Introduction
Nicole: Thank you so much for taking the time to come today. We have a lot of information to go over. I am really excited to share this information with you. It is a way of reframing some of the things that we see out in the community and helping us be the liaison to help other professionals and families work with children who have a lot of difficult behaviors.
Why Do We Need To Address This As Pediatric OTs?
The big takeaway from this is that functional behavior plans do not work for the situation and that is the typical go-to within the school systems. This is what really led me to want to understand this better, and trying to affect some kind of change in the process. Many times the underlying problem is stress from the sensory environment. It disrupts participation in occupations, as well as performance. We see many kids avoiding participation in certain activities. It can create a significant amount of social and emotional distress for the child and for the family. Often there is shame involved, and shame is a very powerful emotion that can have significant consequences. If we can reduce the amount of shame involved, it can be a huge game-changer. If the child is not participating and receiving that learning experience, it can impede their development. We can affect significant change for these children.
Maslow's Hierarchy Of Needs
Figure 1 shows Maslow's Hierarchy of Needs.
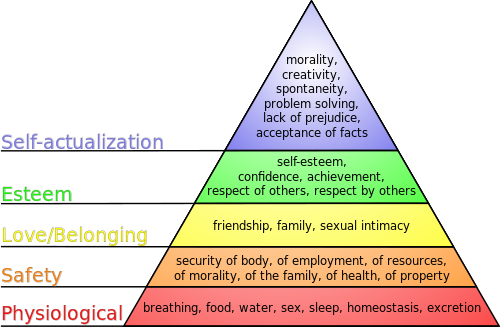
Figure 1. Maslow's Hierarchy of Needs. J. Finkelstein / CC BY-SA (http://creativecommons.org/licenses/by-sa/3.0/)
I use it as a framework when working with children and families. I use it for adults as well. The ultimate goal is self-actualization. It is a hierarchical process according to this model. Kids who have severe sensory processing oversensitivity are getting their physiological needs met, but when you look at the next level, they may not be getting their safety needs met. If the child is threatened by sensory input, which could be something as simple as the sound of the air conditioner, and their system cannot tolerate it, this becomes a safety need not being met. If you feel that people touching you is so noxious that you have this overwhelming response, then your safety needs are not being met. Often kids with these extreme sensory reactions get stuck in this safety mode. It is very hard to get them to a state of love and belonging. Often times these children do not understand what is going on, and they get a lot of mixed messages from those who work with them, including their parents, because it is hard to understand these behaviors. Again, there is a lot of shame involved. We want to work to get them out of this safety situation and then toward the love and belonging stage because there are some significant hurdles there as well. This is why I bring up Maslow's Hierarchy of Needs. The safety piece is really important with these kids, hence the reaction that you see in them.
Purposes Of Behavior
Behavior serves one purpose and that is to communicate. We tend to frame behavior in a very negative lens, but the behavior is very functional. The problem lies with the one who is receiving that behavior. Are they able to really decipher the language that is being conveyed and communicated? There are behaviors, especially in young children, that are wanting or needing something. For example, parents will say that their child is tired and that is why they are acting in a particular manner.
Some of the purposes of behavior are to:
- Seek (attention, food, tangible)
- Escape/Avoid (task, person, environment)
- Communicate Want/Need
- Sensory
One of the areas that is really important with younger children is communicating a want or a need. They also will escape or avoid a task, person, or an environment. This is where it gets a little confusing. Children with sensory issues often will throw a block because they do not want to play with the blocks. That is escaping or avoiding the task. Then there are the kids who seek attention, food, tangible items. A lot of kids go that extra mile to seek attention. They are not always doing a negative thing, but sometimes they can be quite disruptive. If the behaviors are seeking or communicating a want or a need, behavior modification, functional behavior analysis, and functional behavior plans work very well. The Premack Principle, or "first this then that", and other positive behavior supports work in these scenarios.
Negative supports do not work as well. Some kids need a positive-negative, but for the most part, they are very effective. I will never say that behavior modification is not necessary and it can be extremely successful. However, it needs to be a behavior. If it is done with sensory behaviors, it will not be effective because it is not a form of communication that has a specific trigger and does not have a specific consequence as the behavior does.
Sensory, Behavior, Or Both?
Let's compare the two.
- Sensory
- Occurs regardless of circumstances
- Happens for no reason-not predictable
- Positive behavior program does not change response
- The function is escape or avoidance
- Behavior
- Dependent on antecedents
- Predictable
- Responds to a positive behavior program
- The function is attention or communication, or avoid
(Kay & Quint, 2016)
When you look at the differences between the sensory and behavior, the behavior is very dependent upon whatever that antecedent trigger was before; it is very consistent. When the kid plays with the blocks, he takes the blocks and he throws them. It is the presentation of the blocks that is the antecedent. It is predictable, and the behavior will respond to a positive behavior program if you give the child choices. You can ask them if they want blocks or something else, give them a break card, or present a different strategy. Again, their function is very purposeful in terms of attention, communication, or avoidance. Avoidance can overlap into the sensory arena.
