the potential for brain growth. There is a lot of literature out there now talking about how brain architecture is even impacted by the chronic stress experienced by these infants. For example, there was a child I used to see at our local children's hospital. I noticed that every time he came, his nose ran constantly. Every time, I would ask his dad, "Is he sick?" He replied, "The minute we pull into the parking garage, his nose starts to run." He also said, "He's been here a lot, long before he started seeing you." This child was at the hospital as a premature infant and then had multiple repeated hospitalizations during which lots of negative things happened like shots, blood draws, et cetera.
- Although children may not recall events of hospitalization accurately, they may display symptoms of PTSD up to 1-year post-discharge (Rennick & Rashotte, 2009).
- Variation in parent involvement may exacerbate developmental delays/issues.
- Disrupted/limited contact between primary caregiver/child impacts sense of attachment/security (Jaegermann & Klein, 2010).
- Longitudinal studies of institutionalized children reveal attention-seeking behaviors/increased risk of long-term social/behavior delays (Johnson et al., 2006).
Although children may not recall events of the hospitalization accurately, they can display symptoms of PTSD up to one-year post-discharge. And if you think about that little boy, it was well beyond one year.
Variations in parent involvement can exacerbate developmental delays and issues. Sometimes, caregivers cannot be at the hospital the whole time or visit very open due to jobs, other children, and things like that.
This lack of parental involvement can exacerbate any developmental delays or issues and have an impact on attachment and security. Children need homeostasis in order to have attachments. "Can I can trust my parents to take care of me so that I can be big and strong and go out into the world." This is not necessarily going to be the case if you are in the hospital every two weeks, and your parents cannot be there with you all the time.
Longitudinal studies of institutionalized children reveal that attention-seeking behaviors also increase the risk of long-term social behavior delays.
Increased Long-term Neurodevelopmental Impairment
- Impaired cognitive skills
- Motor deficits
- Sensory impairment
- Behavioral & psychological problems
With prematurity, we may also see impaired cognitive skills, motor deficits, sensory impairment, and behavioral and psychological problems. Again, this risk increases every time the gestational age goes down. For instance, an infant born at 24 weeks is going to have a greater chance of neurodevelopmental impairment than a child born at 34 weeks.
Neurodevelopmental Impairment: Impact
- General motor movement at term (equivalent) predictive of feeding problems at 12 mths (Sanchez, et al., 2017).
- Feeding problems more common in children with lower cognitive, language, and motor scores on Bayley III (Crapnell et al., 2015).
- Feeding problems more common in children with higher internalizing domain scores, depression/withdrawal, and anxiety scores on Bayley III (Crapnell et al., 2015).
- Oropharyngeal dysphagia linked to gross motor severity using GMFCS but present across all levels (Benfer et al., 2013)
Here are some studies that support some of these symptoms. General motor movement at term is predictive of feeding problems at 12 months. Additionally, feeding problems are more common in children with higher internalizing domain scores for depression, withdrawal, and anxiety on the Bailey.
Oropharyngeal dysphagia, difficulty chewing, swallowing, and managing food in both the oral and pharyngeal phase of the swallow, is linked to gross motor severity using the GMFCS but is present across all levels. This makes sense if the infant cannot sit up or does not have good postural stability. This is going to impact their ability to have safe oral and pharyngeal phases of the swallow.
Chronic Health Issues
- Children with special health care needs are at risk for range of poor psychosocial and educational outcomes (Forest et al., 2011).
- Pulmonary abnormalities are more pronounced in children with preterm birth and h/o moderate to severe BPD (Baraldi et al., 2009).
- Circular pattern-feeding and swallowing problems can result in chronic pulmonary or constipation problems which further impact intake (Adams et al., 2014).
Children with special healthcare needs are at risk for a range of poor psychosocial and educational outcomes. Pulmonary abnormalities are more pronounced in children with preterm birth and a history of moderate to severe bronchopulmonary dysplasia. The circular pattern of feeding and swallowing problems can result in chronic pulmonary problems or constipation, which can then further impact intake.
Think about this in context. A child is chronically ill with a lot of special healthcare needs reducing their interaction in their home, preschool, and daycare. On top of that, you add breathing, feeding, and swallowing problems. You can see how this becomes a vicious cycle of problems.
Long-Term Health & Educational Needs
- Neurodevelopmental impairment affects 35-50% school-age children born very preterm (Johnson, et al., 2009).
- Cognitive scores are 11-12 points lower than terms peers (Kerr-Wilson et al., 2012).
