Editor's note: This text-based course is a transcript of the webinar, Executive Functions And Motor Control: Opportunities And Limitations For Occupational Performance, presented by Nicole Quint, Dr.OT, OTR/L.
*Please also use the handout with this text course to supplement the material.
Learning Outcomes
After this course, participants will be able to analyze recent evidence correlating motor control and executive functioning, including limitations to practice application.
After this course, participants will be able to apply evidence-based approaches to enhance executive functioning through motor-based interventions.
After this course, participants will be able to evaluate the effectiveness of the practice of utilizing motor-based executive functioning approaches through occupational performance.
Introduction
We have an hour together, and I will be moving a little quickly since this session is intended for an advanced level. I have another course on this platform that focuses on motor learning, so if you’d like to revisit that for more foundational information, I highly recommend it. During this session, I’ll also use some of the same motor learning approaches, which may help reinforce and expand on what you've already learned.
Development of EF Skills
This discussion centers on the interplay between executive function and motor learning, and how these two domains develop in tandem. In the past, they were often viewed as separate aspects of development, but emerging research is revealing that they are, in fact, deeply intertwined. This growing evidence proves clinically valuable, especially concerning specific populations and diagnostic characteristics. It allows us to better tailor our interventions by understanding that individuals will likely experience a more successful transition into adulthood when they possess strong executive function, refined motor learning abilities, and solid motor control. These are areas that, when supported early, yield a meaningful return on investment in terms of long-term outcomes.
While early intervention is widely recognized as critical, it is particularly significant for developing executive function skills between the ages of three and five. This stage marks a child’s initial experiences with conflict resolution, whether in school or at home with siblings. It’s a period where physical responses begin to be supplemented—and eventually replaced—by language and social negotiation. Major developmental shifts in attention systems make this a dynamic and transformative period.
The difference between three and five-year-olds is quite dramatic, and four-year-olds often show a transitional blend of skills. During this time, executive dysfunction or related challenges tied to neurodevelopmental and other pediatric disorders frequently become more evident. Clinicians will start to notice certain children standing out in preschool settings. It’s common to inquire during intake how the child managed during their preschool years, as this can offer critical insight. Parents often report concerns such as difficulty sitting during circle time, frequent behavioral challenges, or trouble engaging in play with peers. Sometimes, children require the support of a one-on-one aide or paraprofessional. These observations often point to underlying issues with executive function, particularly inhibition.
Inhibition is a foundational executive function skill that typically solidifies around the age of four. From that point forward, while the complexity of inhibitory control may evolve, the basic capacity tends to remain stable. This makes the preschool period an essential window for identifying and addressing such issues. When working with older children, asking about their preschool experiences can offer valuable retrospective insight. If you work with them while they are still in preschool, you can gather direct and immediate information about their developmental trajectory.
The Big 3 of EF
- Inhibition
- Impulse Control
- Requires arbitrary rule be held in mind while inhibiting one response to produce alternative response
- Socially acceptable behavior
- Working Memory
- Ability to store, update, and manipulate/process information over short periods of time
- Limited-capacity information-processing system
- Verbal, visuo-spatial, and coordinating central executive
- Cognitive Flexibility
- Ability to think flexibly and shift perspective and approaches easily, critical to learning new ideas (different perspectives)
- Requires inhibition and WM processes
- Switching between two or more mental sets with each set containing several tasks rules
The three main components of executive function—identified by Best and Miller in a landmark 2010 study—represent a significant shift in how we conceptualize and approach executive function in research and clinical practice. Before their framework, executive function was often treated as a disjointed collection of skills, leaving clinicians to sort through an overwhelming list with little guidance on where to begin. This often resulted in a bottom-up strategy, attempting to fix everything at once without a clear roadmap. The Best and Miller model brought clarity and focus by identifying three core components: inhibition, working memory, and cognitive flexibility.
Inhibition, or impulse control, is the first and most foundational of the three. It typically solidifies by around four years of age. Inhibition requires holding an arbitrary rule in the mind and using it to suppress a habitual or impulsive response in favor of a more appropriate one. The classic example is the “cookie test,” in which a child is told not to eat a cookie or donut while an adult steps out of the room. The child’s ability to resist the immediate temptation reveals their level of inhibitory control. Inhibition is the cornerstone of socially acceptable behavior. However, it is essential to note that children don’t typically learn inhibition through feedback alone. Instead, they need clear, explicit instructions to understand when and how they are being impulsive, as they rarely internalize the lesson from natural consequences alone. This has significant implications for clinical work, emphasizing the need to teach and reinforce self-regulation strategies directly.
Working memory develops gradually and steadily across childhood and adulthood, closely tracking language development. It involves the short-term storage, updating, and manipulation of information. One way to conceptualize it is like packing a suitcase: you can only take what you pack, and if you pack the wrong things, you’ll be unprepared. The same principle applies to working memory—if a child doesn’t focus on or encode the right information, they will struggle with completing tasks. Working memory has a limited capacity. For children, this might mean holding only a few items at a time, while for adults, the typical span is around five to six items. Working memory encompasses verbal and visual-spatial information and functions like an air traffic control system. This central executive system evaluates what information should be prioritized and how it should be managed. Interestingly, our reliance on working memory has shifted; we no longer need to memorize phone numbers, so the demands placed on this system have evolved.
Cognitive flexibility, like working memory, continues to develop with age but typically lags a bit behind. It involves shifting perspective, considering alternative strategies, and adapting to changing circumstances. This mental agility is vital for problem-solving and understanding other people’s viewpoints. Cognitive flexibility depends on inhibition and working memory, so delays in this area often trace back to challenges in one or both domains. If a child struggles with cognitive flexibility, it’s usually worth circling back to inhibition first, especially given its early developmental window. Effective cognitive flexibility also requires shifting between different mental sets, maintaining rules, and adjusting to task demands—again, highlighting the interaction between working memory and inhibition.
These three core functions form the scaffolding for higher-order executive processes, including metacognition, planning, organization, and materials management. They are also deeply intertwined with motor learning and motor control, underscoring the importance of holistically addressing them when working with children across developmental stages.
Dynamic Systems Theory: Motor Learning and Motor Control
This framework is rooted in dynamic systems theory, which emphasizes the interaction of three critical elements: the task, the individual, and the environment. While the theory often refers to the "task" in general terms, in occupational therapy, the focus should be on the occupation—the meaningful activity in which the individual is engaged.
The individual encompasses the person's physical, cognitive, emotional, and sensory capacities, while the environment includes both the physical setting and the social and cultural context in which the occupation occurs. These three components are continuously interacting, and it is through this interplay that movement and function emerge.
Motor control, within this framework, refers to the ability to execute motor tasks in response to the specific demands of the environment. It’s about performance—how effectively the individual can carry out a movement or action within a given context. In contrast, motor learning is how these tasks are learned and refined over time. It involves acquiring or improving new skills through practice, feedback, and adaptation to environmental demands.
Understanding this distinction is key: motor control concerns current ability, while motor learning concerns the ongoing development process. Both are shaped by the dynamic relationship between the individual, the task, and the environment, reinforcing the importance of addressing all three elements in therapeutic practice.
Occupational Performance
When we approach this from an occupational therapy perspective, particularly in the context of occupational performance, we start by considering motor control in terms of how an individual can successfully execute a task within a specific environment. It's about asking, "What does this person need to do to complete this occupation?" and "What do they need to learn or refine to do it effectively?" Execution isn't simply about moving; it's about how that movement is carried out—how well-coordinated, purposeful, and efficient it is within the environmental and task constraints.
During execution, we’re addressing several integrated components. Coordination is central, as are fluency and fluidity—the smooth, rhythmic quality of movement that allows it to appear effortless. Balance is another critical piece, both static and dynamic. This includes managing righting and equilibrium reactions, which help maintain posture and respond to environmental shifts. At the same time, the individual must remain aware of their surroundings, adapting to what’s happening in real time while staying focused on the task.
Theoretically, optimal occupational performance (Figure 1) occurs where all these elements—task demands, individual capabilities, and environmental context—intersect seamlessly, like a Venn diagram with perfect overlap. Of course, in practice, this ideal convergence is rare. Life is messy, dynamic, and unpredictable. But that sweet spot, where everything aligns just right, remains our goal. We work to help our clients move as close to that overlap as possible, recognizing that it's in this integration that meaningful participation and function truly occur.