The difference with sensory is the behavior occurs regardless of the circumstances. It is not predictable and does not depend on those antecedents or triggers. Additionally, the timing is not always immediate. Children may have a meltdown from sensory overload because of something that happened earlier. As such, it looks very unpredictable and regardless of the circumstances. For example, you may have heard before, "I do not know what happened. He was fine and then he was not fine."
The other piece of the puzzle is that the behavior program is not working. This is another red flag that perhaps the analysis was not correct. If you couple that with some of that subjective feedback of there seems to be no antecedent and it is unpredictable, most likely it is sensory.
Typically, the function of sensory behaviors is to escape or to avoid when it is a severe behavior. There are other seeking behaviors, kids who like to chew on certain things, touch certain things, or squeeze things, but that is not what I am focusing on. Instead, I am talking about sensory function related to escape or avoidance, because these are the ones that are going to lead to the severe behaviors that are of the meltdown variety.
Sensory Processing
It is important to get the language consistent. When we talk about the idea of sensory processing, some of us may have learned it as sensory integration.
Sensory processing is the ability to register and modulate sensory information and to organize this sensory input to respond to situational demands.
Adaptive responses occur when someone taking in the information and responding to it in a way that is meaningful. This is something that can be very challenging for some of our kids. Modulation is the basic level.
Modulation is the ability to notice and regulate stimuli and respond in an appropriate manner.
If they cannot respond in an appropriate manner, we typically say there is a modulation dysfunction. Depending upon what model you use, it may be framed differently. In Lucy Jane Miller's model for sensory processing disorder, she would call these the sensory over-responsive and sensory under-responsive children or adults. If you look at Winnie Dunn's model, you would say that they are individuals that have a low neurological threshold, so these would be the sensory avoiders and the sensory sensitive children or adults.
The final things to think about are the concepts of habituation and sensitization.
Neurophysiological processes related to modulation of input are habituation and sensitization.
Habituation happens over time. "I have become habituated to the stimuli." For example, you put something on like a band-aid, and after a while, you do not notice it anymore because you have become habituated to it. I live in Florida and we have a wonderful older community down here. Many people become very habituated to the amount of perfume or cologne that they wear. It is just like any kind of odor that you come in contact with, over time you become habituated to it. If you have difficulty with modulation, however, you might not effectively habituate to it. You might also have this sensitization process, where instead of habituating and having the sensory input become less noticeable, you actually become more aware of it. It becomes more noxious, and it is something that eventually you might not tolerate. That is really the process that we are talking about with these kids.
Sensory Processing: Sensory Inputs
There are different sensory modality inputs.
- The brain processes multiple sensory modality inputs.
- Proprioception
- Vision
- Auditory system
- Tactile
- Olfactory
- Vestibular system
- Interoception
- Taste
- Activity level*
(Kay & Quint, 2016; Mangeot, 2001)
We should all be very familiar with the terms: proprioception, vision, auditory, tactile, olfactory, vestibular movement system, and taste. Also, it is important to know that interoception is your internal bodily function awareness. This is when you feel hungry, feel full, or know when you have to go to the bathroom. A lot of kids struggle with this. Interoception is also important because it is your emotional experience. There is a reason why we call being nervous as having "butterflies in the stomach". There is a sensation involved with it. We experience emotions as sensory input. Interoception is so important because these kids feel emotions rather intensely.
Within Winnie Dunn's tools, especially when you are talking about adolescents and adults using the Sensory Profile, it looks at the activity level. The activity level can be very overwhelming to children from a sensory standpoint. The intensity of the activity is also a threat to some of these children.
Sensory Dysregulation
Using Lucy Jane Miller's model, and a little bit of Jean Ayres' model, I wanted to go over some of the different categories for dysregulation and difficulty grading responses to stimuli.
- Over-Responsive
- Negative reactions to sensory stimuli
- Meltdowns, refusal to participate, aggressive behavior
- Under-Responsive
- Limited or decreased response to sensory stimuli
- Does not notice an injury, does not respond to name
- Sensory Seeker/Craving
- Increased need for sensory stimuli
- High energy level, put things in mouth, smells, touches others, poor safety
(Based on the work of Lucy Jane Miller's and A. Jean Ayers' models; Kay & Quint, 2016)
Sensory Over-Responsive
In this category, we are talking about children or adults who have negative reactions to sensory stimuli. This is the group that is going to have the meltdowns, refusal to participate, and unfortunately, aggressive behavior many times.
Sensory Under-Responsive
The under-responsive group is the kids or adults who have that decreased response to sensory stimuli. They tend not to notice when they are injured, they do not respond to their name, and they seem to have low energy
Sensory Seeking/Craving
Then, of course, we have a lot of kids who are sensory seeking. There are some extreme sensory cravers who need increased sensory stimuli and actively go about trying to obtain it. They tend to have high energy, poor safety awareness, touch others, smell things and can have a lot of social issues.
