Editor's note: This text-based course is a transcript of the webinar, Polyvagal Theory Utility In Pediatric OT, presented by Maude Le Roux
OTR/L, SIPT, CTC, ADHD- RSP, and Lara Taggart EdD, OTR/L.
*Please also use the handout with this text course to supplement the material.
Learning Outcomes
- After this course, participants will be able to differentiate between the concepts of sensory modulation and neuroception as they apply to detecting strength or safety in different environments.
- After this course, participants will be able to compare the bottom-up approach of interoception to working top-down through cognitive understanding to create internal well-being.
- After this course, participants will be able to distinguish 3 key concepts of PVT and their application through various practical activities to support activities of daily living, including social relationships.
Introduction
Lara: Thank you for being here. Today, we are going to talk about polyvagal theory, the controversy surrounding it, and how we can conceptualize it as we engage in our work with children, families, and adults who have experienced trauma.
I am also excited to be a new board member for the ATTACh organization. If you are interested, we have a website, ATTACh.org, where Maude has created a space for OTPs who want to engage in trauma-informed care work.
What is Polyvagal Theory (PVT)?
Let’s begin by discussing polyvagal theory. This theory was developed by Stephen Porges in the 1970s and 1980s and presented to the clinical world in the 1990s. It is a theory about the autonomic nervous system and its connection to emotional regulation. Three organizing principles serve as a foundation as we discuss polyvagal theory, which I will call PVT.
One of the organizing principles is co-regulation. This is the idea that we naturally and unconsciously send signals of safety or danger to each other, encouraging or discouraging psychological or physical distance or proximity. Porges talks about this in terms of social engagement behaviors. Under PVT, co-regulation refers to the social engagement system operating at a subcortical, physiological level. We will discuss this later, particularly the neural pathway emerging from one of our cranial nerves—the wandering vagal nerve complex. We will also discuss how the vagal nerve is divided into ventral and dorsal parts. This division explains our reactions to threats while considering facial expressions, head movements, and vocal intonations that communicate openness to friendly interaction.
Another organizing principle Porges coined is neuroception. He created this term to differentiate it from what we traditionally know as perception. Perception involves the cortical part of our brain, particularly the parietal cortex in the sensory-motor area, helping us understand and make meaning of sensations. Porges wanted a term that stayed away from the cortical area and instead described subcortical structures or the autonomic nervous system (ANS). He defines neuroception as the detection of risk without conscious awareness.
Building on this, he elaborates on how the autonomic nervous system continuously interprets risk information transmitted by the sensory systems throughout the body. Before Porges, research already supported the autonomic nervous system’s role in fight-or-flight and rest-and-digest responses. However, Porges highlights that the ANS includes a built-in surveillance system that constantly discerns risk without involving the thinking parts of the brain.
Neuroception scans other people, our bodies, and the environment for safety or danger cues. We will later discuss how trauma can distort neuroception, leading individuals to misinterpret safe situations as dangerous or, conversely, perceive danger as safety. We know that individuals with a history of severe adversity might become habitually hypervigilant, always anticipating threat. In addition to optimizing risk detection and preparing for defense, they might habitually seek out risky behavior to maintain a chronic state of heightened sympathetic arousal. For them, being in a fight-or-flight state feels more normal than being regulated. If you visit Porges' website, you will find assessments he uses to examine neuroception.
Another component, which we will cover in more detail in a few slides, relates to the PVT controversy. Porges introduces the idea of a hierarchy within the autonomic nervous system. Before diving into that, let me briefly overview the relevant neuroscience, one of the subjects I teach at my university.
We know there is a peripheral nervous system in addition to the overarching nervous system, which is divided into the central and peripheral systems. Further dividing the peripheral nervous system, we find the somatic nervous system, which controls voluntary movements. The somatic nervous system consists of somatic motor and sensory components. Sensory neurons from our skin, muscles, and joints transmit signals to the brain, while motor neurons signal our skeletal muscles to initiate voluntary movements. Alongside the somatic system, we have the autonomic nervous system, which governs involuntary functions such as heart rate, digestion, respiratory rate, and glandular activity.
The autonomic nervous system is further divided into the sympathetic nervous system, which prepares the body for stress and emergencies (called fight or flight), and the parasympathetic nervous system, which promotes relaxation and recovery (rest and digest). There is also the enteric nervous system, which governs the gastrointestinal system. These divisions allow the body to perform voluntary and involuntary activities, helping us maintain homeostasis and respond appropriately to internal and external stimuli.
PVT examines the autonomic nervous system through a hierarchical lens, proposing that, based on this framework, predictable patterns of disconnection, mobilization, and engagement exist.
The major cranial nerve involved in the parasympathetic system is the vagus nerve. In the context of the autonomic nervous system and Porges' theory, we still recognize the sympathetic nervous system as responsible for our fight-or-flight response. However, Porges subdivides the parasympathetic nervous system into the ventral and dorsal vagus nerves. He describes the ventral vagus as associated with engagement, while the dorsal vagus is linked to disconnection.
Through this process, we now have these three principal states, an evolution of the mammalian ANS.
Ventral Vagal (Social Engagement/Safety)
Sympathetic (Mobilization/Activation)
Dorsal Vagal (Immobilization/Collapse)
These states—whether ventral vagal, which represents engagement; sympathetic, which means mobilization; or dorsal vagal, which represents disconnection—form the underlying neurophysiological foundation for our feelings and emotions. Although they are often presented as distinct, these states are not truly independent. Sometimes it may feel that way based on how they are described, but that is not the point. Porges talks about blended or hybrid states, emphasizing a continuum of behavioral reactions ranging from immobilization to mobilization, depending on whether the context is perceived as safe or threatening.
The process Porges outlines shows an evolution of the mammalian autonomic nervous system, resulting in these three principal states. This evolutionary lens helps us understand how these systems interact and influence our emotional and behavioral responses. A polyvagal-guided approach to therapy builds naturally on this foundation and fits very well with how we address recovery, trauma, and resilience at Childhelp.
At Childhelp, we work from three primary platforms: first, creating safety and stability; then, engaging in trauma processing; and finally, fostering resilience. These phases are not strictly hierarchical and tend to ebb and flow with each child and family’s needs, but together they form the backbone of our approach. Conceptually, polyvagal theory aligns beautifully with this model, especially in its emphasis on building safety and stabilization as the starting point for healing.
Polyvagal theory reshapes how we view the autonomic pathways and how they relate to therapy. Regardless of our theories or models, we constantly engage with our clients’ nervous systems. From the perspective of the nervous system, we are continually scanning for safety or danger cues. This is not an abstract concept; it is grounded in science. Porges emphasizes that understanding the nervous system empowers us to see that we can influence emotions, feelings, and actions through the plasticity and adaptability of the autonomic system.
When we encounter clients whose nervous systems are locked into survival mode, we witness adaptive survival responses that have become automatic and deeply rooted subcortically. The autonomic nervous system starts to shape their experiences of safety or danger, limiting their flexibility and connection. If these patterns are not addressed, they can solidify into habitual autonomic responses that limit engagement and growth.
Looking at trauma through the lens of the autonomic nervous system helps reduce shame. It reframes survival behaviors as biologically driven adaptations rather than character flaws. This perspective creates more space for curiosity and compassion, allowing the therapist and client to explore autonomic safety and danger cues. Deb Dana, a key follower of Porges’ work, describes moments of regulation as "glimmers," or small signs that the system is moving toward safety.
The ability to recognize and regulate states of autonomic activation is fundamental to the therapy process. It shifts the view that emotional responses are purely cognitive choices and frames them as biologically driven phenomena. This framework helps us stay empathetic and reinforces the belief that positive change is always possible because of neuroplasticity.
Clients often come into therapy with a compromised ability to regulate their activation states. According to polyvagal theory, the capacity to adapt to a changing environment—the ability to rupture and repair—relies heavily on the autonomic nervous system. We see this disruption clearly in trauma survivors, where the survival patterns have become deeply ingrained and stuck.
