Jennifer: Thanks everyone for being here. I want to go over a few disclosures before I begin. I am the owner of Valley Pediatric Feeding LLC in Boise, and I provide therapy services to children. I have been paid an honorarium from occupationaltherapy.com for this presentation. I donate monetary funds to Smile Train, St Jude's Children's Research Hospital, and the Ronald McDonald House Charities of Idaho. I am an ASHA member, ISHA member, a Dysphagia Research Society member, a SIG 13 member, and also a board-certified specialist in swallowing and swallowing disorders.
Where Am I Coming From?
I want to give you a little bit of background about where I am coming from. I am a speech-language pathologist. We come from very different fields. I have taken many sensory courses, but occupational therapists are the experts. When I complete an evaluation, I understand the sensory areas that are involved in a child's functioning, and the symptoms that I could possibly see. I do have some knowledge about sensory issues that are important to a child with a feeding problem.
Looking at the Sensory Moment
What is happening at that very moment when we see a difficulty with a child's feeding?
- What does the child see?
- What sounds are associated with mealtimes?
- How does a child touch a food?
- How does smell affect a child’s participation with a food?
- How does a child taste/eat a food?
- What is a child’s focus at meals?
When there is food in front of him, what does the child see? What sounds are associated with mealtimes? How is that child responding to the clanking in a kitchen? Is mom at the stove or is dad at the grill? How does the child interact with the food? Do they use their hands or only utensils? How does smell affect the child's participation with food? Are there any aversive behaviors? Does the child lick, taste, nibble, or eat the food? Does the child take good-sized bites of foods when eating? How does that process break down? What is the child's overall focus at mealtime? How attentive is that child to the food that is in front of them, on their plate and at the table?
I created this diagram to show that breakdown of everything that we just talked about.
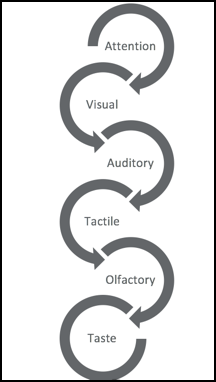
Figure 1. Sensory moment components.
The first thing that we need to look at is the child's overall attention because that is going to cascade down to all of the other sensory areas that are included in a mealtime experience. How well can that child focus? How does that impact the child's visual interaction with foods? How then does that impact what that child is hearing? How does that impact their interaction or tactile component of mealtime? Finally, we need to look at smell and taste. Everything builds upon each other. We are also going to talk about a lot of the concerns that parents bring to us regarding all of these sensory areas.
What Brings You Here Today?
My first question that I pose to parents when they come in is, "What brings you here today?" I want to know their concerns about their child's eating. During this initial interview, this is the first chance I get to hear the family's overall concerns with the child's eating. It can bring out sensory concerns that are related to feeding difficulties that they are dealing with day in and day out. This then allows us to dive deeper into the sensory aspects. It also gives me more information as to whether this child has more than just an oral sensory feeding problem. If a child is having significant sensory difficulties in other areas, then that is going to be a signal to me to make that referral to occupational therapy, or to talk to the physician about referring the child to OT.
Questions to Ask Regarding Sensory-Based Feeding Deficits
Initial questions that I ask parents when I am looking at a sensory-based feeding deficit are:
- Do certain smells bother your child?
- What kind of food textures are typical in your child’s diet?
- What textures does your child avoid?
- Does your child have a color preference with foods?
- Does your child do better with more or less food on her plate?
- Is your child distracted at meals?
- How well does your child attend to food/meals?
What smells bother your child? This might give me some information about what foods are accepted and which ones are rejected. What kind of food textures are typical in your child's diet? This gives me information about how a child deals with textures in their mouth. Do they like foods with more texture or things that are softer? What kind of textures does your child avoid? What particular foods are refused? Does your child have a color preference with food? This one is probably not thought of as much, but I think from our experience working with children on the autism spectrum, sometimes we see color preferences to neutral colors. Does your child do better with more or less food on their plate? Food might be overwhelming to a child. Are they distracted at meals. We will talk more specifically about that later, but it gives me some information about how motivating the food is that is being presented. Then lastly, how well does your child attend to food and meals? How attentive a child is to particular foods, and is attention lost if there are foods that are presented that are avoided?
Typical Comments from Parents
Let's now get into some of the comments that I typically hear from families when they come in for a feeding evaluation.
"My child does not chew food."
From a sensory perspective…
- How does the bite size of a food affect chewing?
- How does the texture of a food impact how well a child chews it?
- Are there any foods that would elicit more chewing?
Initially when I hear this comment, I automatically think that it is a problem with oral motor skills, but there are also sensory-based problems that can lead to decreased chewing. I might ask them more detailed questions such as, "Does bite size affect the food that is being chewed?" Maybe they can chew small bites, but not larger bites of food. Their mouth may become overwhelmed with a larger bite of food and cannot respond by chewing to make it manageable. How does texture of a food impact how well a child chews it? Maybe a child can chew other foods that have a lot of texture to it like a cracker, but not other foods that are softer like a piece of banana. Lastly, are there any foods that would elicit more chewing? Are there foods that a child refuses that lead to better chewing? Why is that child avoiding those foods in the first place?
“My child gags and vomits when he eats ___.”
From a sensory perspective…
- Where is the gag reflex positioned within the mouth?
- What types of foods lead to gagging and vomiting?
- What are the sensory properties of those foods?
- How large of a bite may elicit gagging and vomiting?