When we are thinking about under-responsive and sensory-seeking from the Winnie Dunn model, we are talking about the people that have a high neurological threshold and need to fill it. The under-responsive folks do not always fill their cup with their input and that is why they miss a lot of information, so we might call them low registration according to Winnie Dunn. Meanwhile, the seekers are the ones who actively try to get that input.
Motor Based Postural Disorders
As a quick reminder, we also have individuals with poor posture and dyspraxia.
- Postural
- Difficulty staying seated, maintaining postural control
- Hyperactive- never stops moving, uses momentum, attention difficulties, lays on desk, meltdowns, and frustration
- Dyspraxia
- Difficulty with ideation and sensory feedback to plan and execute movements
- Uncoordinated- avoid tasks, doesn't follow directions, meltdowns, and frustration
(Kay & Quint, 2016)
Postural
When you talk about postural issues from a sensory standpoint, these are kids who have a hard time staying seated and maintaining postural control. They can look hyperactive or display low energy. They use momentum for movement, have attentional difficulties, may lay on their desk to do their work, and can also have meltdowns and frustrations.
Dyspraxia
Kids with dyspraxia can also have meltdowns and frustration because they have difficulty with ideation and sensory feedback. They experience frustration with movement and following directions. I like to call it a betrayal of the body. When your body will not do what you want it to do, it feels like a betrayal. I see many kids with dyspraxia that have a higher risk for meltdowns even though they are not necessarily over-responsive to input.
Other Disorders With A High Comorbidity With SPD
Sensory processing disorders (SPD) have high comorbidity with other disorders.
- ADHD
- Up to 47% of students with ADHD meet criteria for one type of Sensory Disorder (SPD), up to 80% comorbidity
- Students with ADHD and SPD have a high risk for anxiety (Reynolds & Lane, 2009)
- Gifted
- Up to 35% of gifted students have SPD (Cronin, 2003; Jarrard, 2008)
- Asperger's/Autism
- 75% of individuals with ASD have SPD (Cheng et al., 2005; Miller, 2014)
- Developmental Disabilities (DD)
- 40-85% of children with DD have SPD (Miller, 2014)
- Anxiety
- Schizophrenia
- Bipolar Disorder
- Oppositional Defiant Disorder
- Tourette's
(Kay & Quint, 2016)
It is important to remember that there are a lot of kids out there who might not have a sensory diagnosis but have a disorder with a high comorbidity with SPD. If you look to the right in the box, there are a lot of high percentages there. The concomitant behavior of SPD with any of these is what I call white matter disorders.
Do not forget about the gifted kids. This is a little controversial, but some people consider gifted a learning disability because a lot of these kids do not really understand how they learn, it is just really easy for them. Often their frustration tolerance is low. They also have high comorbidity of anxiety, and it has been shown that they tend to have a pretty high amount of SPD as well. I am sure most of you are very familiar with the high levels of comorbidity with autism as well as ADHD. I think the number of 75% for autism is actually pretty low.
When you are going to use some of these strategies with these kids, I typically put my treatment diagnosis as non-specific anxiety as well. There is a reason why you are doing what you are doing with the meltdowns. It always gets covered by insurance.
I also wanted to give you some research information so that you can appreciate how prevalent this is with different diagnoses and why. If you are educating someone, then you have a resource.
Beyond the Numbers
- Visual sensory processing deficits exist in bipolar disorder (Yeap et al., 2009)
- Schizophrenia- Less gray matter (parietal lobe) which is base for sensory function, correlation with sensory processing deficits (Kreitschmann-Andermahr et al., 1999; Ahevinen et al., 2006)
- Bipolar has extremely high co-morbidity with ADHD (62-98%) (Youngstrom et al., 2010); inherent in bipolar to have sensory distortions and unstable sensory processing due to cortical thinning in parietal and occipital lobes (Lyoo et al., 2006)
- Both bipolar and schizophrenia have abnormal sensory gating, impaired sensory-motor systems (Thaker, 2008; Davies et al., 2009)
- Children with fetal alcohol spectrum disorders have problem behaviors related to sensory processing (Franklin et al., 2008); important to note that schizophrenia has possible etiology related to alcohol intake during pregnancy
(Kay & Quint, 2016)
Sensory Input Received
How does this work?