Using polyvagal theory as a psychoeducational tool, we recognize that early and repeated relational interactions help shape the tone of the autonomic nervous system, creating what can be thought of as an autonomic profile. Through this lens, we start to see patterned emotional and behavioral responses not as deliberate choices, but as outcomes of autonomic development and adaptation to earlier experiences. Deb Dana emphasizes that our focus should not be on what happened to a client, because we cannot change the past, but on how to reshape the nervous system to open new pathways for connection and regulation.
Much of the work with polyvagal theory aligns beautifully with the occupational therapy concept of therapeutic use of self. In OT, through our understanding of sensory integration and sensory processing, we recognize that co-regulation always comes first. Through co-regulation—someone helping us regulate—we eventually learn to self-regulate. When caregivers are unavailable or dangerous, clients often develop survival-based self-regulation strategies that are ultimately ineffective and even harmful to their overall well-being.
In therapy, we assess whether the autonomic nervous system is flexible or if chronic dysregulation rooted in a survival state exists. This understanding becomes essential as we plan and adjust our interventions, always aiming to create the conditions for flexibility, engagement, and eventual self-regulation.
That was a lot of ground to cover, and now we are ready to explore the neuroscience behind all of this.
Vagus Nerve
As I mentioned, the vagus nerve is the most significant part of the parasympathetic nervous system. So, of course, PVT emphasizes the vagus nerve as a central concept in polyvagal theory (See Figure 1).
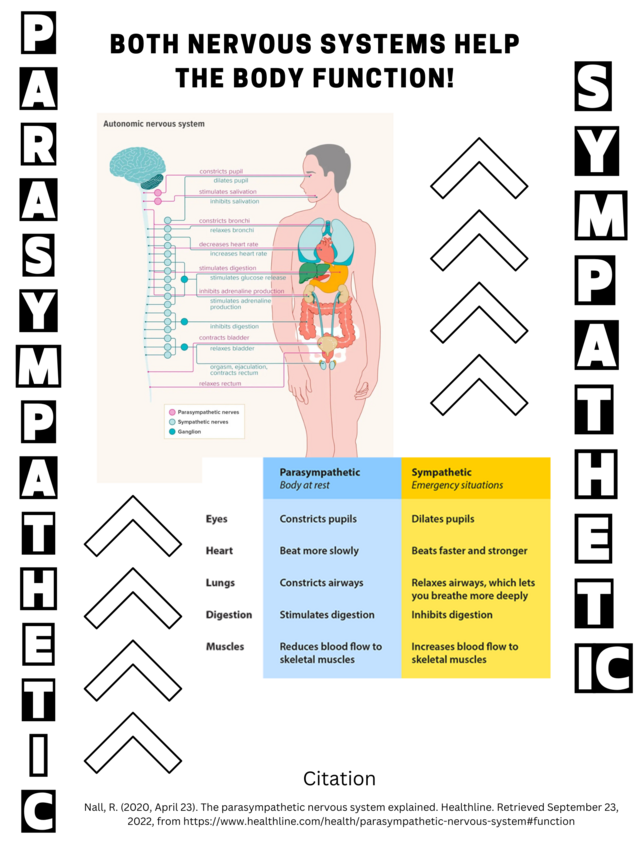
Figure 1. Parasympathetic vs sympathetic systems (Click here for enlarged version.)
When we think about the vagus nerve, it helps us return to neuroscience and neuroanatomy. We know there are different types of nerve fibers. In the somatic nervous system, which is one part of the peripheral nervous system, we have motor fibers that go to our skeletal muscles, which we call somatic motor fibers. We also have sensory fibers that go to the skin for pain, temperature, and touch, called somatosensory fibers. In addition, we have sensory fibers that go to the joints, muscles, and tendons, providing proprioception.
We also have autonomic nervous fibers, often referred to as visceral fibers. These include motor fibers that innervate smooth muscle, cardiac muscle, and glands. We also have visceral sensory fibers that carry sensory information from smooth muscle and cardiac muscle back to the brain, often through stretch receptors. This visceral sensory information is called interoception because it involves sensing the body's internal state.
What is fascinating about the vagus nerve is that it carries all of these types of fibers. It has somatic motor fibers, providing voluntary control to muscles like the larynx and pharynx. It also has visceral fibers, the primary cranial nerve associated with the parasympathetic nervous system. To clarify, sympathetic and parasympathetic fibers are motor neurons; parasympathetic fibers originate from cranial nerves or the sacral area of the spinal cord, and sympathetic fibers come from the thoracic-lumbar area through the sympathetic chain to reach their target organs. Additionally, the vagus nerve has somatic sensory fibers, providing sensation from regions like the external ear and parts of the throat.
The vagus nerve is crucial for regulating many involuntary body functions and is a key player in the parasympathetic nervous system. It influences heart rate, digestion, respiratory rate, mood, and even immune function. It represents the main component of the parasympathetic nervous system and oversees many essential functions.
I want you to start getting into the spirit of PVT, while also grounding it in what we know to be true. Using this, I want to help you better understand the distinction between the ventral and dorsal vagal areas, which is part of Porges' hierarchical ladder.
The sympathetic nervous system is more familiar to most of us. It governs the fight-or-flight response. If you place your hand over your shoulder and think about your thoracic area, around the upper part of your scapula, near T4, and then move your hand to your pelvis, where the lumbar spine is, that region represents the area where the sympathetic nervous system fibers emerge. Sympathetic chains exit and synapse from the thoracic and lumbar spine before traveling to the organs. This provides a way to imagine the sympathetic nervous system's anatomical layout physically.
Now, we shift to the parasympathetic system, specifically the vagus nerve, and see how Porges differentiates it. If you place your hand where the bottom of your jaw and your ear meet, at the base of the occiput, you're roughly over the medulla, where the vagus nerve originates in the brainstem. Then, if you place your other hand over your heart, this represents the territory of the ventral vagus.
Keeping one hand at the base of the skull by the ear and jaw where the brainstem lies, move your other hand from your heart down to your abdomen. This lower territory represents the dorsal vagus. In Porges' theory, the division is related to the diaphragm: above the diaphragm (the area from the base of the skull to the heart) is considered ventral vagal territory, associated with connection and engagement, while below the diaphragm (from the heart to the abdomen) is considered dorsal vagal territory, associated with immobilization.
The idea is that the energy landscape of these two regions—the ventral vagus supporting connection and the dorsal vagus supporting immobilization—offers a new way to understand how our autonomic responses shape our behaviors and experiences.
Controversy of PVT
This is where we start getting into some of the controversy, because even today, the brain remains a largely mysterious and not fully understood structure. That uncertainty naturally carries over into theories like PVT. The vagus nerve, often referred to as the "wanderer," is the primary parasympathetic branch, and Porges’ innovation was to divide it into the dorsal and ventral vagal systems. He then extrapolates that PVT reflects this division as a way of understanding illness and wellness. In this model, illness results from a dysregulated nervous system, while wellness reflects a nervous system guided by the ventral vagus, the branch associated with connection and safety.
Moving into the controversy surrounding PVT, I will share a link later that outlines some of the main criticisms of Porges' theory and how he has responded. There are many criticisms, but I will highlight just two major ones. (I realize I made a small error in the slides, so if you're following along, please swap slides 11 and 12.)
The first criticism concerns the evolutionary claims. Porges describes the dorsal vagal system as the most ancient, arising around 500 million years ago, with the sympathetic system developing later, and the ventral vagal system emerging even more recently. However, critics argue that there is no solid evidence for this claim of a more primitive center of the brainstem evolving into a newer system. Porges counters that cardioinhibitory vagal neurons, which act somewhat like biological pacemakers, have been reliably documented in vertebrates and are located in the dorsal motor nucleus of the vagus nerve in the medulla. Over evolutionary time, he believes, these cardioinhibitory neurons migrated ventrally. Deb Dana, who often teaches about PVT, sometimes refers to this newer ventral vagal system as the nucleus accumbens.
This is where things become a little controversial. Although the vagus nerve undeniably originates in the medulla’s dorsal motor nucleus, the nucleus accumbens is not located there. Instead, it sits in the forebrain, in the basal ganglia, specifically within the caudate nucleus and putamen. The nucleus accumbens is critical in the brain’s reward system, motivation, pleasure, and reinforcement circuits. It is anatomically and functionally distinct from the medullary vagal structures. This mismatch raises essential questions about whether a newer ventral vagal system exists, as Porges describes it.