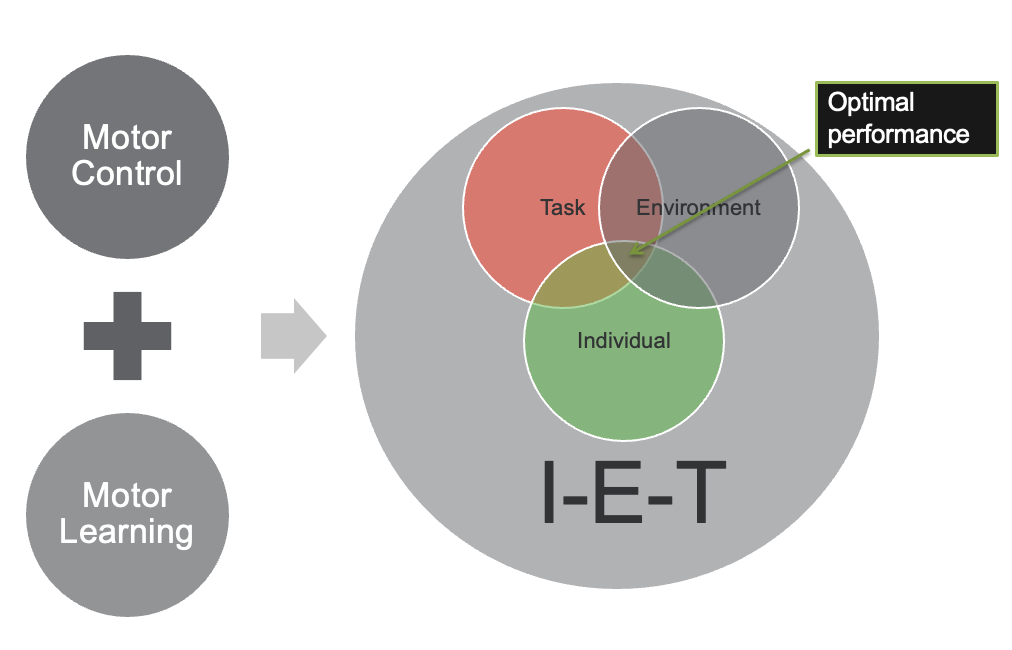
Figure 1. Optimal performance between the individual, the environment, and the task.
It doesn’t usually happen that way in real life. That perfect overlap between the task, the individual, and the environment—the ideal balance where optimal performance occurs—is rare. As therapists, we’re often working within the gaps. Our job becomes identifying which component is out of alignment. Is the task too demanding? Is the environment creating unnecessary barriers? Or does the individual need to develop additional skills or support to meet the demands?
We constantly evaluate and adjust these variables, like balancing the size and weight of circles in that conceptual Venn diagram. If one circle is too large, the task is too complex, or the environment is overstimulating, it can throw everything off. Likewise, if the individual's skill set is still developing or limited in some way, they may not yet be able to meet those external demands.
The therapeutic process involves modifying and shaping these elements to align more harmoniously. This might mean adapting the environment, simplifying the task, or providing targeted interventions to enhance the individual’s capabilities. The goal is to align those three circles closer, creating a better chance for meaningful, effective occupational performance. This analysis and adjustment process is how we bring everything together and move toward that ideal balance, even if we never reach it perfectly.
Tasks (Occupations)
- Movement Ongoing
- Discrete: fixed beginning/end (taking a shot in basketball)
- Serial: a series of discrete (dance routine)
- Continuous: no distinct beginning/ end (running)
- Stability Mobility Continuum
- Consider the base of support
- Stable or mobile
- Open v. Closed
- Closed: predictable and static environment (movement can be planned/ executed in advance, requires precision/accuracy)
- Open: a dynamic and changing environment, required to adapt
When we analyze motor tasks, it's important to understand that movement is an ongoing process. I’ve created a similar presentation that dives deeper into this topic, so if you’ve taken that course, what I’m about to describe should feel familiar and build upon it.
Movement tasks can be categorized in various ways. One way is through discrete, serial, and continuous classifications. A discrete movement has a fixed beginning and end. For example, if I take a foul shot in basketball, the action has a clear start and stop. But if I continue shooting foul shots one after another, that sequence becomes serial—essentially a series of discrete actions strung together. Think of a dance routine or a choreographed cheerleading performance; these, too, are serial because they involve sequences of individual steps.
In contrast, continuous movements don’t have a distinct beginning or end. Walking and running fall into this category. It’s hard to pinpoint exactly where the movement starts and stops—it just flows.
Another essential concept is the stability–mobility continuum. Every movement falls somewhere on this spectrum. To determine where, I look at the base of support and how balance reactions come into play. Is the movement more stable or more mobile? Take the example of shooting basketballs again: if I’m standing in one place and someone feeds me balls, I’m pretty stable. I’m not shifting my base or reacting to anything unpredictable. But the task demands much more mobility if I start running around the court, collecting balls, turning, and shooting. Even the ball is more dynamic in this scenario, so I have to adjust my base of support more frequently. This shift toward mobility introduces complexity, not just in the lower body but also in the trunk and upper limbs. Shooting while jumping or balancing on one leg introduces yet another layer of mobility, with trunk rotation and reaching outside the base of support all coming into play.
Then we have the concept of open versus closed motor tasks. A closed task happens in a predictable, controlled environment. The person performing it can anticipate how it will play out, allowing precision and planning. Again, sticking with the basketball analogy, imagine me standing in one place and shooting repeatedly, just like those basketball arcade games. The environment is controlled, the variables are minimal, and the feedback is consistent. But as soon as I start moving, catching balls from different angles, and adjusting for new positions, the task becomes open. Suppose I'm in a real game, unpredictability skyrockets. A defender might swat the ball, forcing me to react in real-time. That’s the nature of open tasks—they require adaptability because the environment is constantly changing.
I see this in therapy and play settings, too. Take Connect 4, for instance. The traditional version is closed—you pick up a chip, line it up, and drop it into a slot. The movement is predictable. But there’s another version—maybe you’ve played it—where you flick the chip with a tab, trying to get it into a cup. That version is far more dynamic. It’s open, with variability in distance, angle, and force. It’s fun but more challenging, making it an excellent activity for developing adaptive motor planning.
Someone once asked me whether the open-closed and stability-mobility distinctions are part of the same continuum. It’s a fantastic question. While they’re related, they are separate dimensions. More mobile tasks are often more open, but it’s not a hard-and-fast rule. They can align, but they don’t always.
When observing someone learning a new motor task, think about a specific child you know—maybe a child you’re working with, your son or daughter, or a neighbor’s kid. Picture them learning to swim, catch a ball, or master a new game. You can see the learning process in their movements—the hesitations, the adjustments, the trial-and-error. These observable behaviors give us valuable insight into where they are on the learning continuum. Through this lens, we begin to understand the mechanics of movement and the journey of acquiring it.
Fitts & Posner 3-Stage Model
This is Fitts and Posner's three-stage model.
- Cognitive Level
- High cognitive activity
- Movement: Slow, inconsistent, inefficient; fixing present
- Requires visual attention; large parts of movement controlled consciously
- Associative Level
- Learner selects best strategies
- Movements: More fluid, reliable, efficient
- Decreased cognitive demands
- Autonomous Level
- Low degree of attention for success; movement controlled automatically
- Movements: accurate, consistent, efficient
- Can divert attention to other aspects of activity rather than motor
I often refer to this as the golden rule for analyzing someone's learning process—understanding their stage. At the cognitive level of motor learning, the individual puts in a lot of mental effort. The cognitive demand is high, so movements are slow, inconsistent, and inefficient. You’ll observe behaviors that suggest the person is trying to stabilize themselves, fixing or freezing parts of their body to create a sense of control. It makes sense; when something is hard, people naturally try to reduce the variables by anchoring themselves somehow.
I’ve seen this in so many situations. For instance, when someone is just learning to juggle, their eyes are locked on the balls, their hands are rigid, and everything is happening at a painstakingly slow pace. Every part of the movement is controlled consciously, which can be incredibly draining. And they make a lot of mistakes. This is where frustration tends to set in, especially for kids. They might feel overwhelmed and disheartened, which is often the point where they’re tempted to give up.
As therapists or educators, our response is often to break the task down into smaller components, which can be helpful. However, we must also guide them toward integration, helping them progress to the next stage: the associative level. At this stage, the learner starts to receive feedback from the task and begins selecting better strategies based on what works. Movements become more fluid, efficient, and reliable. They start recognizing patterns: “When I move my arm this way, I get a better result,” or “If I apply more pressure here, it works more consistently.”
This pattern recognition is a sign that they’re problem-solving in real time. The cognitive load lightens because they rely more on proprioceptive and kinesthetic feedback. Visual monitoring decreases, and the body moves to match the task's demands. Mistakes still happen, but now they’re learning from them. The process becomes less frustrating, and they might even say, “Hey, I think I’m getting this.” That’s a decisive moment.