- Fine motor & gross motor deficits (deKieviet et al., 2009)
- Visual-motor integration deficits (Geldof et al., 2012)
Neurodevelopmental impairments affect 35 to 50% of school-aged children who were born preterm, and cognitive scores are 11 to 12 points lower than term peers. Fine motor and gross motor deficits were also documented in this 2009 study. Finally, the 2012 study also documents visual motor integration deficits.
The Premature Infant: Early Experiences
We went through some of the long-term and short-term co-occurring diagnoses and those impacts. Let's now look at the early experiences.
Overall Experience
- Born with immature brain/nervous system, GI system, respiratory system
- Early life in a NICU
- Atypical types of stimulation/pain/interaction
- Cues difficult for caregivers to comprehend
Preemies are born with immature brains, nervous, GI systems, and respiratory systems. They also have an early life in the NICU. Think about your infants or an infant in your family. They come home and everything is about them, including typically a well-laid-out nursery.
In contrast, a premature infant lives in the hospital with atypical stimulation. Instead of parents and other caregivers holding and rocking them, they may be in an incubator exposed to more painful stimuli. Their cues are also difficult to comprehend because caregivers change. Additionally, as just mentioned, caregivers are not with them 24 hours a day.
Stress and the Premature Infant
- Stress becomes an issue when equilibrium is pushed out of balance due to the environment causing bodily/mental tension.
- Stress during early development associated with long-term changes in neurobehavioral development.
- Stress to trauma - "the result of exposure to an inescapably stressful event that overwhelms a person's coping mechanism” (Van der Kolk, 1997).
- Stress reduction is a goal of intervention before term age (Hadders-Algra, 2011).
Stress becomes an issue when that equilibrium is pushed out of balance due to the environment causing bodily and mental tension.
Stress during early development is associated with long-term changes in neurobehavioral development.
Stress turns to trauma when exposure to inescapable stress overwhelms someone's coping mechanism.
Stress reduction is a goal intervention before term age, but does it always happen? Absolutely not. NICUs have gotten so much neurodevelopmentally-driven over time. As an example, I can remember when I first started in the NICU in 1998-ish. There was so much noise like loud voices and dropping of metal things on the floor. Many NICUs have progressed from that to a quieter environment. You also see kangaroo care interventions and other positive changes in the environment. That being said, there is still a level of stress in the environment like monitor sounds and multiple people touching throughout the day.
I overheard one of the nurses talking about babies with neonatal abstinence syndrome, where they are born addicted to opioids. They cry a great deal. To deal with this, they created a quiet room. Nurses could take 15-minute breaks in this room to get away from the crying. We also need to consider the stress on the infants. They may also need quiet to be able to get it together.
Neuroprotection
- Rapid change in the brain last trimester (Buss et al., 2012)
- Period of dendritic growth, synaptic connections, apoptosis, myelination, and pruning (Shaker, 2017)
- Simultaneous actions for preterm infants in NICU 1. Becoming a feeder, 2. Developing sensory/motor pathways (Shaker, 2017)
- Pathways that are created (positive & negative) are reinforced (Shatz, 1992)
- Stress activates “fight/flight”-the release of stress hormones (Smith & Vale, 2006)
- Repeated stress can alter brain structure/neurobehavior (Smith et al., 2011)
There are rapid brain changes in the last trimester. There is a period of dendritic growth and synaptic connections. There are also simultaneous actions for the preterm infant like becoming a feeder, developing sensory-motor pathways, and keeping up their body temperature.
They have both positive and negative pathways being created. They have fight-or-flight responses when they feel pain, and that is going to inhibit a lot of their development because they will shut down everything.
- Repeated stress/altered pathways impact feeding in NICU and after discharge (Shaker, 2013).
- Repeated stress associated with feeding/altered pathways can result in later refusal to feed (Shaker, 2013).
- Positive response by caregivers to infant communication and avoidance of negative feeding experiences target cue-based (Shaker, 2017)
Repeated stress has been shown to alter brain structures and neurobehavior over time. The therapists in the NICU are incredibly driven toward neuroprotection interventions as a result.
Repeated stress is also going to impact feeding in the NICU and long after discharge. You may see a later refusal to eat because everything has been very negative early on.
Thus, positive caregiver responses to infant communication and avoidance of negative feeding experiences are absolutely critical.
Importance of Feeding in the NICU
- The most frequent cause of delayed discharge from NICU is reaching full feeds.