The second controversy relates to Porges' concept of the "ladder." Some critics argue that the ladder oversimplifies human emotional and physiological responses. We've seen other simplified frameworks used before, like the Zones of Regulation, the Alert Program, and Dan Siegel’s "Flip Your Lid" model. While these models can help teach and conceptualize complex ideas, they can also unintentionally create misleading impressions.
The ladder metaphor can imply that higher is better—reaching the top (the ventral vagal state) is the goal—and that being lower on the ladder (in sympathetic or dorsal states) is inherently negative. This introduces a kind of value judgment about biological states. In reality, each state has value and a purpose. For instance, mobilization through the sympathetic system is vital when there is a real threat; immobilization through the dorsal system can be protective when there is no other way to survive.
Deb Dana and others working closely with Porges carefully emphasize that the goal is not to reach and remain at the top of the ladder, but to develop the flexibility to move up and down as needed. Flexibility is key—not being rigidly stuck in any one state. The true intention behind the ladder metaphor is to provide a way of visualizing how we shift between different physiological states, not to judge one as better than another.
When thinking about the ladder in the spirit of PVT, the ventral vagal pathway is associated with normal heart rate, normal muscle tone, and states of relaxation, engagement, creativity, and hopefulness. The sympathetic system, associated with mobilization, shows increased heart rate, blood pressure, hormone levels, and muscle tone and can manifest as stress, anxiety, worry, panic, or avoidance. The dorsal vagal state, associated with immobilization, reflects low heart rate, low muscle tone, and low energy, and may be experienced as depression, unhappiness, loneliness, or hopelessness.
While these descriptions make it seem like being in the ventral vagal state is ideal, the heart of PVT is not about valuing one state over another. It is about recognizing the biological purpose behind each state and building the ability to move fluidly between them as needed.
Break Out of Mindset of the Hierarchy
When I created the last couple of slides about breaking out of the mindset of a strict hierarchy, I wanted to introduce the idea that Porges and others also talk about hybrid or blended states. Let me explain what that means. You can be in a dorsal vagal state, but if your ventral system—your system of connection—is still online, the experience of immobilization can feel very different.
For example, if you are ventrally anchored, moving into a dorsal vagal state doesn't have to feel like loneliness or unhappiness. Instead, it might feel like quiet moments of reflection or deep intimacy. Similarly, if you are ventrally anchored and shift into a sympathetic state, it can manifest as positive experiences like play, dance, sports, or energized performance. However, when you are not ventrally anchored, you are more likely to get stuck in those states—stuck in the ladder, so to speak.
It becomes about the quality of the experience. Even sympathetic activation can feel thrilling and joyful rather than anxious or overwhelming when ventrally anchored. Without that ventral anchor, we risk feeling trapped in hyperarousal or shutdown. Deb Dana uses the term "ventrally anchored" to describe this steady foundation that allows blended states to be more positive and adaptive.
These blended or hybrid states reflect the complexity of real-life emotional experiences. They move beyond a simple good-versus-bad appraisal and allow us to see how our nervous systems can move fluidly, creatively, and adaptively through different states depending on context and need.
Another essential idea is that social connection is a marker of a ventral vagal state. However, it is critical to recognize that not everyone expresses social connection similarly. Before engaging socially, I often need time alone to rest, recharge, and let my guard down. I need quiet solitude to fill my cup before I can show up fully for a work party or another social gathering. Without that time alone, social connection becomes much harder. If we take polyvagal theory too simplistically, we might miss these important nuances, but I feel that Porges and Dana address these variations in how people connect.
Within the hierarchy, some people worry that PVT might lead to a kind of cognitive appraisal—labeling parts of the nervous system as good or bad. There could be a temptation to think in terms of "having a good nervous system" or "having a bad nervous system," depending on how easily someone connects or mobilizes. However, I believe the deeper intention behind this work is the opposite: not to judge the nervous system, but to use an understanding of it as a pathway toward becoming non-judgmental.
That spirit of curiosity, compassion, and flexibility is at the heart of what PVT invites us into, even amid the controversy and the valid critiques.
The Utility of PVT
Before I turn this over to Maude and whatever beautiful insights she has to share, I want to leave you with a final reflection on the utility of polyvagal theory. For me, its most significant value is as a conceptual framework. Suppose anything I have said resonates with you, especially knowing that the neuroscience of the autonomic nervous system is well established. In that case, polyvagal theory can help conceptualize our work.
Before Maude dives deeper into neuroception, interoception, and related concepts, I want to circle back briefly to sensory receptors. We know there are different types. Exteroceptors detect stimuli from the external world and include our somatic senses like touch, temperature, and pain, as well as the special senses such as vision, hearing, and smell. Proprioceptors are found in muscles, tendons, the utricle, saccule, and semicircular canals, providing information about body position and movement. Then we have interoceptors, the visceral sensory receptors, which detect internal sensations from organs like stomach pain, bladder fullness, or feeling hungry.
This is all rooted in well-established neuroscience. When we think about the autonomic nervous system, especially the parasympathetic system, we know the vagus nerve plays a dominant role, along with some parasympathetic fibers originating from the sacral region of the spinal cord. Parasympathetic fibers, primarily motor neurons, extend from cranial or sacral areas and activate organs to promote rest and digest activities. Sympathetic fibers, on the other hand, come from the thoracolumbar spinal segments and engage the body for fight-or-flight responses.
When it comes to interoceptive pathways, things are a bit different. These sensory fibers are not motor; they carry information back to the brain. Although not fully understood, visceral sensory fibers travel along similar pathways as motor fibers but in the opposite direction, sending information from the organs to the brain. This is how we get sensations like butterflies in the stomach or the urge to eat or drink.
We also have clinical evidence supporting interoception, such as referred pain. A person having a heart attack might feel pain in their shoulder, not in their chest, because interoceptive fibers do not map precisely to specific brain regions. Their signals are more diffuse. This phenomenon supports the idea that our internal sensory experience is complex, sometimes misleading, yet real.
All of this background in sensory systems connects to the concept of neuroception. Neuroception is not easily categorized as purely sensory or purely motor, because the autonomic nervous system is inherently motor in its primary function, while interoception is sensory. Nevertheless, through neuroception, our bodies respond to cues of safety or danger without conscious thought.
What I appreciate most about Deb Dana’s interpretation of neuroception is the idea that we assess safety by knowing what is happening inside our bodies (interoception), outside our bodies (exteroception), and between ourselves and others (social connection).
We monitor our internal cues through visceral sensations. This is rooted in neuroscience, as visceral sensory fibers provide this information. We monitor the external environment through touch, vision, and other senses. Again, we have strong evidence for this, especially when working with children with sensory processing disorders who may be hyper-responsive or under-responsive to sensory stimuli. And finally, we experience the "between" through the social nervous system—through mirror neurons and other systems that light up when we interact with others, as we now see through advanced imaging techniques.
These relational experiences are very real. They help us sense safety or threat on a biological level. A simple glance between a child and caregiver, or even the tensions that can arise in adult relationships, like the political disagreements I sometimes experience with my husband, are lived experiences that involve the nervous system at a deep level.
Safety is truly an embodied experience. We have the neuroanatomy to show this, which validates why these concepts matter. With that, I will turn it over to Maude, who I know will continue weaving together these ideas beautifully.
The Polyvagal Theory and Sensory Modulation
Maude: I hope to do you justice, DeLara. This is a vital place to pause and sit with what has been shared at many levels. I view PVT as a conceptual framework. The more I study the nervous system, the more I realize there are areas where the setup of the ventral and dorsal vagal systems may not match perfectly with what Porges proposed.
When I look at the body, I see it as an integrated unit, operating together. Porges and his colleagues could describe my breathing system above my diaphragm—my lungs and heart—as ventral vagal. Still, I also know from a broader biological perspective that breathing can activate sympathetic arousal, decrease parasympathetic inhibition, or modulate both depending on the context. Similarly, the organs below the diaphragm, such as the gut, kidneys, and bladder, must maintain a delicate homeostasis balance for the body to function well. The goal is always balance, always homeostasis.