Then there’s the autonomous level. At this point, the individual performs the task almost effortlessly. The movement is fluid, accurate, and consistent. They’re no longer thinking through each motion consciously—it’s become automatic. And here’s where something fascinating happens: they can begin to multitask. Their attention is freed up to focus on higher-level executive functions because the motor aspects of the task are running in the background, almost like muscle memory. However, if a child is stuck in the cognitive phase, they can’t engage those executive functions. You won’t get that beautiful overlap of motor skill, cognition, and context that we aim for in occupational performance.
Someone once asked me if the arrow between these stages could move backward. It’s a great question. Typically, the arrow points forward because with practice and consistency, people tend to improve. But yes, regression can happen—especially if a child is dealing with a medical issue, like a chronic illness or brain injury. I remember working with children who had seizures or even a hemispherectomy. In those cases, you can see a return to the cognitive level, where we start over.
However, regression usually occurs outside major medical events only when the challenge increases. If you raise the difficulty of a task, you might see someone who had been at the associative level slip back into more cognitive patterns temporarily. That’s not necessarily a bad thing. It just means they’re now learning something new within that skill set. And if the task remains unchanged, muscle memory should eventually kick in, and they’ll continue progressing.
So yes, the arrow generally points forward—but it's not rigid. Life, illness, and task demands can bend that path. The key is guiding, adjusting, and supporting the learner through it.
Link Between EF and Motor Control
What's the link between executive function and motor control?
- Sequencing and WM
- Temporal binding effective
- Inhibition: slow, sustained activities
- Hebbian’s Law:
- Neural synchrony for attention
- Anticipation for memory
- Temporal binding for fluency
Sequencing and working memory are deeply interconnected. You're inherently drawing on working memory when engaging a child—or anyone—in tasks requiring sequencing. A clear example is the use of obstacle courses in therapy sessions. When a course involves multiple steps that the child must remember and complete in a specific order, it becomes a sequencing event, placing high demand on working memory. This demand increases when the child must plan their actions, mentally rehearsing the sequence before and during the task. In contrast, if the course permits spontaneous participation with no required order, the load on working memory is significantly reduced.
Another central concept is temporal binding, grounded in Hebbian’s law, which states, “Neurons that fire together, wire together.” This is not just a theory—it’s a foundational neuroplasticity principle explaining how repeated and coordinated neural activity strengthens skills over time. Temporal binding refers to linking sequences of events through time, which plays a vital role in developing fluency in movement.
Anyone who has practiced piano with a metronome or used tools like Interactive Metronome has experienced this phenomenon. Aligning movements with a rhythmic beat—such as timing a basketball shot to a consistent pulse—supports the development of fluent, precise motor patterns. The rhythm acts as a scaffold, guiding the body and reinforcing the brain's neural pathways. It enhances motor control and sharpens focus, making it a powerful tool in skill acquisition and attentional training.
In terms of inhibition, slow, sustained activities can be especially practical. Introducing tasks that require stillness or stability can help build inhibitory strength when a child struggles with impulsivity or poor motor control. Activities that involve holding a posture or maintaining balance force the child to slow down and act intentionally. In these moments, they must remember a rule—like “don’t step off the line” or “wait your turn”—and resist the urge to act on impulse. This is where meaningful progress happens, as motor and executive functioning capacities are challenged and strengthened.
Hebbian’s law also applies to the concept of neural synchrony for attention. The goal is to help children maintain sustained focus by synchronizing their brain activity around a single stimulus. Focused attention builds vigilance, which can be supported by reducing environmental distractions. Positioning a child in a prone position can eliminate peripheral visual input, and using a dimly lit room with a flashlight can direct their focus to a single point. These strategies help organize the nervous system and reinforce attentional pathways.
Anticipation is another powerful element in preparing the brain for memory formation. Whether it's the introduction of a new object, the turn-taking structure of a game, or a verbal cue signaling action, anticipation primes the brain for engagement. The child becomes alert, and their system is ready to respond. This state of readiness changes the brain’s electrical polarity, setting the stage for stronger neural connections. That “firing and wiring” effect is a direct route to building working memory.
Embedding anticipation into activities is highly effective for truly supporting working memory development. When combined with sequencing, you naturally enhance both participation and cognitive retention. This is why practices like Taekwondo are so beneficial—they integrate sequencing, rhythm, anticipation, and controlled movement. These elements collectively activate neuroplasticity and support motor and executive function development in a structured, engaging way.
Research
I’ve compiled a collection of evidence to support the concepts we've discussed and to provide a well-rounded understanding of the topic. The selection includes high-level research like systematic reviews and meta-analyses, which offer strong, generalizable conclusions based on rigorous methodology. These help establish a solid foundation for what works and why. I’ve also included observational and comparative studies that bring in the practical, real-world nuances controlled trials may not fully capture. This mix allows us to see which interventions are effective and how they function across different settings, populations, and challenges, giving us insight into both outcomes and implementation.
Authors and Date | Type of Study | Study Results | Application to Practice |
Bugner et al., 2021 | Systematic Review | •EF improvements linked to motor learning, especially with structured and varied practice | •Use motor learning principles (Fitts & Posner) to design therapy activities |
Bao et al., 2024 | Meta-Analysis | •Found small positive association between motor competence and EF •General motor competence, locomotor, object control, and stability associated with EF •Children and adolescents | •Interventions targeting children’s motor competence may be a promising strategy to improve EF |
Richter et al., 2024 | Observational Study | •Parents rated ADHD children lower in EF; motor assessments confirmed impairments | •Combine parent reports with performance-based measures for ADHD evaluations |
Pan et al., 2019 | Pilot study of 12-week table tennis program with ADHD group | •ADHD training group scored significantly higher in locomotor, object-control, and cog tests | •Consider table tennis as potential clinically relevant approach* |
Pan et al., 2024 | Comparative Study | •Motor-EF association stronger in autistic children, supporting early intervention. | •Address motor-EF links in OT for ASD to prevent developmental delays |
Albuquerque et al. 2022 | Cross-Sectional Study | •Found significant EF-motor links in children, especially ages 6-8 | •Support early concurrent development of motor control and EF |
In the material I’ve shared, you'll see that I’ve curated a diverse range of sources to support the ideas we’ve been exploring. I’ve included links to these studies wherever possible, though not all are open access. Still, I made a deliberate effort to select resources that are accessible to most people and that offer meaningful insights for clinical reasoning and intervention planning.
Fitts and Posner's motor learning framework is one foundational model that shows up consistently in the evidence. It’s well-established and provides a clear structure for designing therapy interventions. This model helps you determine where a child is in their motor learning progression—whether they’re operating at the cognitive, associative, or autonomous stage—and allows you to tailor interventions to match their current level of skill acquisition and support needs.
Solid evidence supports the idea that improving motor competence can enhance executive function, particularly in children with ADHD. One of the most important considerations in assessment for this population is the need to combine parent reports with performance-based evaluations. Research indicates that parents of children with ADHD often report lower levels of functioning than what is observed in direct assessment. If you rely solely on parent feedback, the baseline may be skewed. Performance-based tools often paint a more accurate picture, especially in this group, whereas in other populations, parent reports tend to align more closely with actual performance.
A study by Pan and colleagues offers a great example of how a physical activity like table tennis can support executive function. In this study, children attended a table tennis camp and demonstrated gains in executive function from pre- to post-assessment. On the surface, table tennis may appear simple, but it incorporates essential motor and cognitive engagement components. The rhythmic auditory input supports temporal binding. The requirement to anticipate the ball’s movement and make fast, coordinated responses integrates motor fluency and executive control. It’s a great case of Hebbian learning in action. And while table tennis worked well in this context, the principles it involves—timing, anticipation, rhythm, adjustment—can easily be adapted to other games or therapeutic activities.
The evidence strongly supports addressing motor and executive function development together for children with autism. These areas tend to be delayed in children with ASD, but early intervention can improve functioning and may even mitigate the risk of further developmental delays. Starting early is critical. The earlier we intervene, the more responsive the brain is, especially during the developmental window between ages three and five.
Motor control and executive function develop in tandem, and this overlap is significant during early childhood. That’s when neuroplasticity is high, and intervention can shape long-term outcomes. I’ve included more detail in the material to help structure your early intervention strategies in a developmentally appropriate and effective way. By combining motor learning principles with targeted executive function support, we can design grounded, individualized, and deeply meaningful interventions.