- Infants born earlier than 28 weeks ga, extremely low birth weight, complex medical diagnoses at greater risk for delayed full feeds
- The degree of medical complexity/number of diagnoses closely correlates with a longer time to reach full oral feeds
(Jadcherla et al., 2010)
Feeding is one of the most frequent reasons for delayed discharge. I cannot tell you how many babies I have seen over the years that are keeping on weight and have stable temperatures but cannot complete full feeds yet. Due to this, they are stuck in the NICU. Babies born earlier than 28 weeks, with extremely low birth weight and complex medical diagnoses, are delayed in their feeding initiation.
The degree of medical complexity correlates with a longer time to reach oral feeds. This sets up a situation for pressured feeding when everybody says, "When the infant learns to eat, you can go home." However, do not forget. If they have co-occurring issues like bronchopulmonary dysplasia, cannot breathe well, or have a heart problem, feeding is not going to be a positive experience. It is all reflexive at this point and dependent on many factors.
Feeding Comparison
- Volume Driven
- Volume/time based
- Risk oral aversion
- Risk-negative physiological impacts
- Risk-poor model for parents
- Neurobehavior/brain structure at risk
- Co-Regulated/Cue-Based
- Infant is active participant in collaboration/guides (Shaker, 2017)
- “Being fed becomes being supported to feed”
- Feeding begins with hunger cues and ends with satiation cues.
Feeding can be volume-driven or co-regulated/cue-based. We want to see co-regulated, cue-based. Volume-driven is volume and time-based. Every three hours, the infant is going to get 30 ccs of formula or the mother's breast milk whether they like it or not. This causes oral aversion, negative physiological impacts, and risks for poor modeling for parents affecting brain structures and neurobehaviors.
This being said, if an infant is preterm, the team will calculate what the infant needs and until the child can regulate, they will require set volumes and set times for feeding. Once infants can stay alert and are more stable, they can be active participants. We want to see the infants' cues like rooting and their hands in their mouths prior to being fed. Feeding begins with hunger cues and ends with satiation cues.
Often, I also do not see a consistent change in behavior when that infant starts to say, "Stop, I've had enough." I often see caregivers ignoring satiety cues because they want the infant to gain weight and feed. Certainly, we do if the infant needs a moment to get reorganized, but we do not always tap into their cues. About 50% of parents in the NICU report that their child has food aversion at 18 to 24 months if that tells you anything.
Examples of Stress
- Autonomic Stress
- Bradycardia
- Sneezing
- Yawning
- Gagging
- Tremors
- Motor Stress
- Flaccid tone
- Hyperextension
- Grimacing
- Finger splaying
- Arching
- State-Related Stress
- Diffuse sleep/awake states
- Eye aversion
- Irritability
- Crying
- Staring
Examples of distress that we might see during feeding with an infant include bradycardia, where the heart rate drops below 100 beats per minute, flaccid tone, and eye aversion. They are not going to make eye contact with you and look away. They may also show hyperextension, grimacing, and other things that say, "I don't like what's going on here, and I need it to stop." They may need to reorganize or stop altogether, but sometimes that does not happen. We want to make sure that we change this behavior so that there are no long-term negative effects.
Prematurity: Impact on Caregivers and Family
Maternal Experience
- Birth transitions from a natural process to a crisis
- Crisis results in negative emotions
- Grief and guilt
- Early attachment impacted by high-tech environment
- Infants less able to interact
Birth transitions from natural processes are ideal. The natural process is you go in, have a baby, the baby comes in the room with me, and then you go home. Often, instead, it is a crisis situation. They come early, the nursery is not done, and the child has a health issue, like a cardiac deformity. There can be concerns about whether the child is going to live. How are you going to navigate extended hospitalization with a job and other children? ICrisis results in a lot of negative emotions or it can. Grief and guilt. Why did this happen to me? Why did my baby come early?
Early attachment is impacted by the high-tech environment. I want to sit in my nursery with my baby with a lamp on and talk and read to them, but instead, I am in a nursery that is louder with many other people and professionals. I cannot touch my baby when I want, and the infant is much less able to interact due to medical issues and equipment. The maternal/paternal experience can be very different.
Parent Perceptions
- Parent/provider partnerships in NICU/PICU –conflict, communication problems, lack of collaboration (Lutz, 2012)
- System barriers/financial concerns escalated parent distress & expectations violated in comparison to “normal” families (Lutz, 2012)
- Mothers vs. fathers in NICU – more stress (Pallas et al., 2012), increased change to (her) daily routine (Clottey & Dillard, 2013), more guilt, role damage (Lindberg & Ohrling, 2008)
- Fathers reported overall higher stress levels/mothers reported more health-related problems, more depression, social isolation, and role restriction (Howe et al., 2014)
- Parents with preterm infants continue to report more stress than those with term (Howe et al., 2014).