That’s the framework I want you to keep in mind as we shift toward thinking about modulation. Lara has already laid the groundwork for this beautifully. As we explore modulation, I encourage you to reflect on what you already know about it. What anchors you when you think about modulation? Of course, we want to ground it in neurobiology—understanding the subdivisions of the peripheral nervous system and the role of the autonomic nervous system in responding to the world around us.
Our bodies constantly evaluate external information through touch, vision, and other senses and process it internally. In a beautiful webinar I listened to, Ruth Lanius spoke about the periaqueductal gray area of the brainstem as a place where external and internal information meet. It is located close to the vagus nerve and plays a vital role in the embodied sense of self.
When we think about early development and the baby's nervous system right after birth, we see that arousal levels are shaped by rhythm and regulation, by the mother's voice, body movements, and touch. Rhythm and regulation prime the interoceptive system at the beginning of life, making it available for ongoing development.
This is how I want you to think as well. Whether you are considering PVT or modulation, it comes down to our sense of availability and response to being present in the moment. It is an embodied experience, a state where the entire system is geared to respond to what is happening in the environment. It is the ability to say, "Here I am," and in that acknowledgment, affirm, "therefore I exist." This presence is an emotional self-identity and a physical and neurobiological identity.
This becomes the first connection point between PVT and modulation. Both concepts speak about the same body. While PVT uses the metaphor of the ladder, which we don't necessarily see represented the same way in modulation theory, there is a shared foundation where they overlap—inside the workings of the vagus nerve.
Both frameworks emphasize receptivity to the environment and adaptability, which foster the flexibility needed to respond to whatever the environment brings to our system. This flexibility is essential for maintaining a healthy, balanced nervous system, and a resilient sense of self.
Jane Ayres
Jean Ayres talks about the sensory modulation system as part of the central nervous system, specifically in how it regulates the activity of the central nervous system. For those of you who have training in sensory integration, you are familiar with the concepts of modulation and discrimination. Discrimination is how we grade movement, determine how hard or softly to push, how much force to use—all the fine-tuning that develops over time through early sensory experiences.
However, if the modulation system, particularly the autonomic aspect, is not supporting the foundational ability to process and manage those pathways of discrimination, it disrupts the entire system. Even though modulation and discrimination are separate systems, they are very closely related and co-regulate in essential ways.
Jean Ayres used an excellent analogy to describe modulation. She likened it to the old-fashioned radios where you had to turn the dial to find the station manually. You would hear crackling and hissing as you moved through static until finally landing on a clear signal. Modulation keeps us in that stage where we initially hear the crackling and the fragmentation, but if modulation works well, we eventually find the clear channel. Without proper modulation, the message remains distorted and fragmented, preventing it from reaching the prefrontal cortex in a way that allows for adaptive, organized action.
This image captures how critical modulation is—not just in sensory processing but also in setting the stage for higher-order thinking and adaptive behavior.
Sensory Modulation and Emotional Regulation
We can't talk about sensory modulation without also talking about emotional regulation. I love learning PVT and seeing how it frames the nervous system as a social engagement system. It makes complete sense because modulation is deeply connected to emotional regulation, and emotional regulation is, in turn, connected to modulation. You cannot be socially effective if you are not regulated sensorily and emotionally.
They may have different triggers. I might become dysregulated if someone close to me hurts me emotionally, or I might become dysregulated because I am tactilely defensive. Dysregulation may look the same on the surface but can stem from very different origins. Our experiences, starting from in utero all the way through life, are primarily encoded in the brain through sensory information and emotional associations. Emotional and sensory experiences walk together.
This is why, when we see children with modulation challenges, we often hear them labeled as "having behaviors." I’m not entirely sure how I feel about that term. After all, we all behave—behavior manifests our internal processing. Saying someone "has behaviors" without context doesn’t mean anything. If you say I have an adaptive response to a sensory or emotional trigger that manifests as an outward behavior, that makes sense. However, labeling behavior without understanding it does a disservice to what is happening internally.
Think about the brain like a computer. You input the data first, gather the sensory and emotional information, then organize it, making sense of what fits together and what does not. Only after that processing happens can you "print out" a behavior. The behavior you see is the direct outcome of what data was gathered and how well it was organized. There are no hidden messages; the behavior reflects what the system has been able to process and how it has adapted.
Understanding this is critical when discussing how modulation and emotional regulation connect. Trauma can drive people into deeper states of shutdown or hyperarousal. We have a different "flavor" or response pattern to overwhelming stress or input. The ability to regulate—or the lack of it—has everything to do with how the autonomic nervous system supports us through our environment's sensory and emotional demands.
We know that self-regulation does not develop fully until much later in life. Research shows that true self-regulation, a part of executive functioning, typically becomes fully available between 24 and 28, depending on which study you read. Early in life, children depend on co-regulation. Whether through sensory experiences, motor activities, or emotional support, we provide co-regulation to help children organize their internal worlds. That’s very similar to what PVT highlights: supporting the nervous system through social engagement to promote regulation.
I also want to address an old analogy that is often used but needs some updating. Many people describe the sympathetic nervous system as the "gas pedal" and the parasympathetic as the "brake." That analogy is too simplistic. In light of PVT, it is more accurate to think of sympathetic arousal as what happens when you press down on the gas pedal—you increase speed, and if you don't modulate it, you will eventually crash. The parasympathetic nervous system, particularly the ventral vagal system, acts more like lifting your foot off the gas to bring the intensity down. It isn't about slamming on the brakes; it’s about inhibiting excessive arousal and returning to a balanced, flexible state. The brake analogy more closely fits the dorsal vagal shutdown—when the system is overwhelmed, and you come to a complete stop.
This distinction is important because it shapes how we view stress and the body's response to it. Cortical arousal, which is necessary for coping with challenges, depends on sympathetic activation. We need some sympathetic arousal to function through stressful periods—it helps mobilize muscle strength and mental focus. The key is maintaining usability and functionality, and then having the ability to return to rest afterward.
When sensory experiences are overwhelming—when the environment is too bright, too noisy, too chaotic—the system becomes flooded. Our survival instincts kick in, prompting fight, flight, freeze, or fawn responses. This is true for everyone. If a bomb went off near us right now, our nervous systems would mobilize immediately to survive. That instinct is not pathological; it’s built into us.
However, the way individuals respond to sensory information varies. One person might become highly vigilant and impulsive, feeling the urgent need to act. Another person might take a more thoughtful, measured approach. When a child’s response does not seem coherent with the situation, we often label it as maladaptive. But from the child’s point of view, their response is entirely adaptive to the sensory information they are receiving.
We must remember that what looks like impulsivity or aggression to us may, in fact, be a child's attempt to survive overwhelming sensory and emotional input. Our job is to understand the child’s sensory experience and how it impacts their motor planning, emotional responses, and overall regulation. By doing so, we can move away from judgment and toward a deeper, more compassionate understanding of the internal processes driving the behaviors we see.
Sensory Defensiveness
When we talk about sensory defensiveness, which everyone working in pediatrics today encounters, whether it’s tactile defensiveness, auditory defensiveness, or another form, I am hoping you could expand your view and think of it as sensory-emotional defensiveness. Especially in the trauma world, but even outside of trauma, the sensory systems themselves can become the source of the trauma experience. When sensory systems are overwhelmed, they simultaneously trigger emotional adaptive responses. Likewise, when a child is emotionally triggered, it often simultaneously triggers a sensory adaptive response of defensiveness.
If you approach every child’s defensiveness similarly, you’ll quickly notice differences in response. Some children might respond well to a deep pressure therapy protocol, finding regulation through tactile input. Others may not respond at all to that intervention. Some children might react beautifully to sound therapy as a regulatory method, while others find it ineffective. That’s because there is a two-pronged mechanism at play: one rooted in the sensory system, and one rooted in the emotional system.
The limbic system’s association with the reticular activating system, critical for maintaining the balance between sympathetic and parasympathetic arousal, plays a central role here. These systems are deeply interconnected, meaning sensory input and emotional processing are never truly separate.