Authors/ Year | Type of Study | Population/ Age Range | Key Takeaways |
Strooband et al. (2020) | Systematic Review | Under 6 (FMC) | •Effective for FMC: •GMC •Consultation for FMC-no evidence of effectiveness |
Lelong et al. (2021) | Scoping Review | Children with ADHD | •Prevalence 30-52% motor problems, GM/ FM, gender, handedness not influence •Motor approaches effective, ranging 4-8 weeks with 3 weekly sessions •Feedback positive influence-children with ADHD rely more on visual feedback than NT controls (frequent to infrequent; auditory for graphomotor) |
Ruggeri et al., (2020) | Systematic Review | ASD | •83% have motor issues •Motor skill acquisition improved with visual vs. verbal instructions, but equally well adult, robot, or peer |
Dapp et al., (2021) | Longitudinal Switzerland (PE constant)
| K-18 mos. later 3x/week 90 min+ | •Differentiated approach uses physical activity, enhances GM skills •PA positively affects mental health •Generalize: structured PA has biggest effect; nonsignificant trend in FM benefits with structured PA only |
Shi et al., 2022 | Systematic Review | Typical | •Acute and long-term moderate intensity 30-50 min, 3x/wk for 17 weeks+ have positive effects on executive function •Acute, closed skills more effective for inhibition Open skills more effective for WM, CF •Open-continuous and closed-sequential are most efficient •Long-term, open, sequential, and open-sequential are more effective |
We know that motor learning is highly effective for improving fine and gross motor coordination. However, when it comes to fine motor coordination specifically, consultation alone—without active practice—has not shown to be particularly effective. In one study, consultation-based interventions didn’t lead to significant gains. This reinforces what we know about motor learning: to improve motor skills, children must actually practice those skills. Simply training others to support the child or modifying tasks through consultation strategies isn’t enough unless true motor learning occurs.
In children with ADHD, there is a high prevalence of motor difficulties. Interestingly, handedness does not significantly influence these challenges, nor are there strong gender-based differences. Whether the motor issues are gross or fine, they tend to be similarly distributed. What’s encouraging is that motor-based interventions are effective. Ideally, these programs should be delivered over four to eight weeks, with three weekly sessions. While that might be difficult to achieve in some settings, incorporating elements of motor learning into home programs can also yield meaningful benefits.
Feedback plays a critical role for children with ADHD. They tend to rely more heavily on visual feedback than their neurotypical peers regarding gross and fine motor tasks. However, an interesting distinction emerges with graphomotor skills: auditory feedback seems more effective for those. It’s a curious finding, but it’s backed by research. So when you're working on handwriting or drawing tasks with children with ADHD, it may be more impactful to guide them verbally rather than visually. This nuance in feedback delivery is important and often overlooked.
When working with children with autism, we also see a high prevalence of motor difficulties—up to 83%, according to some studies. Fortunately, these children respond well to both visual and verbal feedback. And contrary to what was once believed, the source of the feedback—whether it’s a robot, a video, an adult, or a peer—doesn’t seem to matter as much. The takeaway here is that feedback can be effective, giving therapists flexibility in structuring interventions. While we often default to verbal feedback, especially in the clinic, we should remember that showing—offering visual feedback—is just as powerful, especially for individuals with ASD.
Physical activity is another area that has shown significant mental health benefits for children, and it can be an essential way to enhance gross motor development. One study involving kindergarteners examined long-term effects of increased physical activity and found that children who engaged in at least 90 minutes of physical activity three times a week showed improved gross motor skills even 18 months later. Activities like soccer or other structured sports can be tremendously beneficial, yet we don’t always think to recommend them as part of a therapeutic plan. The dosage here is also worth noting: 90 minutes or more, three times a week, is a strong benchmark for outcomes related to both physical and cognitive development.
In terms of structured intervention, research suggests that moderate-intensity activities conducted three times per week for at least 17 weeks positively affect executive function. More specifically, closed skills—predictable, structured activities—are especially effective for improving inhibition. That makes intuitive sense because closed skills allow for planning and rule adherence. Conversely, open skills involving unpredictable and dynamic environments are more effective for enhancing working memory and cognitive flexibility. These activities demand constant adjustment and adaptation, which engage those executive domains more intensely.
Interestingly, the research points to open, continuous activities and closed, sequential tasks as the most efficient overall for supporting executive function. Open continuous activities—like walking or running through a nature trail—lack a defined beginning and end and require ongoing adjustment. These promote cognitive flexibility and memory. On the other hand, closed sequential tasks—such as structured basketball drills repeated in sets—are great for working memory and inhibition. For instance, you might ask a child to perform ten repetitions of several drills in sequence: dribbling through the legs, figure eights, then shooting. They must remember the order, track how many reps they’ve completed, and hold back from jumping to their favorite part of the routine. That combination challenges both memory and self-regulation.
We’re seeing consistent patterns emerge in the research, which is exciting. These findings give us practical, evidence-based ways to refine our approaches and tailor interventions to the unique needs of each child.
Evaluation
- Early Identification and Screening Crucial
- Motor and executive function (EF) should be assessed early, particularly in children with movement difficulties.
- EF deficits, especially in working memory, correlate with motor control challenges.
- Use a variety of assessment tools to capture both motor and EF skills
- ADHD Specific
- Children with ADHD can perform worse on motor / EF tasks compared to NT peers
- Parent-reported measures tend to underestimate abilities
- Best practice: Combine parent reports with objective performance-based tests for a more comprehensive evaluation
- Autism Specific
- Relationship between motor skills and EF is stronger in ASD than in NT peers
- Addressing EF-motor links early in OT interventions can prevent cascading developmental challenges
- Assess both FMC and GMC when evaluating executive function in autistic children
- Motor Learning Based
- EF improvements are linked to structured motor learning, particularly gross and serial motor skills in closed or stationary environments
- Use Fitts & Posner’s motor learning framework to assess how children adapt to new motor tasks and executive demands
- EF Based
- ADHD: Response inhibition and WM
- ASD: Prioritize cognitive flexibility and planning tasks
- DCD: Prioritize WM and planning tasks
- Use multiple types: BRIEF, performance-based, naturalistic, play-based, goal-directed tasks, and daily routines will give more accurate picture
Evaluating executive function in young children, especially those around three, is definitely a challenge. One of the questions that often comes up is whether subjective or objective assessments are available for this age group. The short answer is: it’s complicated. Executive function is difficult to measure in a standardized way for such young children, largely because their developmental variability is high and their behaviors are so context-dependent.
For the younger kids, observation is often the most reliable and informative approach. Watching how a child responds in natural settings—how they manage transitions, delay gratification, or follow directions—gives you valuable insight into their executive functioning. For example, you can use a simple task like “go, not go,” where the child has to inhibit an action. Say there’s a favorite toy in front of them—can they resist the impulse to go get it when asked to wait? That kind of test, though informal, taps directly into impulse control and behavioral regulation.
Similarly, you can observe how well a child follows directions for working memory. Following a one-step command might be expected at age three, but you can stretch the task slightly by introducing a few elements—asking them to carry out a task using two objects, for instance. These subtle challenges help you assess memory, attentional control, and cognitive flexibility.
As kids get older, there are some tools you can start to use. I’ve found a few free working memory assessments online that can be helpful. These aren’t necessarily norm-referenced but offer a good ballpark sense of capacity. Remember that children often score higher on these isolated digital tests than they do in functional tasks. If a child can remember five items in a structured, test-like setting, they may only manage three in real-world, dynamic environments. That’s a vital calibration point when interpreting results.
Regarding standardized tools, the BRIEF (Behavior Rating Inventory of Executive Function) is one of the more well-known assessments, although it’s better suited to slightly older children. There are some free options too, including the TXI (Texas Executive Function Inventory) series. There’s the DEXI for adults, TEXI for teens, and CHEXI (Child Executive Functioning Inventory) for children. The CHEXI starts around age four or five, though you’d want to verify that before using it in practice.
Ultimately, the best approach still leans heavily on observation for the little ones. Talking with teachers—especially those in preschool or daycare—can be incredibly insightful. They see the child functioning in a structured environment with peers and can often report on patterns or difficulties you might not witness during a single session. Likewise, parent input is critical, though it’s always important to cross-reference with performance-based observations.
I’ve also included a resource page with more structured information on evaluation to help pull everything together. It’s meant to be something you can return to as needed. The key takeaway is that while formal tools are limited for young children, a thoughtful blend of observation, collaboration, and informal tasks can provide meaningful insights into their executive functioning.
Clinical Decision-Making Tool: Intervention Activity Analysis Focusing on Motor and EF
So this is a tool that I basically created in Figure 2.