Some articles talk about parents' perceptions of the NICU like conflict, communication problems, and lack of collaboration. This is getting better, but this was back in 2012.
Some parents mentioned system barriers and financial concerns which increased their distress, as compared to "normal" families.
Moms and dads in the NICU said they had more stress, increased changes to their daily routine, more guilt, and their roles as parents were damaged.
Fathers reported overall higher stress levels, while mothers reported more health-related problems and depression.
Parents with preterm infants continue to report more stress than those with term infants, even after the NICU. When you think about the comorbidities and the co-occurring diagnoses, this makes sense.
Family Support
- Empathize family experience
- Provide opportunities for families to share their feelings/needs
- Assist with the identification of support systems
- Advocate
- Encourage healthy coping strategies
We want to empathize with the family experience and provide opportunities for the families to share their feelings. We can also assist with the identification of support systems, advocate for them, and encourage healthy coping strategies.
Here is an example. I was talking about a specific genetic diagnosis while teaching a feeding class to professionals in Florida. A parent came up and said, "I just wanted to thank you for talking about this particular diagnosis today." I replied, "You're welcome." She went on to say, "My infant had this diagnosis, and she he passed away at six months." She said, "I can't tell you how many therapists came to see her who didn't know what her diagnosis was. And if they knew what the diagnosis was, they didn't take the time to look up the ramifications." I have had other people say similar things. Probably the first and best way that we can help is by understanding what their child has gone through and how it is very atypical of what they expected or wanted.
Questions and Answers
Why is prematurity higher in the US than in other countries?
It is actually not higher in the US than in other countries. In fact, I was listening to something earlier that talked about it being fairly high in Great Britain, and I was a little surprised.
How much does gestational dating matter?
It is helpful to determine developmental milestones, but it is not a specific science in itself.
What does it mean to reorganize?
If I am feeding a baby, and they start to get a little discombobulated or dysregulated because their stomach is hurting or they are trying to breathe, then I will reorganize them by trying to take any stress away. I might say, "Okay, you're having a hard time with this bottle right now. Let me take the bottle out because it's too much for you. You're swaddled. Let me give you a few minutes to breathe. Let me give you your pacifier," if that baby's taking a pacifier.
I have seen a lot of the OTs rock the infant or do other things to get the infant back to a regulated place.
What if the father was a premature baby? Does that increase chances?
I do not know the answer to that question, but it is a very good question.
Have you seen all disciplines working together with the premature baby and family in the NICU or just OTs and SLPs?
At the children's hospital where I worked for about 12 years, we had all three disciplines in the NICU. It was large with 120 beds with some of the units for older NICU babies that stayed with us, like those with necrotizing enterocolitis. We had one little one that stayed with us until she was almost 18 months.
PT tended to work more with the older infants than they did with the younger infants and OTs and speech more with the younger infants. Although I know in some NICUs, that is not the case, and PT does as much as the others.
The NICU that I am in now is much smaller, and we just have OT and speech for the most part.
Do African American women have a 50% increased chance of premature babies even when all the other differences are the same?
What I was sharing with you earlier is based on just a couple of studies that I read. One study said that when a mom is Black, she has a 50% increased chance of premature delivery, regardless of socioeconomics.
Why is prematurity at a higher risk of intraventricular hemorrhage?
They are born with much weaker, less well-established systems.
Are there any studies relating to the father's emotional journey or stress?
Yes, there are. I mentioned one about moms and dads. I am sure there are probably more recently.
How long would it take for a premature infant to recover 100% despite having neurological impairments, and how much does it impact development?
A premature infant is an individual first. If an infant is born at 28 weeks gestation and has congenital heart defects, neurological side effects, or whatever the case may be, they may not function in a typical way. That being said, one of the first babies that I ever worked with was born 24 weeks, and no one told her. She is about 17 or 18 now, and she still does not eat very well, but it is more of a gut issue.
Is prematurity more prevalent with in vitro fertilization?
I have heard different thoughts on that. Many times, in vitro, will result in multiple births, and therefore, there can be a higher incidence of prematurity. The other reason is if someone has to use in vitro, there's potentially a reason why they have to go that route, which can be associated with why then that infant is delivered prematurely.
References
See additional handout.
Citation:
Williams, R. M. (2023). Overview of prematurity and associated conditions. OccupationalTherapy.com, Article 5595. Available at www.OccupationalTherapy.com