Because of this integration, the therapeutic relationship between the client and you becomes paramount to decreasing defensiveness. The connection, the co-regulation, and the trust that you build become just as important—if not more important—than the sensory protocols themselves. Through relationships, we help modulate not only the sensory systems but also the emotional responses tied to them.
Gravitational Insecurity
Gravitational insecurity is a modulation issue in which the vestibular system, particularly the utricle and saccule, does not accurately process movement and position, leading to a deep, reflexive fear of movement. It creates a sensory-driven fear response, not a cognitive one, causing even slight shifts in position to feel unsafe. Figure 2 shows an anatomical image of the internal ear.
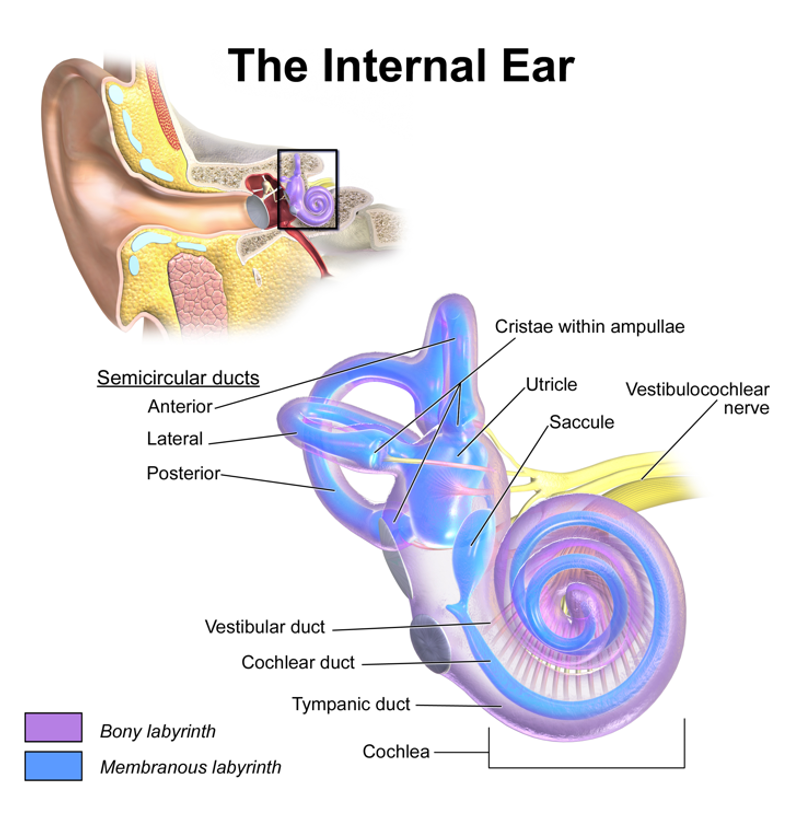
Figure 2. The internal ear anatomy (Click here to enlarge the image.)
Especially with gravitational insecurity, tipping your head back or lifting your feet off the ground can trigger a fear response entirely out of proportion to any real danger present.
When we think about trauma survivors and the PVT framework, we often talk about danger and threat. It’s important to remember that risk or threat is not always visible to the outside observer. It is something deeply experienced within the system itself. The body creates an adaptive response to that internal sense of threat.
When the sensory system sends inappropriate messages about where the body is in relation to gravity or movement through space, it undermines the feeling of being grounded. Over time, this can affect self-identity development and diminish one’s internal awareness of the body in the safest, most secure way possible.
Aversive Responses to Movement
Another related condition that can look very similar to gravitational insecurity is what the literature refers to as aversive to movement. This one has more to do with dysfunction in the semicircular canals, which detect rotational movement. Although the underlying systems differ, the outward presentation can look almost the same, with very high insecurity about how grounded and stable the body feels in a given moment.
Under-responsiveness to Sensation
The fourth category we can discuss is under-responsiveness to sensation, which can correlate more closely with a dorsal vagal experience. In this state, sensations are not noticed in a typical way; there is more of a sense of numbness, a flat affect, where the child may appear disconnected from the sensory input around them. Sensations occur, but the response is delayed or blunted, sometimes leading to a complete shutdown.
It's important to remember that it’s difficult to talk about any system as being purely under-responsive or over-responsive. Most often, we can say that an individual leans toward being more responsive in one specific system, but not necessarily in all. Different sensory systems within the person can have different profiles—one system may be highly over-responsive while another is under-responsive. A mixture of sympathetic and parasympathetic influences runs through every system.
We shouldn't think of it as either-or. We are looking for flexibility: the ability to move between heightened and dampened responsiveness depending on what the situation calls for. That brings us back to the idea of the ladder system from PVT—not as a rigid hierarchy, but as a model of fluid, adaptive movement between states.
In one of her webinars, Janina Fisher said something that resonated with me: We have incredibly smart systems. I had always known that, having worked with nervous systems my whole career, but how she phrased it hit me differently. It made me realize that behavior, even when it appears maladaptive to us, is never truly maladaptive for the child. The child uses whatever available resources to create an adaptive response to their experience.
If they are being bombarded with sensory input, flooded emotionally, or numbed by overwhelming conditions, their adaptive response will match that experience. Our role, then, is to change the experiences we provide. We must understand how to grade sensory and emotional experiences in a way that helps the child shift their adaptive responses over time, moving toward greater flexibility and regulation.
Arousal
When we talk about arousal, that’s what we’re referring to. Arousal means how wakeful and alert I am—whether I am aroused enough to be present and engaged, as I speak today. There’s a certain amount of sympathetic arousal within me right now because I want to make sure I stay on top of my game and give you the experience and information you came here for.
At the same time that I maintain this sympathetic arousal to stay engaged, I’m also regulating myself. I temper my voice, slow down my speech, and pace myself in a way I hope you can follow and enjoy. This is where my parasympathetic system steps in, helping me to down-regulate the sympathetic activation, maintaining a balanced arousal level that keeps me available and present.
I’m also maintaining an awareness of my environment—where I am sitting, how far I am from the monitor, and making sure my voice projects clearly over the microphone. I am staying aware of my physical positioning and surroundings, just as much as I’m aware of the content I want to share and how I want to share it. All of this—the sensory feedback from my body, the awareness of my environment, and the knowledge I draw—comes together to form my adaptive response to you. It is activated by both my sensory experiences and my cortical processing, weaving together to create the experience of being fully present and connected.
Stress and Modulation
When we experience stress, it immediately impacts modulation, or what we often call the "gas and brake" system. If I am stressed, my system tends to stay in a state of hyperarousal.
An axis in the body governs this response—the HPA axis, involving the hypothalamus, pituitary gland, and adrenal glands, which releases cortisol in response to stress. So if I start thinking, "Oh my goodness, I’m not going to get through these PowerPoints today, I’m not going to cover all the information," my stress response may kick in, and I may begin to move into overarousal. As that happens, you might even notice my whole demeanor changing.
At that moment, I have to ask myself, how will I pace myself through this? Pacing is an executive functioning skill born from the foundation of sensory regulation. However, when stress takes over, it can override my executive skills. Even though I want to stay calm and regulated with you, if the pressure builds up and I won’t finish in time, that stress may overtake my calm state. It can lead me to skip over points I wanted to make or forget to mention something important.
Stress dampens the executive pathways in the brain, feeding into the body’s sympathetic arousal system. My body responds urgently to the notion that time is running out. This is part of an active monitoring system that works moment by moment, constantly comparing and adjusting based on internal and external cues.
Even as I speak to you, I draw on my past experiences. I remember presenting this PowerPoint before—though we tweaked it a bit for you today—and I recall what I needed to say and what received good feedback. I am using that memory in the present moment, weaving it into my delivery. This ability to pull from the past while staying present is part of our working memory capacity, and it remains available to us as long as we maintain good homeostasis within our nervous system.
Anxiety System
My anxiety system is not simply an over-arousing system. It also has the critical role of triggering the vagus nerve to step in and perform its parasympathetic job of inhibition. Suppose I have a healthy balance between my sympathetic arousal and parasympathetic inhibition when I feel anxious. In that case, my system should automatically call on the parasympathetic side, saying, "Hey, time for you to do your job. Step in here, calm me down, so I can move through this moment."