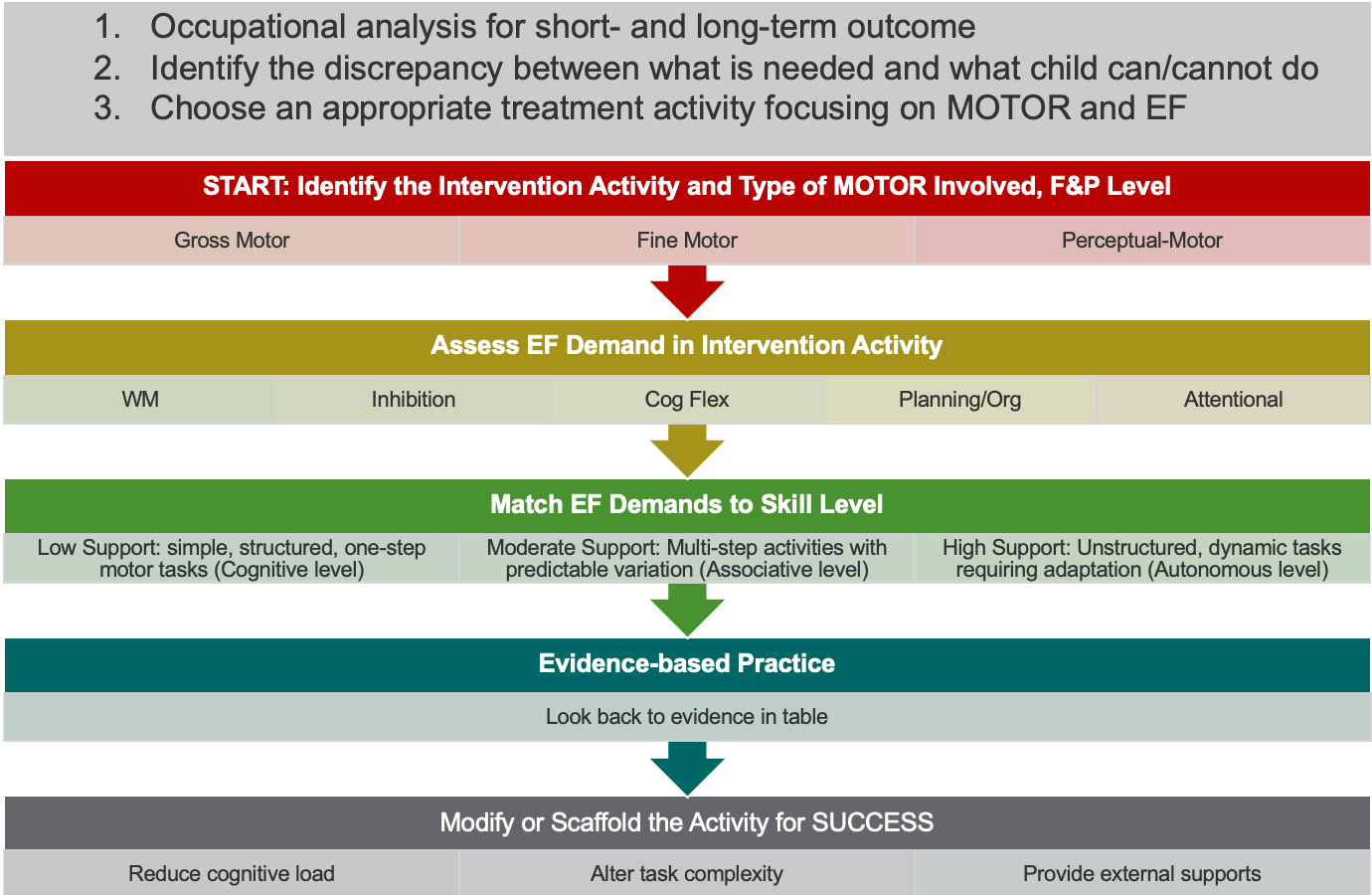
Figure 2. Clinical decision-making tool. (Click here to enlarge the image.)
This clinical decision-making tool is designed to help you create interventions grounded in activity analysis and integrate motor and executive function components. It's specifically tailored for an occupation-based approach—or at least, an occupation-centered one. That means we start with the occupation itself, break it down, and determine what the child can and cannot do within the requirements of that task.
Take bathing as an example. First, I analyze the context and environment: what kind of space is the child working in? Is it a bathtub, a shower, or a sink? Then I look at each step involved in bathing. Can the child initiate the task? Can they undress appropriately, lather soap, wash thoroughly, rinse, and dry off? I go through every part of the sequence. From there, I begin identifying where the breakdowns occur. Is the issue motor-based, like difficulty balancing while washing feet or poor coordination when scrubbing the scalp? Or is it executive function-based? Are they impulsive and skipping steps? Is working memory limiting their ability to remember the sequence of actions? Are they rigid in thinking and unable to problem-solve if their usual routine changes?
This is where we shine as occupational therapy practitioners. We are trained to look at function through both motor and cognitive lenses. Once I identify the areas of difficulty, I consider what type of motor challenge it is: gross motor, fine motor, or perceptual motor. I also reflect on where they are within the Fitts and Posner model—are they at the cognitive, associative, or autonomous stages? I probably don’t need to intervene if they're at the autonomous level. But if they’re at the cognitive or early associative stage, that’s where I need to direct my attention.
To determine their level, I observe them in action. Are they highly visually dependent? Do they seem frustrated? Are they making many mistakes or relying heavily on trial and error? That tells me they’re still in the cognitive phase. If they refine their approach, become more fluid, and show increased accuracy, they’re likely in the associative stage.
Next, I examine which executive functions are at play. Is working memory an issue? Is inhibition a struggle? Is attentional control weak? If I suspect cognitive flexibility is the issue, I often revisit inhibition and working memory first. Similarly, if attention is problematic, I might start there. However, when both inhibition and working memory are involved, I typically focus on inhibition because it offers a stronger return on investment at that stage of development. Modifying for inhibition is also more difficult, whereas working memory can often be scaffolded more easily.
Then I match executive function demands to the child's current skill level. If the child functions cognitively, I begin with low-support tasks—simple, structured, one-step activities. For those in the associative phase, I move to moderate-support activities with multiple steps and some predictable variation. If they’re at the autonomous level, they're likely functioning with high support capacity, meaning they can self-adapt and manage unexpected challenges in real time.
This is where evidence-based practice comes into play. I refer back to motor learning literature to guide my choices. I consider dosage—how frequently and for how long interventions should be delivered. I think about whether the child has ADHD, autism, developmental coordination disorder, or more generalized concerns. The approach needs to match the child’s specific profile. I also incorporate concepts from Hebbian learning—temporal binding, sustained attention, anticipation—to design interventions that promote neural change.
With this information, I modify or scaffold the activity for success. This might mean reducing the cognitive load, altering the complexity of the task, or providing external support. I consider the three core elements: the task, the environment, and the individual. If the task is too demanding, I simplify it. If the child is overwhelmed by cognitive demands, I make it more manageable, sometimes by focusing solely on inhibition or attention. If the environment is contributing to the difficulty, I adjust it. Maybe I dim the lights or reduce background noise to minimize distractions.
When I alter the task, I consider its structure. Is it open or closed? Is it stable or mobile? Is it a discrete or continuous action? These elements shape how I challenge the child and guide them toward success. By weaving all of this together—motor learning principles, executive function insights, and an occupation-centered analysis—I can deliver targeted, evidence-based interventions that are both meaningful and effective.
Jamari: 8-Year-Old With DCD
Let's look at Jamari. We've talked a little bit about ADHD and autism, but what I want to talk about is DCD. Many of us will see kids with DCD, and there is some research to help with that.
Basketball (Occupational Analysis)
- GM
- Dribbling
- Shooting
- Ball skills
- EF
- WM: Sequence
- Inhibition: Fouls, shot choice, dribble direction
- CF: changing plan
- Context:
- Practice
- Flooring
- HORSE vs. skill drills, vs. practice games, vs. games
- F&P
- Dribbling: Cog Level
- Shooting: Associative level
- Ball skills: Cog Level
- Has never played a game
You chose a fun and meaningful theme—March Madness and basketball—and it's a strong example of how occupation-based activities can drive therapeutic engagement and outcomes. Basketball is not only enjoyable for many kids, but it’s also rich with opportunities to target both motor and executive functioning skills in a functional and motivating way.
In this case, you’ve identified a child deeply interested in basketball, even though he struggles with playing it. That spark of interest is precisely where we want to begin. His favorite subjects are science and reading, and he has a pet turtle named P.B. and J., which gives us a wonderful glimpse into his personality and potential motivators. But the key challenge here is that while he enjoys basketball as a spectator, he has difficulty participating in it, particularly because of difficulties following two- to three-step directions and managing tasks with multiple steps, which are clear signs of working memory challenges.
These working memory difficulties are spilling over into other meaningful areas of his life, like his desire to lead science activities. It’s easy to see how following a sequence of steps or instructions in an experiment would be difficult for him. Additionally, he’s facing challenges in his ADLs—buttoning shirts, tying shoes, and packing his backpack. These all point to deficits in fine motor and perceptual motor skills and executive functioning, especially around task sequencing, organization, and follow-through. He likely struggles with remembering steps and coordinating bimanual tasks when grooming, bathing, or completing chores. There’s probably some reduced task quality too, simply because of the underlying executive and motor integration issues.