- Brainstem activated with norepinephrine (warning system for arousal)
- Arousal increases once amygdala (limbic system) activated
- Eventually, dopamine released
- Sensory input goes to the thalamus (1 of 2 places relayed)
- Cortex: perceive sensation, initiate movement
- Amygdala: for memory pertaining to arousal/attaching emotional meaning to a stimulus (can lead to fight or flight)
(Kay & Quint, 2016)
It is an interesting process. When we look at the brain depicted here, sensory processing is a very basic physiological response that we have to sensory input. It starts in the brainstem. We start to get sensory input, and your brain has to identify whether or not the sensory input is a problem or not. If there is an alerting sensory input, your arousal increases. That is how we use sensory input to affect arousal. If it goes into what we call the lizard brain or the amygdala, the limbic system is activated and dopamine is released. That sensory input relay then goes to the thalamus. There are a couple of places in the cortex that then receive it. The cortex says, "Oh, this is the sensation. I am going to initiate some kind of movement."
Threat Analysis
The amygdala attaches an emotional meaning to the stimulus.
- Amygdala to R hippocampus
- From hippocampus to R orbitofrontal cortex (OFC) for more information and memory activation
- Threat vs. excitement analyzed and survival behavior either increased or decreased
- Organizes motor defensive behavior and autonomic responses to "threat"
- OFC activates the hypothalamus, the brain center for autonomic function (Miller et al., 2007: Van Hulle et al., 2012)
(Kay & Quint, 2016)
For example, when we think about something that makes us happy, we tend to identify a sensation with it. "Oh, that smell reminds me of my grandparents' house." We have these emotional attachments to sensory stimuli. It is a really important part of the process because after it goes around to these different areas in the brain, it makes its way over to the hippocampus. The hippocampus derives meaning from this input. This happens very quickly. It has to decide whether it is a threat or excitement? When that happens, you have now imprinted on your brain whatever it decides. If it decides it is excitement, then you have a positive memory. If it is something that is identified as a threat, it is now been labeled in your brain as a threat, and you are going to kick in an autonomic reaction, which is fight or flight. Meltdowns are basically a fight or flight reaction.
I am providing the link to an individual's blog (eatingoffplastic.wordpress.com/2014/07/23/highly-sensitive-person-vs-sensory-processing-disorder/). She is an adult living with a sensory processing disorder. She has some interesting insight.
Children who have sensory over-responsiveness have an abnormal threat analysis. It is a survival mechanism. Every time they experience this sensory information, their body becomes much more efficient at identifying it as a threat and turning their autonomic system on to fight or flight it. As a result, their reactions get faster, more efficient, and more dramatic, unfortunately.
I have a couple of videos so that you can see what this looks like. The comment was, "Prior to the video, everything was fine. He was climbing on the equipment and smiling." Please note that neither video has sound so that you can concentrate on what you are seeing.
Video #1
In this video, you can probably appreciate that it was a very busy environment with lots of people. The music was pretty loud. You can also see that he is looking a little off. As mentioned above, right before this he was having fun. Here is another video.
Video #2

In this second video, he has moved to head butting. He is actually a fighter and not a flighter. Mom is basically the recipient of the fight. Even though she did not do anything to him, he is going to fight because he does not know what it is that he is fighting.
What Autonomic Systems Are Affected?
When we think about an autonomic experience, the sympathetic and parasympathetic nervous systems are activated.
- Parasympathetic Nervous System
- Homeostasis
- Enteric Nervous System
- Gastro system (not yet studied)
- Sympathetic Nervous System
- Fight or flight
(Kay & Quint, 2016)
Sympathetic is the fight or flight piece. We do not quite understand how the enteric nervous system gets involved, but it is your gastro system. We are learning more about it. Many kids have a lot of stomach issues. The young man in the video has significant gastro issues that require a special diet. He does not have autism, and he is gifted. He is very successful in school, but he has a lot of stomach issues. He has gas, bloating, constipation, and then sometimes diarrhea. It is a constant struggle for him. The parasympathetic system really tries to provide us with homeostasis. When that is knocked out, or activated in a way that it cannot do that, everything is thrown off. It is a pretty complicated process.
What Are The Signs?
- Red Ears
- Facial color change (pale, red)
- Muscle tone changes: decrease (noodle kid), increase (fisting, rigid/tense)
- Significant reduction in performance in a short amount of time
- Breathing changes (holding breath, heavy breathing, etc.)
(Kay & Quint, 2016)
The good thing is there are signs. When the kids start to get red ears, that means the limbic system has already been activated, and it is going into autonomic. You may also see their face change color, either paler or redder. Muscle tone may also change. You might see them turn into a "noodle kid". We may think that these kids just lay on the floor and play dead, but it is not that. They lose muscle tone temporarily. You can also have the flip side or increased muscle tone. They might start fisting, or go rigid or tense. You could see the boy in the video had increased tone. He had a fisted hand and was hitting mom with it. He was also head butting and had some extension activated there as well.
There is also a significant reduction in performance in a short amount of time. They go from perfectly fine to then falling right off the cliff. It almost looked like he was a little glassy-eyed, and he was not able to even communicate. You may see breathing changes; they may hold their breath, or have heavy breathing. You could not hear it with him because the music was so loud, but he actually had an increased breathing sound. He did not get the red ears or face, but he did get a little pale. His big things were the muscle tone change, the reduction in performance, and the breathing changes. Every kid is different, but all of them will have a significant reduction in performance.