This process happens subconsciously, without conscious control. The ability to use my cortex to think critically—asking myself whether the input I’m receiving matches my expectations—depends heavily on this balance. If the sensory or emotional input I’m getting doesn't align with what I expect, and if there’s a mismatch, the behavioral inhibition system can be activated. That mismatch can draw me down into a shutdown response, or it can push me into escalating arousal, where I want to quit, to escape the situation altogether.
The fundamental goal of modulation is tempering these responses, keeping things steady, keeping the system moving forward at an even pace, like driving a car steadily at 60 miles per hour. We have cruise control today, but it only works well on an open road, not in the middle of traffic. In real life, we must keep making tiny, constant adjustments to stay on course.
This is precisely what Porges describes when discussing the social engagement system. It’s the continuous assessment happening inside: Do I engage or not? Do I feel safe enough to connect, or do I feel threatened? This internal negotiation always shapes whether we reach out to others or pull away to protect ourselves.
Impact on Praxis and Executive Functioning
Of course, all of this impacts praxis, and it also impacts executive functioning. Praxis is not something we are born with. For those of you who have training in sensory integration, you know that praxis refers to the brain’s ability to tell the body how to move. It is essentially an adaptive response based on the integration of sensory input and cortical planning. At birth, we don’t have praxis. We must first work through our primitive reflexes, integrate them into more mature movement patterns, and build a foundation of postural control.
We enter a critical constructive period around 18 months to two and a half years. Through play and exploration, we develop praxis—the ability to plan, sequence, and execute movements. This period is crucial. If good praxis abilities do not develop, it can create a deep sense of immobilization, physically and emotionally. Without strong praxis, children may feel like they cannot participate in the same way as their peers. They may struggle with sequencing, timing, and rhythm, operating on a different track from others around them.
It can be extremely disconcerting when a child is cognitively aware enough to notice this mismatch but doesn't understand why it’s happening. It feels like fighting a battle you cannot see or name. Praxis difficulties can lead to executive functioning challenges later on, but they can also impact a child's sense of autonomy, hope, and social connection. The child may wonder, "Should I keep trying to engage, or should I just withdraw and stay shy?"
We must focus on what the body needs when considering these challenges. If a child struggles with processing external information—especially when the sensory environment is overwhelming, like in a busy classroom—then the negotiation happening in areas like the periaqueductal gray becomes compromised. The child isn’t just trying to focus on the lesson; they are also fighting to stay grounded in their own body, battling the external chaos. It’s no wonder that sometimes we see children smiling or appearing calm on the outside, even though internally, they are waging a silent war.
This is also where the interoceptive system becomes vital. When children are in a state of high sympathetic arousal, the interoceptive system often gets suppressed. As a result, we may see patterns like increased bedwetting beyond the typical developmental window, picky eating to exert external control over internal chaos, wet accidents at school, or avoiding the bathroom altogether until they get home. These autonomic functions—things most of us take for granted—become severely impacted when the homeostasis between sympathetic arousal and parasympathetic inhibition is disrupted.
When children feel out of sync with their interoceptive selves—their internal sense of their bodily state—they often gravitate toward activities that require limited body involvement. They may prefer video games, screen time, and computer activities where the mind is engaged, but the body is inactive.
Observing the activities children seek out or avoid can provide a great deal of valuable information. Their preferences can give us important clues about how well their sensory, motor, and emotional systems work together or where they struggle.
Attachment and Sensory Modulation
When you turn to the world of attachment, you realize how deeply intertwined it is with modulation. We don’t have enough time today to discuss all of this. Still, it’s essential to acknowledge that when relationships early in life feel unsafe, even without any judgment toward anyone involved, it leaves a lasting impact. Life happens: postpartum depression, parents struggling with their health or circumstances, adoption, foster care. These experiences intersect heavily with modulation, and we must recognize that overlap.
When a baby doesn’t consistently feel safe in those early months of life and receives an ambivalent response—sometimes the caregiver is there, sometimes not—the baby may develop an ambivalent attachment. This isn't because the caregiver is bad; it’s often simply because of circumstances. However, that ambivalent attachment can prime the nervous system more toward survival responses rather than allowing the baby to settle into homeostasis. As a result, we may later see difficulties with sleeping, eating, and other activities of daily living. There can even be a resistance to autonomy—an internal sense that growing up might lead to losing that caregiver's attention or support.
Think, too, about the avoidant attachment profile. A child with this pattern often says, “I’ll do it myself.” They may push away help, saying, “Thank you, Mommy, I do it.” But at three or four years old, they often lack the developmental skills to do everything independently. That gap between the desire for independence and the lack of ability can quickly lead to frustration. If that frustration builds without adequate support, it can tip into a disorganized attachment pattern, where the child struggles to trust others while struggling with their limitations. Mary Main later added this disorganized attachment profile to the original work of Ainsworth and Bowlby.
When looking at modulation and considering the balance, or homeostasis, we aim for in the PVT model, it’s critical also to consider the attachment relationship between the child and their caregivers. If the way you are co-regulating with a child during therapy is supportive, but at home, the child is being met with a different style of interaction, there can be a deep disconnect. It doesn’t necessarily mean there is an attachment disorder—it may simply mean there are attachment dynamics that need attention to support co-regulation more consistently across settings.
This is true for both modulation therapy and for polyvagal-informed work. We must consider the connection patterns in the child's life because even with all the beautiful work you do in your sessions, an underlying attachment anxiety can be triggered and interfere with the child’s ability to integrate new regulation experiences. Awareness of this larger context helps us better support the child's growth toward true, sustainable regulation and connection.
Polyvagal Theory – Steven Porges
When we think about polyvagal theory, especially because so much of PVT is applied in trauma-related circumstances, we have to understand that the concept of safety is central. In trauma, safety is violated. It is not available inside the system, regardless of whether the external environment is safe. The violation of safety is a triggered response inside the body.
You know this feeling. When you walk into a party for the first time, it's a new environment. Maybe you meet someone, and after a few seconds, you can feel whether it’s okay to stay and engage with them or whether you need to distance yourself. Some people you feel drawn toward; others you instinctively want to move away from. Why? Because you are interoceptively picking up on cues of safety. We all have this internal barometer, but the way each of us handles safety varies, and our adaptive response to that sense of safety or threat is what matters most.
This is why it’s important to consider modulation in trauma circumstances—to create a better embodied response to the environment in any given moment. When the experience of safety has been violated, it creates distance in future relationships. It affects how much physical contact feels acceptable, how much we can ask for nurturing, and how much we are willing or able to offer nurturing to others. It impacts how safe we feel with other people.
For some, the violation of safety leads to panic and extreme hyperarousal, completely immobilizing the system. Others might appear completely numb, and it could be easy to misinterpret them as being under-aroused. But often, that numbness is actually a shutdown response triggered by overwhelming overarousal.
In modulation work, we don’t think about this experience strictly regarding a ladder. Instead, we see the whole body as constantly interrelating—ventral and dorsal vagal influences working together, not as isolated pieces. The goal remains the same: finding and supporting homeostasis. The regulation of sensory and emotional experiences is deeply tied to feeling safe. It’s not about “bad” behavior; it’s a protective mechanism.
To address a behavior, you must first address why the child or client needs to protect themselves. Deal with the trigger before you deal with the behavior. That understanding is key.
When you look at the levels of organization that PVT describes, you see it reflected in primitive immobilization—complete shutdown, disengagement, and survival responses like fight, flight, freeze, or fawn. Whether from the PVT lens or sensory modulation theory, these are all adaptive responses to feeling threatened. Even when a child smiles at you, it doesn’t always mean they are truly connected or regulated. The smile can be a social mask—an attempt to please, to avoid conflict, or to survive the moment—while internally, they are disconnected from their interoceptive experience.
Often, children suppress their internal sensations to survive the demands placed on them. They may go through the motions, but are not truly present to learn or absorb information. This is not something they can consciously control. It is an automatic, deeply biological survival response. Understanding this is essential to supporting authentic healing and regulation.