So if we know he wants to play basketball, let’s lean into that and use it as the anchor for an occupation-centered approach. An accurate occupational analysis of basketball reveals that it’s a predominantly gross motor activity that also heavily draws on cognitive processes. On the motor side, we have dribbling, shooting, catching, and passing—all requiring coordination, timing, and spatial awareness. From the executive function side, basketball involves significant working memory demands (remembering rules and play sequences), inhibition (resisting the urge to shoot when it’s not a good choice, managing physical impulses during defense), and cognitive flexibility (adjusting your actions based on how the game is unfolding in real time).
In practice, basketball looks different depending on the context. Practicing dribbling in a quiet gym is not the same as playing a game of H-O-R-S-E, which requires planning and adapting based on where your opponent shoots from. A one-on-one match or a group game brings yet another layer of complexity—social cues, rule adherence, turn-taking, and quick decision-making. The setting matters too. Shooting on a low basket in the clinic versus a regulation-height hoop in a gym demands different levels of strength, coordination, and visual-motor planning.
Using Fitz and Posner’s model helps you identify their motor learning stage across different skills. He’s at the cognitive level for dribbling and ball handling—likely needing lots of visual attention, making frequent errors, and showing frustration. Shooting seems to be a little more developed; he’s at the associative stage, beginning to use feedback and refine. He’s never played in a real game, so we know game participation would represent a novel task for him, likely demanding a return to cognitive-level learning.
The beauty of using basketball as your therapeutic medium is that it naturally incorporates his executive function challenges. You can shape the activity to target working memory by creating structured sequences—perhaps asking him to perform a three-part dribbling pattern or shoot from specific spots in a particular order. For inhibition, you might have him pause before shooting, or build in a rule that he can only shoot after bouncing the ball a set number of times. To build cognitive flexibility, set up scenarios that require him to change his plan based on cues, like switching hands mid-dribble or deciding when to pass instead of shoot.
By embedding these executive function demands into a meaningful, motivating activity like basketball, you’re honoring his interests and directly addressing his developmental needs. This is the essence of occupation-based therapy—starting from what matters to the child and building function from there.
START: Identify the Intervention Activity and Type of MOTOR Involved, F&P Level
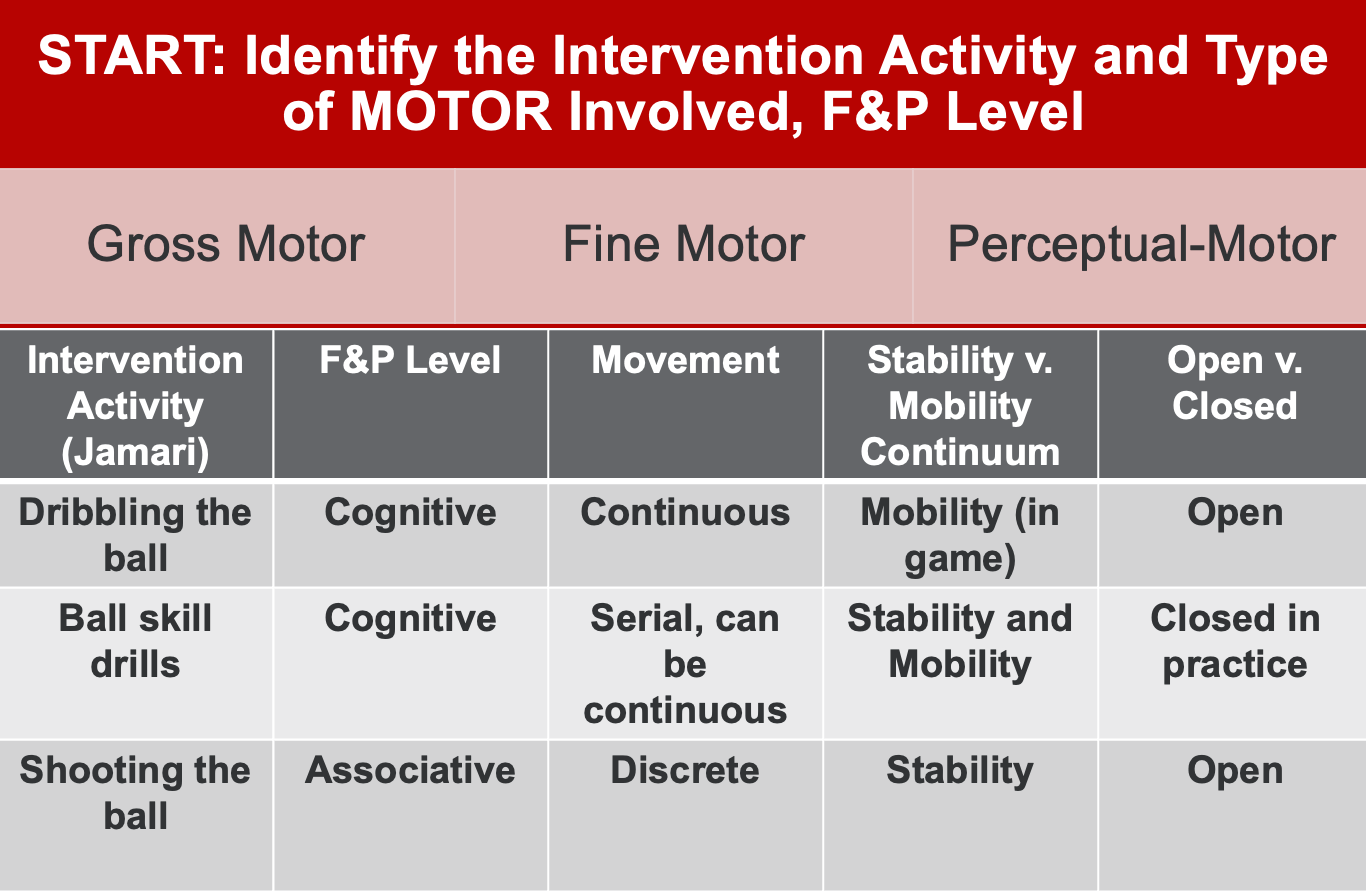
Figure 3. Example of a treatment plan.
So when we begin intervention with this child, we will start with simpler, more structured formats like skill drills and H-O-R-S-E-style games. The goal is not to immediately overwhelm him with complex, unpredictable tasks but to build a solid foundation of skill and confidence. We must carefully plan what we want to work on, aligning the level of challenge with where he is in his motor learning process.
For example, if we focus on dribbling—a skill he’s currently at the cognitive phase with—we recognize that this movement pattern is more continuous in nature. In a real basketball game, dribbling is highly mobile. The player moves across the court, adjusts directions, and adapts to defenders, all while maintaining control of the ball. That’s a lot of motor and executive demand. But we can dial that complexity down significantly by modifying the task to fit a more developmentally appropriate level.
Having him dribble in place removes much of the mobility demand and emphasizes upper limb coordination and ball control. Now, his support base remains static, and the task becomes more stable, allowing him to better focus on timing and rhythm. The ball becomes the only moving part, simplifying the experience and reducing the overall challenge. This makes the task far more accessible and less likely to produce frustration.
From an open vs. closed task perspective, dribbling is inherently more open than other activities, simply because your hand is not continuously in contact with the ball. There's inherent variability, and that can introduce inconsistency. But again, we can structure the practice environment to reduce some unpredictability. Keeping the surface flat and the task repetitive makes it feel more closed and controlled.
When we move into ball skill drills—around the world, figure eights, through-the-leg patterns, or catching and passing—we're still in the cognitive phase with him. These tasks are great because they can be made serial in structure. For instance, he can do ten figure eights, then ten bounce passes, then ten shots. That structure creates clear beginnings and ends to each task, helping reinforce sequencing and working memory. It also gives us a great opportunity to gradually increase executive function demand—maybe by asking him to remember the order of drills or self-monitor his repetitions.
Again, depending on how they're performed, these tasks can be designed to emphasize stability or mobility. If he’s doing figure eights while standing still, he’s in a stable posture. But if we ask him to walk while doing them, the mobility demand increases substantially. The same goes for catching or passing—standing still and tossing the ball back and forth is very different from moving and catching on the run.
Shooting, on the other hand, is a skill he’s beginning to develop; he's likely in the associative stage here. It’s a discrete task with a clear beginning and end: lift, aim, release. This kind of movement can also be modified for stability. He can practice shooting from a fixed position on the floor—feet set, focus on technique—making it far more manageable. But if we add movement, like having him catch and shoot on the move or pivot before shooting, we increase the challenge by introducing mobility and variability. The practice setting helps determine how open or closed the task is. Repetitive shooting in the same context is relatively closed; game-like shooting, where the ball comes from different angles, is much more open.