You may see kids start to have to hold their heads up when they are working or hitting themselves on the head. They may also pound their fists on the table. These are good signs that something is going on. They may suddenly have to lay their head down because they cannot hold themselves up anymore. They might also say that they are shaking or have dry mouth. We know what it feels like to have our heart racing and they might feel that as well. This is something you can always ask them after the fact. You will not be able to tell unless you put your hand on their chest and they typically will not appreciate that during a meltdown, so I do not recommend it.
How Does This Affect Function?
How does this affect function?
- Acute arousal and defensive posture produce a consistent FREEZE
- Helpless to solve the problem--helplessness results
- Repeated FREEZING--passive immobility despite given new possibilities for escape
- Problem-solving and learning potential becomes negatively influenced
- FREEZING can then result from neutral stimuli
- Environmental input (initially benign) can then become traumatic stimuli
- AKA- "Deer in the headlights" or shutting down
(Kay & Quint, 2016)
When you have acute arousal and a defensive posture, it produces a consistent freezing situation. It is the outcome of an inability to solve a problem, so it is like learned helplessness. We call this repeated freezing passive immobility. These kids basically shut down. When you go into fight or flight, your autonomic system is activated and you have a reduced cognitive ability. Your cognition shuts down and problem-solving is not going to happen. When someone tries to give you solutions while you are in a meltdown, it only aggravates the system and makes it become a threat. You cannot work on a meltdown while they are in a meltdown. If we try to reason with them it is only going to make it worse. The limbic system is involved during a meltdown.
- Limbic Activation
- Not a tantrum
- Not behavioral communication
- Often sensory-related
- Fight or flight
- Confidence killers
- NEED SUPPORT not PUNISHMENT
(Kay & Quint, 2016)
Meltdowns are not a tantrum or a behavioral communication, they are fight or flight. They do not respond well to punishment or a functional behavior plan. It is also important to note there is shame tied to these meltdowns. These kids are not proud of their behavior, and it is highly embarrassing and shameful for them.
Intervention Approaches
This outlines specific approaches to intervene in a meltdown.
- Student-Centered Care
- Reframe the behavior, education, information, coaching
- Sensory strategies to maintain arousal level for learning
- Increase coping abilities
- Environmental adaptation
- Cognitive, behavioral, and social-emotional learning
(Kay & Quint, 2016; Warner et al., 2013)
Reframe the Behavior
It is very important to reframe the behavior. When we talk about how to intervene with these kids, we need to help people to look at it a little differently. We want them to know it is sensory-related, there is no trigger, no consequence, and it is not a form of communication. Most people have experienced this fight or flight sensation at some point in their life, and so they can understand it. Pointing out the physical signs is also very helpful.
Sensory Strategies
We can use sensory strategies to maintain their arousal level for learning. Proprioception is the magic bullet. If you can give proprioception to kids who tend to really ride high on these sensory responses, you can calm them down.
Coping Abilities
We also want to go in and increase coping abilities using these sensory strategies. Have them start to make decisions about what they need in a preventative sort of way, and also what they can use to calm down after they have had an episode.
Environmental Adaptation
We need to adapt to the environment. We need to understand that some environments are going to trigger this. The school environment is tough, and even more so in the cafeteria. How can we adapt things to make it less threatening to them. Do they need a little chill place in the classroom to go to? A lot of teachers are really starting to respond to this idea and are providing options.
Cognitive Behavioral and Social-Emotional Learning
Finally, cognitive-behavioral and social-emotional learning is helpful. I am not going into all that here, but it can be very helpful to the process.
I always say they have to take these entire five strategies to really make a difference.
Goals for Sensory Processing Intervention
What are the goals? You want to make it very apparent that sensory processing is going to be part of the response with their behavior, and that has to be communicated.
- Awareness of the role of sensory processing in student's behavioral responses
- Maintain a calm, alert state in the learning environment
- Increased active learning and task behavior
- Utilize sensory strategies to self-regulate attentional and emotional responses
- Prevention of episodes of challenging behavior
- Decreased episodes of challenging behavior
(Sonia Kay & Nicole Quint)
You want to really start to regulate when you are working with them and then regulate them as well. How can they maintain a calm alert state in their learning environment? We need to teach the adults who work with them to also do the same. We want to increase active learning and task behavior. We want to have them start to learn how to use their own sensory strategies to self-regulate their attention and their emotions. We need to prevent episodes of challenging behavior by using sensory strategies like proprioception, or perhaps vestibular. The usual offenders are auditory and tactile stimuli so these are the areas we need to address. We would measure true behaviors and say that we have seen them go down. We also want to see sensory behaviors decrease as well.
Intervention Process
The intervention process includes the following.