Neuroception and Sensory Modulation
When looking at neuroception and sensory modulation, and considering how they map onto the polyvagal states, it becomes clear how interconnected these systems are. We seek sensory thresholds to achieve and maintain homeostasis in a ventral vagal state. There is an ability to regulate, to stay balanced and present, similar to what I described earlier about my own experience right now—being alert but regulated enough to connect, speak clearly, and stay engaged.
When the sympathetic nervous system becomes more dominant, we examine whether the sensory input triggers over- or under-responsiveness. Is the system receiving too much or too little input? Do I need to mobilize into a fight-or-flight response? That internal decision-making process begins to stir. Something is happening; the system senses it. How do we as therapists step into that space and provide co-regulation? How do we become a parasympathetic influence within the therapeutic alliance, offering our client a calming, anchoring presence?
When we enter dorsal vagal states, we start moving into shutdown, freeze, or fawn responses. As Lara said earlier, though, the dorsal vagal system is not inherently bad. Dorsal states can serve a positive, protective function.
Think about traveling. Suppose I leave the house early enough for my flight. In that case, I can stay primarily in ventral vagal—I feel calm, organized, and capable of navigating security, passport control, and boarding without stress. If I leave late and everything becomes rushed, my sympathetic system kicks in to help me mobilize and meet the deadlines, but the feeling of anxiety becomes very real and intense until I know whether or not I made it.
Now, think about those long international flights where you’ve traveled 14 hours, then 11 hours more, and now you're sitting in an airport waiting for your third connection. You find yourself just vegging out—you close your eyes at the gate, you’re not asleep, but you’re not fully alert. That’s a dorsal vagal state supporting you in that moment. You’re present enough to hear your boarding call, but you are conserving energy. That low-energy shutdown is adaptive, allowing your system to rest.
However, while dorsal vagal shutdown can serve a purpose, we cannot stay there if we need to learn, engage socially, or move through our daily lives. It's useful for moments of recovery, like allowing ourselves some "me time," letting that state wash over us so we can rebuild energy for the next period of sympathetic activation. But in contexts where active engagement is necessary, like a classroom or a social interaction, we need the flexibility to move back into ventral vagal states.
Understanding this dynamic—that dorsal, sympathetic, and ventral states all have important roles but require flexibility—is essential in guiding clients toward greater regulation, resilience, and participation.
Interoception
Interoception allows us to feel our internal embodiment truly. It is such a fascinating and essential system. Interoception will enable us to sense internal states like warmth, coldness, ticklishness, and other bodily sensations, but it also goes far deeper than that.
The sensory information from interoception is sent to the insula in the brain, often referred to as the "fifth lobe," tucked on both sides of the corpus callosum. The insula plays a critical role in processing and integrating these internal sensations. And just as a fun, nerdy fact, there’s even a specific part of the insula dedicated to the emotion of disgust, while the processing of other emotions tends to be a bit more blended across different regions.
Interoception is also profoundly connected to our sense of safety as infants. Some researchers suggest that disgust—or at least an awareness of discomfort and safety—is one of the earliest emotional responses a baby experiences. There’s a lot of discussion around the specifics, so I won’t dive too far down that rabbit hole here, but the main point remains: interoception is foundational to emotional experience.
The key emotional components that arise through interoception are intimately embedded within the vagus nerve itself, and this is precisely where polyvagal theory aligns so strongly. PVT emphasizes that our sense of emotional safety, regulation, and ability to engage socially are all directly tied to the state of our vagus nerve and our internal sensory experiences.
Requirements for an Embodied Self
Ruth Lanius, in her presentation on the periaqueductal gray, shared a powerful slide titled "Requirements for an Embodied Self." It posed a profound question: What does it truly mean to be a self? How are you "you," and how am I "me?" Her answer pointed to balance—a state of equilibrium within our system that allows us to remain in sync with both the world around us and our internal experience.
There is a synchronicity that gives us a felt sense of where our bodies are in space—even with our eyes closed, we know where we are in the room, the objects around us, and even the people nearby. At this moment, I am aware of where I am seated, how far I am from the screen, and how I am positioned at present. But I also hold a sense of continuity—an awareness of what I need to do tomorrow and what I’ve done today and in the past. This ability to track across time—to connect past, present, and future—is something that becomes especially difficult for trauma survivors.
There’s also the importance of the “I” perspective. Knowing that this is me—Maude—having a distinct sense of identity from a first-person point of view, and possessing the capacity to know how I feel, moment to moment. This is where things often unravel for children or clients with modulation difficulties.
For them, sensory input doesn’t always integrate smoothly and coherently. Instead, sensations run loosely, almost chaotically, across multiple sensory systems, leading to a feeling of fragmentation. These individuals may become reactive and reflexive in their responses, able to respond to what’s happening but without the prefrontal cortex's availability to pause, reflect, or gauge an appropriate response. The contemplative layer, which allows for thoughtful, regulated reaction, is often out of reach.
That loss of self-connection—the inability to name or even notice how they feel—is deeply tied to sensory modulation challenges and to the safety-threat evaluation system described in the PVT model. Without that foundation of felt safety, the sense of self—the embodied self—can remain elusive. In our work, restoring that balance is often the first step toward helping clients truly connect with themselves and with others.
Social Engagement and Modulation
When we talk about social engagement and modulation, you have to think about a number of different relay stations that need to come together.
- Cannot keep up with the pace of conversation
- Limited cognitive flexibility to go with the flow of change in group exchange
- Timing difficulties will impact the rhythm of conversation
- Difficulty understanding social nuances due to difficulty pairing gestural and verbal skills together
- Initiating and getting into the conversation difficult
- Diminished working memory can lead to impulsivity, hyperactivity, or withdrawal
- Finding common interests not always ideal
- Cannot use motor and verbal together at same time, impacting on many social games with rules
- Difficulty with “losing,” as winning would provide power, but losing reminds child of their “failure”
First, let’s discuss the conversational aspect. Kids—or adults—with modulation difficulties often struggle to keep pace with the rhythm of a typical conversation. There’s a breakdown in flexibility within the social engagement system, which makes back-and-forth exchanges harder to track and respond to in real time.
The natural rhythm of conversation is impacted by timing difficulties often linked to praxis. It’s not just about understanding the words—it’s also about synchronizing verbal and nonverbal communication. There may be trouble coordinating gestures, tone of voice, facial expressions, and spoken language to accurately interpret or convey the message in the moment. Initiating a conversation can also be difficult due to latency, or delayed processing, and joining an ongoing interaction may feel overwhelming or disorienting.
Working memory capacity also plays a significant role here, and that capacity is heavily reliant on embodied praxis—the physical and sensory experiences that help build internal organization. If a person struggles to stay grounded in their body, it becomes much harder to track the flow of conversation or hold onto details long enough to formulate a response.
Finding common interests isn’t always a solution, either. The way someone with modulation challenges experiences the world may be fundamentally different. What’s meaningful, engaging, or fun to them might not align with what others expect in social play or conversation.
There's also a common struggle with integrating motor and verbal systems. This can affect a wide range of social interactions, especially in structured games or group activities requiring physical and verbal participation.
And then there’s the emotional layer—when someone doesn’t feel in control of their system, they often experience a diminished sense of personal power. This can manifest in a strong need to win during games, not just for fun or competition, but because losing feels like a personal failure or a confirmation of inadequacy. It becomes an internal mantra: “If I don’t win, I’m a loser.” You and I know we can win or lose and still enjoy the experience, but for someone with modulation challenges, that kind of perspective isn’t easily accessible. The sense of safety and competence tied to regulation must come first before flexibility and joy in social play can take root.
Social Outcomes
Social outcomes will be different. and they look the same.
- No one will let me play.”
- “Why am I always the last to be picked?”
- Often become loners
- Victims of bullying
- Not invited to parties
- Rarely a “cool kid”
- Resistant to change
- Wanting to be the same – fighting the “unknown”
- Wearing clothes that fit in but may not suit the family lifestyle or culture.
- Children with high IQ can deliberately underperform to fit in, not wanting to be seen as “different.”