By understanding where he is developmentally for each skill and carefully adjusting the task demands—dribbling in place vs. on the move, serial drills vs. continuous play, stability vs. mobility—we create an environment where he can experience success and gradually build his capacity. The richness of basketball as an occupation-based tool lies in its flexibility. We can align each activity with his motor learning level and executive function profile with just a few adjustments, allowing him to develop confidence, skill, and greater independence across settings.
Executive Function Demand
Let's now take a look at executive function demand in Figure 4.
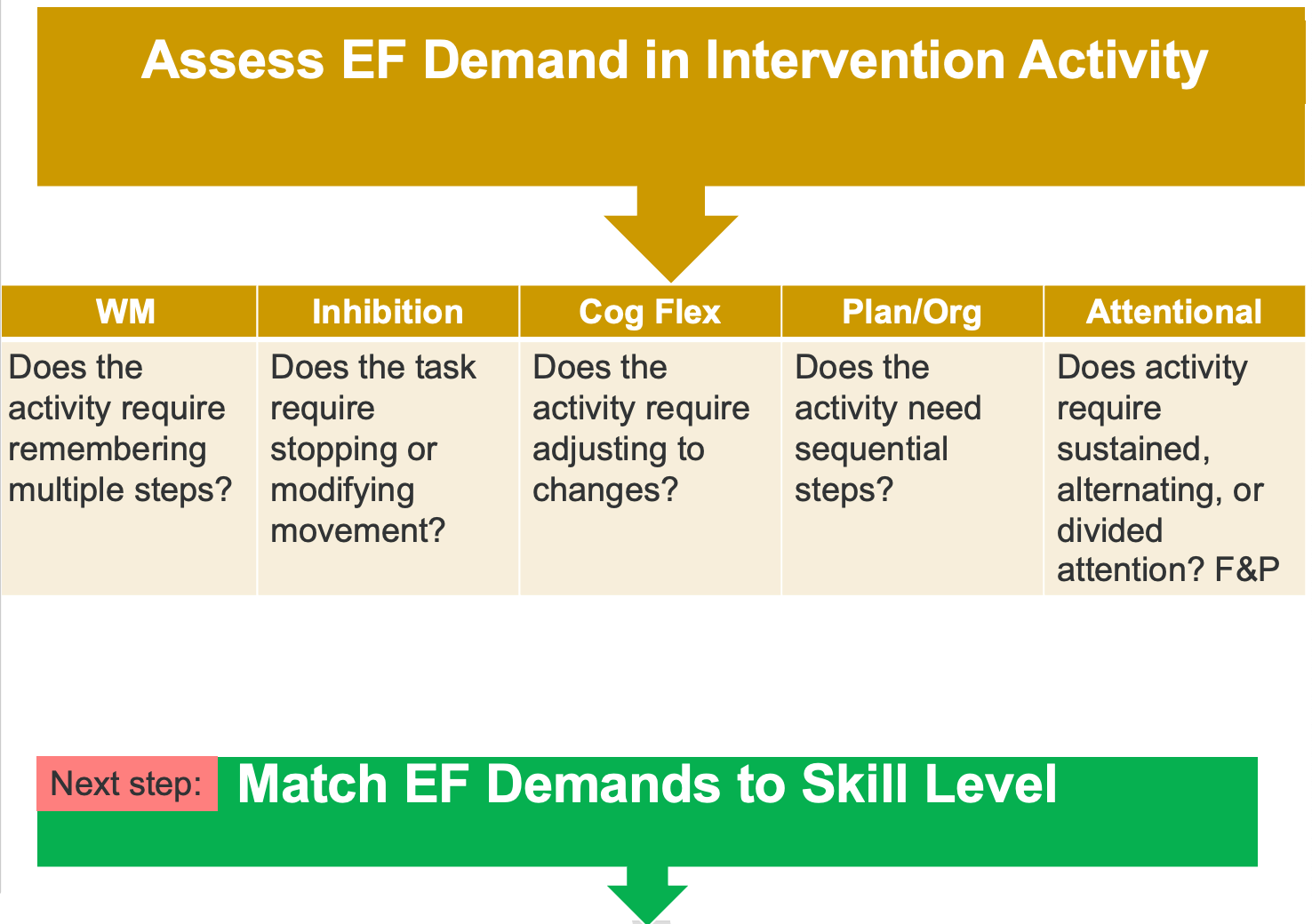
Figure 4. Executive function demand.
As you delve deeper into activity analysis and intervention planning, you ask guiding questions connecting motor performance with executive function demands. These questions form the core of your clinical reasoning and help identify the specific cognitive skills required by a given task.
One of the first things to consider is whether the activity requires remembering steps. If it does, then you're addressing working memory. Many daily routines—like dressing, grooming, or conducting a classroom science experiment—require a child to hold and manipulate information over a sequence of actions. When a child struggles here, they may forget steps, skip parts of a task, or need repeated prompts to complete the activity.
Next, ask whether the task requires the child to stop or modify their movement. This speaks to inhibition. For example, does the child need to resist an impulse to act too quickly, such as waiting their turn during a group game, following a "freeze" cue, or choosing not to shoot the basketball just because they have the ball in hand? A child with poor inhibition might act too soon, struggle with self-control, or make errors due to an inability to suppress automatic responses.
You should also consider whether the child needs to adjust to changes during the task. This is a marker of cognitive flexibility. If the plan changes, the environment shifts, or if unexpected feedback requires a new approach, the child needs to be able to adapt. This is especially challenging for children who rely on routine, resist change, or get anxious when things are unexpected. A lack of flexibility may look like repeating the same ineffective strategy or shutting down in the face of a challenge.
Another foundational question is whether the task involves sequential steps. This overlaps with working memory and emphasizes broader task planning and organizational abilities. Many activities, from tying shoes to completing classroom assignments, depend on the ability to understand and execute steps in the correct order. Difficulty with sequencing can lead to confusion, task avoidance, or incomplete performance.
Finally, assess the nature of the child's attention. Is it sustained, meaning the child can stay focused on a single task for an extended period? This foundation usually aligns with the cognitive stage of motor learning. If the child can shift their attention back and forth between two tasks, they’re demonstrating alternating attention, typically emerging at the associative stage. Divided attention—true multitasking—usually isn’t possible until a child reaches the autonomous stage, where the motor skill itself is automatic and doesn't require active cognitive oversight.
If a child cannot sustain attention, they will likely remain in the cognitive phase of motor learning. That’s a clear signal to start with simple tasks, reduce environmental distractions, and provide strong scaffolding through structure, routine, and repetition. As attention improves, you can layer in more complex demands—alternating and, eventually, divided attention. However, the process always starts with understanding exactly where the child is, what the activity demands, and how to bridge the two.
These questions aren't just checklists but key entry points into individualized, developmentally aligned intervention. They help you meet each child exactly where they are—cognitively and physically—and guide them toward meaningful, sustainable progress.
Match EF Demands to Skill Level
Figure 5 shows how to match those executive function demands to his skill level.