- Assessment
- Use of observation, questionnaires, and assessments to determine the student's sensory preferences and needs.
- Sensory Diet
- An individualized specific daily plan of sensory stimuli that assists that individual in staying alert, calm, and regulated. Sensory stimuli are applied in a proactive method to satisfy/meet the student's sensory needs and support their function in the educational environment.
- Sensory strategies
- Sensory tools that include input from most of the sensory systems that the student can access when needed to regulate their emotions and behavior.
(Sonia Kay & Nicole Quint)
There are a lot of ways to assess this whether it is through observation, questionnaires, etc. The same way that you do with your typical sensory assessment, but you want to be mindful of how extreme their over-responsiveness is, and their history of meltdowns. You want the family to videotape it for you so you can see it. I like to trigger it in the kids myself, but if that does not happen, I need a video to see. You also want to look for those five signs.
We can intervene with a sensory diet, or sensory buffet as I like to call it. We can really have it include those preventative pieces as well.
We can have specific sensory strategies that the child can access as needed to regulate their emotions and behavior. An example could be a safe place to go if they are feeling stressed. They need to learn to identify when their system is being overstressed. I think about this as a two-fold process.
1. Self Regulation
- CBT
- Calming strategies
- Social & Emotional Learning
- Zones of Regulation
- Alert Program
- Power! Batteries
2. Sensory
- Emotional supports
- Preparatory Input/Sensory Diet (Buffet)
- Access to a quiet area
(Sonia Kay & Nicole Quint)
Sensory is what we do in the environment to support them. What kind of sensory diet or environmental adaptation can we provide? In terms of self-regulation, which is beyond this, there are cognitive-behavioral strategies and social-emotional learning. These are things like the Zones of Regulation or the Alert program. I have created one that I call POWER! Batteries.
Sensory Regulation Techniques
How can I alert or calm a system with sensory strategies?
- The sensation from all systems can be modified to increase or decrease the orientation
- In general to ALERT a system:
- Input is unpredictable
- Input is unfamiliar
- Input will be varied and change
- In general to CALM a system:
- The input is predictable
- Input is familiar and expected
- Input will be sustained
(Sonia Kay & Nicole Quint)
Alerting
For alerting, the input is unpredictable, unfamiliar, and varied and changed. Be aware that if the environment is alerting the child might be more at risk for having a meltdown.
Calming
If we want to calm a system, we would make the input predictable, familiar and expected, and sustained. So really when you're trying to calm these kids down, that's what we're going to be looking at.
Here are some types of input in Figure 2.
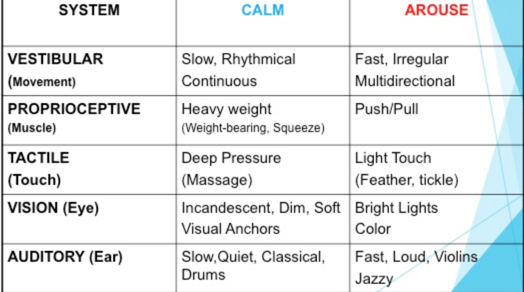
Figure 2. Types of calming and arousing input (Kay & Quint, 2016).
The chart lists intervention strategies, but these can be used for environmental adaptation as well. If one kid is stressed in an environment, other kids probably are as well. Classrooms are often loud with a lot of visual stimuli on the walls. It can be very overwhelming for kids and people do not even realize it. It is important not to forget about that piece of the puzzle.
Environment
There are environmental strategies as well.
- Classroom
- Structure-effect on sensory processing
- Visual schedule
- Movement breaks
- Set up of desks/types of chairs
- Sensory characteristics-effect on arousal
- Lighting
- Paint color
- Wall displays
- Noise level
- Structure-effect on sensory processing
- Sensory Strategies- can lead to self-regulation
- Sensory bins and kits
- Fidgets
- Cold water
(Kay & Quint, 2016)
Classroom
Within the classroom, we can promote structure with things like visual schedules, movement breaks, and alternative seating. Sometimes it is a simple thing like putting tennis balls on the chairs, to decrease that noise when they scoot in and out, that can make all the difference in the world. Teachers like it too. We all have sensory thresholds, and when you are in a noisy classroom all day, your system can use a break as well. If you are working with teachers or parents have them assess their sensory responses to the environment.
Some sensory characteristics can affect arousal. Lighting, paint color, wall displays, and noise levels are all important to consider.
Sensory Strategies
We need to have sensory strategies available to them. We need to teach them how to use sensory bins and kits. All kids can benefit from them as sensory processing is the basis for learning for everyone. For example, if I give a kid a ball to sit on, the teacher may say everyone is going to want a ball. That is typically the first time, but after that nobody really cares anymore.
Resources
I wanted to give you some resources.