- More interested in video games than socialization
- Dependent on others to socialize
Whether you're viewing things through the lens of polyvagal theory or from the perspective of sensory modulation, the emotional and social consequences for children who struggle with regulation are often the same. You hear statements like, “No one will let me play,” or “Why am I always the last one picked?” These children often become loners, not by choice, but because their nervous systems—and resulting behaviors—set them apart in ways that peers may not understand.
Sadly, they are frequently victims of bullying. They’re not invited to birthday parties, they’re not seen as the “cool kid,” and often, they stand out for reasons beyond their control. Their resistance to change or preference for sameness isn’t just about stubbornness—it’s often a response to nervous system overload, where predictability provides a sense of safety. The unknown becomes a source of anxiety, and the familiar becomes a lifeline.
Adolescents, in particular, may try to fit in by mimicking peer norms—wearing certain clothes, for example—that may not align with family values or expectations. This can become a delicate and emotionally charged topic, especially when families navigate cultural or socioeconomic boundaries.
In working with teens, another subtle but essential challenge emerges. Children with high IQs may deliberately underperform in school just to avoid standing out. They don’t want to be labeled the “nerd” or singled out for being different, so they mask their abilities to blend in socially. It’s a form of self-protection, rooted not in academic difficulty, but in a desire for belonging.
For many, video games become a refuge. These environments are predictable, structured, and easier to manage than the unpredictability of face-to-face social interaction. Online or screen-based experiences may feel safer than real-life engagement, mainly when socializing depends heavily on others to initiate, organize, or maintain the interaction.
This highlights just how much nervous system regulation influences not only behavior but also identity, social access, and emotional well-being. Whether through PVT or modulation theory, we come to understand that behind many of these behaviors is a child—or an adult—trying to find safety, connection, and a sense of self in a world that often feels overwhelming.
Intervention
What do we do as we conclude this part of connectivity for you in the PVT and sensory modulation?
- Sleep Restoration
- Somatosensory complex
- Interoception
- Body Awareness
- Vibration
- Massage
- Weightbearing
- Postural Control
- Praxis
- Problem-solving
- Visual-Spatial
- Visualization
- Bilateral Integration
- Interhemispheric Organization
- Crossing midline from head to toe
Please, everyone, one of the very first entry points in your therapeutic process should be addressing sleep. If there is a sleep concern, deal with it first. It doesn’t matter whether your starting point is psychoeducation, establishing new routines, or facilitating medical referrals—this step is foundational. Look at everything from possible sleep apnea to reflux or silent reflux, which can surface only when a child is lying down but never fully reaches the esophagus. Evaluate underlying medical conditions, screen for possible allergies or breathing obstructions, and talk to families about their perceptions and practices around bedtime routines. This matters because quality sleep is critical for regulation and modulation. Everything else you’re working on will be harder to access without it.
Once sleep has been addressed, your next entry point is the somatosensory complex. This includes interoception and body awareness. And just as a little hint from my own practice, I use a lot of vibration. I love using full-body vibration plates. I place the child fully on the plate, allowing the vibration to stimulate the vagus nerve and deepen body awareness. It’s a powerful tool. In addition, Kelly Mahler’s curriculum is excellent for structured interoceptive and body awareness activities, and sensory integration (SI) work on its own is a beautiful way to enhance both body schema and postural control.
We also incorporate massage regularly—deep, slow, and relational massage. The specific type doesn’t matter as much as the quality of presence you bring. I use the MNRI tactile integration massage protocol quite a bit, but what’s most important is that you are present. You are not thinking about what you’re going to cook for dinner while touching someone else’s body. Your energy matters. We also do a great deal of weight-bearing, which is highly effective for somatosensory input and grounding. This naturally folds into developing postural control.
Once regulation and somatosensory grounding are in place, you can transition into praxis work—problem-solving, visual-spatial skills, visualization, and bilateral integration. From there, add sequencing and timing activities. Your final stage of integration involves crossing the midline from head to toe. That includes binocular fusion for the eyes, binaural listening for the ears, tongue lateralization for midline oral-motor coordination, upper body bilateral and cross-lateral integration, and the same for the lower body. All of these elements need to be synchronized, with proper sequencing and timing, to fully support functional integration.
But here's the caution I want to emphasize: don’t skip the first two steps. Many well-meaning practitioners leap into obstacle courses and praxis work because it feels productive and goal-driven. But if the body is not ready to receive and integrate the message, those activities will fall short. After everything we’ve discussed today, it’s clear—your client’s embodied self is the entry point. That embodied self is the source of felt safety, of being grounded enough to engage with the world and not feel threatened by incoming information.
You have to think through the lens of the child. A child with sensory challenges has a fragmented sense of self. They are doing the best they can with the resources they’ve been given. Until, of course, therapy steps in—and we help change the game.
Summary
Thanks for your attention today. We hope you learned something today.
Questions and Answers
Do you use cranial sacral therapy in your practice?
Lara: I don't, unfortunately.
Maude: I don't either.
Lara: I know people who do, and I've had several clients who have gone through cranial sacral therapy and liked it. So, we get good feedback from it, but I don't have personal experience with it. I'm sorry.
Do you have any favorite activities or practical application strategies for incorporating these ideas with parents and children in a treatment session?
Lara: Yes! I love what Maude mentioned about sleep and interoception. Interoceptive activities are key. For example, one of my students created a Velcro board with a body image and different interoceptive feelings like “a knot in my belly.” We might pair these with bodywork and help kids build language around what their bodies tell them.
I also talk about ventral anchors—things inside us, outside us, and between us that help us regulate. I ask students to name their anchors. For instance, right now I feel a threat from the NBCOT textbook I teach from, but I also have a ventral vagal anchor—my pickleball paddle—that helps me feel connected.
We even name our autonomic nervous systems with animals or colors to help give kids a language for their experience.
Maude: I use similar strategies. You can address this from both a top-down and bottom-up perspective. Lara said that top-down includes cognitive strategies like naming colors or identifying states. However, cognitive strategies only go so far without waking up the interoceptive system.
For bottom-up, I incorporate vibration and sound therapy. I’m a big proponent of music for regulation—it activates both brain hemispheres. While I won’t name a specific sound therapy here, Dr. Porges’ Safe and Sound Protocol is one example.
We also focus on body awareness—working on the floor, crawling, weight-bearing, and anti-gravity responses to engage the vestibular system. That foundational integration is vital.
How do you approach a treatment session with a child?
Maude: Awareness is half the battle. I never work with a child immediately. I let them settle into the space, observe what they touch and where they go, and I enter their world once they’re more settled.
I follow their lead—Legos or a platform swing—and tell them their ideas are good enough for me. Then we scaffold challenges gradually. It’s essential to enter a session with this lens of self-awareness and use of self, especially when dealing with systems sensitive to threat or danger.
Where can I get a vibration plate like the one you mentioned?
Maude: I usually get them from Amazon. One brand is LifePro or ProQuo. Look for one with adjustable speeds. They typically range from $259 to $325. I don’t have any stake in recommending them; I'm just sharing what’s commonly used.
At what point should an occupational therapist refer to a psychologist?
Laura: I’m not trained in trauma processing, so I typically collaborate with licensed mental health professionals—LPCs, LCSWs, MFTs—who handle that part while I focus on safety, stabilization, and resilience-building. That said, a child may still process trauma during OT sessions because we are in the experience with them.
Most of my clients are co-treated with a mental health professional, and we often refer caregivers as well. Co-regulation between parent and child is powerful when both have access to support.
Maude: The parenting and co-regulation piece is a whole topic itself. Every caring parent has anxiety about their child’s future, and we need to hold space for that. I often co-regulate parents during sessions—sometimes they join us on the floor, and other times, if they’re at their limit, I offer them a break in the waiting room.
When parents observe how we navigate frustration with their child in real time, they often have an “aha” moment: “That was so much easier than our usual power struggles!” Modeling is the best way to teach co-regulation—not just talking about it, but showing them.
References
See the additional handout.
Citation
Le Roux, M, & Taggart, L. (2025). Polyvagal theory utility in pediatric OT. OccupationalTherapy.com, Article 5797. Available at www.occupationaltherapy.com