We can fill in that blank with lots of different foods. I am sure you have heard lots of different stories from families. From a sensory perspective, the child may have a very hyper-responsive gag reflex. We need to test to see where this gag reflex is and what foods are leading to gagging and vomiting? The gag reflex may be set off by texture-specific foods. What are the sensory properties of those particular foods. A child may eat some soft foods, but not others. What is specific to a particular food that is leading to difficulties? Again, we also want to look at the size of the bite. Could smaller bites be managed better?
“My daughter won’t drink from a cup.”
From a sensory perspective…
- Why does a child like or dislike the feeling of the cup at the mouth versus a bottle or Sippy cup?
- Does the child prefer a bottle because of the soothing/self-regulation that it gives, which is missing from an open cup?
- Does the flow of liquid alter how well a child accepts a different vessel?
- Are there environmental implications on what vessel a child will drink from?
Is there an aversion to the vessel that is being presented? Why does a child like or dislike the feeling of a cup in the mouth versus a bottle or maybe a sippy cup? What the refusal is behind that situation? Often children enjoy the overall soothing or self-regulation that sucking from a cup provides. This is a very specific relationship within sensory processing. I also want to think about the flow of liquid and how that is altered with a cup versus what happens with a bottle. What is the speed of the liquid that is coming into the mouth? How is that liquid being channeled into the mouth? This is very different from a nipple on a bottle to an open cup. What are the environmental implications of why a child will not drink from a cup. If this is an only child, there might not be any other models of other children using a cup. Parents drinking from a cup are not necessarily a motivator for them to work on cup drinking.
"My son spits out fruits and vegetables."
From a sensory perspective…
- What is aversive about fruits and vegetables? Taste? Texture?
- Is there a form that a child may be able to ingest a fruit or vegetable?
- Has there been a point in the past where the child actually ate these foods?
- What kind of reaction does the child receive with this behavior?
I think when we look at picky eaters, fruits and vegetables are the main food groups that are typically rejected. What is aversive about those fruits and vegetables? Is it their taste or texture? Is it the diversity of color? The colors may be overwhelming because they are so bright. Is there a fruit or vegetable form that a child may ingest? Sometimes a child will eat raw baby carrots, and that is their only vegetable and the only "form" (small, crunchy) that they like. Will they take it in another form? Some examples are vegetable chips or freeze-dried fruits that can also be crunchy. Will those be accepted in place of a fresh fruit or vegetable? Was there a point where the child ate these foods, and then these foods were lost? Why and when were those foods lost? Was there a precipitating factor behind that loss? Lastly, if a child is spitting food out, I want to look at the kind of reaction that the child is receiving from the parent. The parent may give a negative response, like "We don't do that.," or "You don't spit out your food." That reaction may be reinforcing to the child in some sort of way.
“My son can’t be in the kitchen when I am cooking.”
From a sensory perspective...
- What is bothersome – smell, sight of food?
- Is the entire environment just too over-stimulating?
- How does the food preparation environment negatively affect the mealtime?
What are all the precipitating factors of surrounding a food before it is presented for eating. Is it the smell of the food as it is being cooked? Is it the sight of the food when it is out? Is the entire environment too overstimulating? Perhaps there is banging going on around the stove, the fan might be on during the cooking process, or there are lots of smells. The whole environment could be too busy and overstimulating. How does all of this negatively affect the mealtime? Has there been so much sensory overload during meal prep that it carries over into the mealtime? We also need to look at how the family is responding to that situation.
“My child won’t eat around other children.”
From a sensory perspective...
- What are the precipitating factors for not participating in social eating situations? – sight of other foods, smells of those foods, the way other children eat?
- How distracting is the whole situation?
- Which people does a child do well with in terms of eating a meal?
Are there precipitating factors for that child not participating in social eating? Are the foods that the other children are eating bothersome? Are all the different smells of the different foods competing with each other and that is problematic? Do some children get bothered by the way other people eat, especially if a child is sitting next to a relatively messy eater? I also look at how distracting the whole situation is. Eating at home is a very controlled situation, but when they are eating in a social situation, there are many different things going on. We might even ask, "Is there a social situation that a child could eat with other people?" This give me information about a positive situation, and how I can build on that in order for a child to improve in his social eating.
“My child has a meltdown every time I give her ___.”
From a sensory perspective...
- What is the most bothersome aspect of the food that is offered?
- Are there patterns to the foods that are refused?
- Could just the “newness” of a food be the problem?
- What are the interactions between the child and parent that may impact the situation where new foods are offered?
We can fill that blank in with lots of different foods. What is the underlying sensory reason why that tantrum is occurring in the first place? What is most bothersome about the food that is being presented? Are there patterns to the foods when a child has a tantrum and is refusing that food? What type of things are we seeing? Could this just be the newness of a food? Maybe a parent is trying a brand new food, and that is when these tantrums occur. We could ask the caregiver if there is less of a meltdown with a new food that is new but similar to familiar foods. This is going to give me information about how we present new foods. What are the interactions between the child and parent that may impact the situation when new foods are offered. I am looking at the response that the child is getting from the parent, and how the parent is handling those situations as a whole.
“My daughter will only eat foods that are brown, yellow, and white.”
From a sensory perspective...
- Why are those colors preferred? What may be soothing about them?
- Why are other colors refused?
- Does the child make an association about a specific color that is negative towards food? Is this association from past experiences? Can you even find the pattern?
What do they normally eat? What are the colors? Why are those colors actually preferred by the child? What could be soothing about them? Why are other colors refused? With an older child, I can ask them directly about their color choices to get their perspective.