- Fun and Function website has "build your own sensory break" form (https://funandfunction.com)
- POWER! Batteries and POWER! Battery Chart for monitoring
- Provided with additional resources for this course or the POW! Course
- Sensory stories
- Social stories
(Kay & Quint, 2016)
The Fun and Function website has a build your own sensory break form that I find super helpful. They have also a lot of equipment that you can order. There are many websites like this, but I really like this tracking form. Fun and Function is owned by an OT, so I think that is why it is such a great form. I have the POWER! Batteries and POWER! Battery Chart for monitoring in the handouts. There are also plenty of sensory stories out there. Here is a website that shows how to create a sensory story in seven steps. I like to make these with the child. This might also be good for a child with Oppositional Defiant Disorder (ODD) because then they have the buy-in. You know ODD is all about making them feel like they are in control. You can also look at this video (www.youtube.com/watch?v=R8c_Br8I_Tc) for social stories.
Conclusion
In conclusion, remember that all kids have sensory needs and challenges, but children with emotional challenges usually have more intense underlying sensory needs and difficulties. The sensory environment has positive calming effects when it is structured and predictable, and it can be alerting when it is unpredictable and unstructured. In some kids, especially those with a sensitive limbic system and neurological threshold, they will be at increased risk for abnormal threat analysis. Having sensory options can promote consistent, optimal environments that promote learning and decrease the chance of behaviors. If you are in a clinic environment or home health, you can create your own sensory options there as well. Finally, having all of these sensory options promotes learning for children and adults as well.
I do like to say thank you to my university as they allow me to do these courses. I also wanted to just give a huge shout out to Dr. Sonia Kay. We have a program that we created called It Just Makes Sense. We are really trying to promote using sensory strategies in the classrooms to promote learning and to prevent maladaptive behaviors. It is a lot of work because it is so hard to get into the school systems and affect change. One of the strategies that we use is to educate OTs, like in this format, so that everyone can be doing this is as well.
Questions and Answers
What do you do when a student will not participate in sensory strategies because of oppositional defiant behaviors?
First, we want to understand avoidance. Is it a behavioral avoidance or is it a sensory avoidance? Do they see sensory strategies as a threat? Or do they not want to take your advice on something? Typically, I use the manipulation method (sounds bad). However, I want them to think it is their own idea. Having them have as much choice in the process as possible is important. I might offer lots of different options. I might educate less and just have them think it is something cool in their interest area. For example, let's say we make a fidget. I might not tell them what it is and let them just think they are making a toy. Eventually, I would tell them how it could help. I have some kids who get very distressed by this because they know that you are giving them a solution to a problem and they cannot really admit to the problem. The problem is a threat. Thus, I really like to use more cognitive-behavioral with those kids coupled with sensory.
When you are dealing with someone who is having some issues, what are your top recommendations for teachers?
The big thing is getting them to reframe their perspective. Helping them to realize that it has something to do with the environment. I like to use a collaborative consultation model with teachers. I like to take the path of least resistance. I ask them if they prefer we gave them something for the child, or would they like to change something in their environment that works for everyone, including that child. Typically, they say they want something for the child, and then when they see that it works for the child, they then ask for something environmental. If the culprit is auditory then the use of headphones is very helpful. A quiet tent area is also very helpful. Resistive or proprioceptive activities throughout the day, coupled with movement breaks, are other great strategies. Will the teacher do some kind of movement breaks for everybody? Can they do something resistive with the kid like TheraBand on the chair? Could it be something heavy for the lap? Even chair push-ups are a great simple activity. I would like to emphasize the quiet safety area because I think it makes a huge difference for the kids to know they have a space to go to. I like to push that if I can if I feel that the teacher is open to it. Many of these teachers are really just beside themselves on what to do and they want help.
Is the It Just Makes Sense presentation available or will it be in the near future?
It is not, and this is the first one that I have done. I can definitely see that. It is a program that we are trying to put into the schools as a consultative model. We are always happy to educate everyone because we know that there is a big need out in the community for this.
I like your idea of having a program in place for all students, not just the one having sensory problems. Do teachers respond well to this idea?
I have a couple of teachers who really have taken literally the ball and run with it. For example, it might start with a therapy ball or something, some kind of adaptive seating situation, and once you get it in there, they usually then have the buy-in. If I can, I like to do presentations for the entire school, and that usually gets everyone more on board. I like to have the teachers do their own sensory checklist to see that they have some of the stuff too. I tell them that if they make some environmental changes, they are going to benefit from it. That usually helps them with wanting to make some changes in their classroom as well.
What recommendations do you have specifically for homework times when a kid is tired? Setting them up for failure but has to get work done.
If it is significant and I think it is beyond their capacity, I am going to try to get reduced homework as a temporary solution. Then I am going to have them do just a little bit. The environment is also very important. Do they need a little decompression prior? Do they need background noise? Sometimes we think that having a sterile, quiet area is ideal, but some of these kids need background noise. I need background noise. I cannot work without Spotify or Pandora because I am very distracted by noises in the halls, the air conditioner, the clock going, etc. I also want to give some kind of immediate reward for doing the activity, which has a lot of meaning. Over time, I am going to start making them have to work a little harder. But if it is a pretty significant situation, I am going to go the 504 route. Typically the schools are pretty good about that. Alternative seating can also make a huge difference. Let them pick what they want to sit on. Do they need a sensory reward after? Do they need proprioception? Again it is thinking about what do I need to calm and alert them? However, if they are seriously distressed by the homework and seeing it as a threat, I need to have them reframe the homework into something positive. I need to untrain or retraining the brain. The schools are starting to respect the sensory aspect now that the DSM has sensory for autism. I am noticing it is starting to trickle out and people are starting to notice that the functional behavior plans do not always work. They have to do something different.
References
Cheng, M., & Boggett-Carsjens, J. (2005). Consider sensory processing disorders in the explosive child: case report and review. The Canadian child and adolescent psychiatry review = La revue canadienne de psychiatrie de l'enfant et de l'adolescent, 14(2), 44–48.
Cronin, A. (2003). Asynchronous development and sensory integration intervention in the gifted and talented population. Retrieved from http://www.sengifted.org/ articles_social/Cronin_AsynchronousDevelopmentandSIIntervention.shtml
Davies P. L., Chang W. P., Gavin W. J. (2009). Maturation of sensory gating performance in children with and without sensory processing disorders. Int. J. Psychophysiol. 72, 187–19710.1016/j.ijpsycho.2008.12.007
Franklin, L., Deitz, J., Jirikowic, T., & Astley, S. (2008). Children with fetal alcohol spectrum disorders: Problem behaviors and sensory processing. American Journal of Occupational Therapy, 62, 265–273.
Jarrard, P. (2008). Sensory issues in gifted children: Synthesis of the literature. Retrieved from http://www.spdfoundation.net/pdf/SensoryissuesinGiftedChildren.pdf
Kay, & Quint. (2016). It just makes sense: Sensory solutions for the young child." Department of Occupational Therapy Faculty Proceedings, Presentations, Speeches and Lectures, 493.
https://nsuworks.nova.edu/hpd_ot_facpres/493
Kreitschmann-Andermahr I, Rosburg T, Demme U, Gaser E, Nowak H, Sauer H. (2001). Effect of ketamine on the neuromagnetic mismatch field in healthy humans. Brain Res Cogn Brain Res., 12, 109–116.
Lyoo, I. K., Sung, Y. H., Dager, S. R., Friedman, S. D., Lee, J.-Y., Kim, S. J., … Renshaw, P. F. (2006). Regional cerebral cortical thinning in bipolar disorder. Bipolar Disorders, 8(1), 65–74. doi: 10.1111/j.1399-5618.2006.00284.x
Mangeot, S. D., et al. (2001). Sensory modulation dysfunction in children with attention-deficit-hyperactivity disorder. Developmental Medicine & Child Neurology, 43, 399-406.
Miller, L. J., Fuller, D. A., & Roetenberg, J. (2014). Sensational kids: hope and help for children with sensory processing disorder (SPD). NY, NY: A Perigree Book.
Miller, L. J., et al. (2007). Concept evolution in sensory integration: A proposed nosology for diagnosis. American Journal of Occupational Therapy, 61, 135-141.
Reynolds, S., and Lane, S. J. (2009). Sensory overresponsivity and anxiety in children with ADHD. American Journal of Occupational Therapy, 63(4), 433-440.
Thaker, G. K. (2008). Neurophysiological endophenotypes across bipolar and schizophrenia psychosis. Schizophr Bull, 34(4), 760-773.
Van Hulle, C. A., Shirtcliff, E. A., Lemery-Chalfant, K., & Goldsmith, H. H. (2012). Genetic and environmental influences on individual differences in cortisol level and circadian rhythm in middle childhood. Hormones and Behavior, 62(1), 36–42. https://doi.org/10.1016/j.yhbeh.2012.04.014
Yeap, S., Kelly, S. P., Reilly, R. B., Thakore, J. H., & Foxe, J. J. (2009). Visual sensory processing deficits in patients with bipolar disorder revealed through high-density electrical mapping. Journal of Psychiatry & Neuroscience: JPN, 34(6), 459–464.
Youngstrom, E. A., Arnold, L. E., & Frazier, T. W. (2010). Bipolar and ADHD comorbidity: Both artifact and outgrowth of shared mechanisms. Clinical Psychology: A Publication of the Division of Clinical Psychology of the American Psychological Association, 17(4), 350–359. https://doi.org/10.1111/j.1468-2850.2010.01226.x
Citation
Quint, N. (2016). Making sense of meltdowns: how to identify and intervene for children with sensory-based disruptive behaviors. OccupationalTherapy.com, Article 3474. Retrieved from http://OccupationalTherapy.com