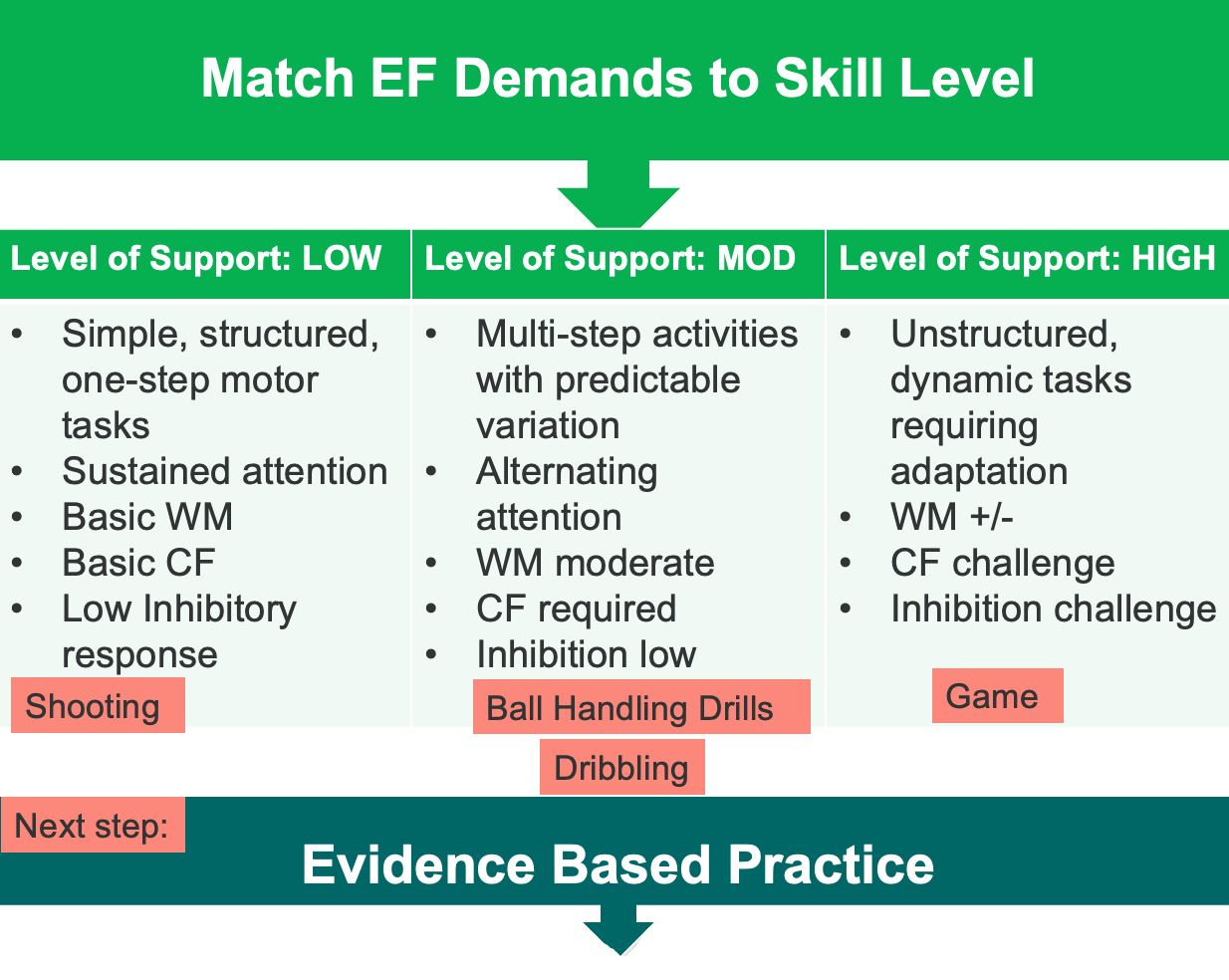
Figure 5. Ways to match EF demands to skill Level.
Now that I’ve identified he’s functioning at the cognitive level, most activities need to remain within a low level of support. That means choosing structured, predictable tasks focused on foundational executive functions, particularly early working memory, emerging cognitive flexibility, and minimal demands on inhibition. The motor tasks should be broken into one-step sequences so that he can develop fluency through repetition, build confidence, and reduce frustration.
I might set up a short series of three or four drills. These could include dribbling in place, basic bouncing and catching, two-handed tapping of the ball, or slow, controlled passes. A timer could structure duration and introduce rhythm, helping foster temporal binding and support motor planning. The session needs to feel steady and achievable, maintaining a calm and supportive tone that allows him to experience success.
With shooting, I can afford to increase the complexity slightly and move toward moderate support. He seems to be performing at an associative stage here, so he’s beginning to benefit from feedback and make refinements. I might have him shoot from different marked spots or follow a brief sequence—bounce once, aim, and shoot. These small layers of challenge elevate the executive demand in a manageable way, encouraging growth while minimizing the risk of overwhelm.
Dribbling can also begin to stretch slightly into more dynamic territory. I might try gentle walking while dribbling, or use short patterns such as two dribbles followed by a catch and repeat. If he’s successful with this, it may indicate he’s beginning to approach the associative stage in this skill. That gives me a signal that we can start nudging the activity toward more game-like elements down the line.
Complete gameplay, however, would fall into the high support category. This activity demands multitasking, spatial awareness, real-time decision-making, and more advanced motor coordination. He’s not ready for that yet, and introducing it too early could easily lead to breakdowns in performance and confidence. It’s essential to recognize that while gameplay is a long-term goal, we’re still laying the groundwork for it.
The focus remains on building fluency and comfort in the basics. As he becomes more proficient, I’ll gradually introduce variability—changing the space, timing, or order of tasks—to foster adaptability and build executive function. Each small step he masters becomes part of the foundation for broader, more complex participation in the future. This process of layered, intentional challenge ultimately supports both motor growth and cognitive integration.
Evidence-Based Practice
Evidence-based practice is shown in Figure 6.
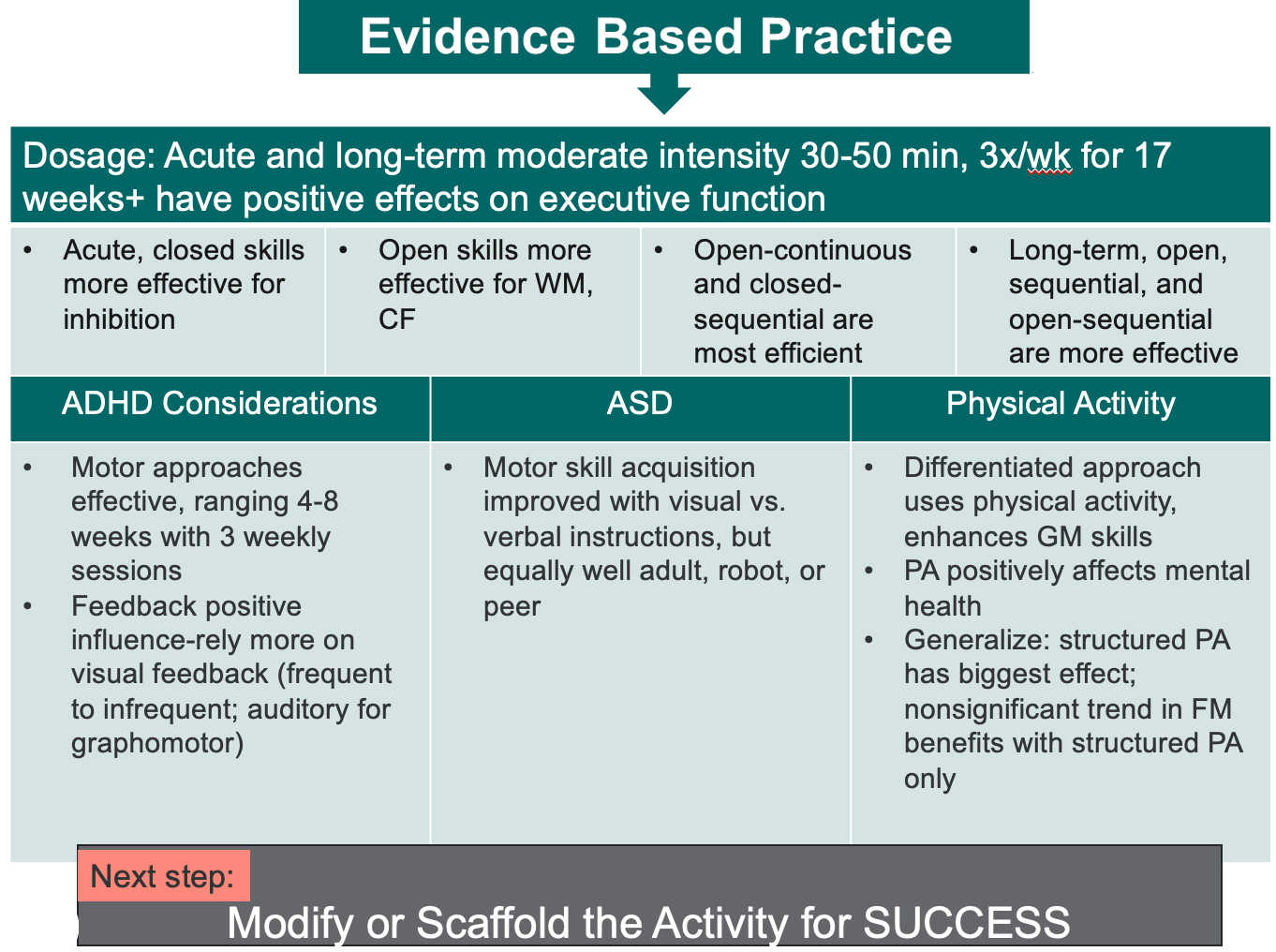
Figure 6. Evidence-based practice. (Click here to enlarge the image.)
This is where your clinical reasoning becomes essential. It’s the point where you take everything you've gathered—dosage guidelines, diagnostic considerations for ADHD and autism, the benefits of physical activity, and the unique motor and cognitive profiles associated with developmental coordination disorder—and start shaping a truly individualized intervention. This is the heart of good practice: drawing from evidence and translating it into meaningful, tailored support.
The dosage data gives you a structural foundation. If the research suggests three sessions per week over six to eight weeks to see measurable improvements in executive function, then that becomes a guide. Of course, real-world settings may not always accommodate that schedule, so you adapt. Maybe you extend the duration, integrate practice into daily routines, or offer carryover through home programming. But that benchmark gives you a target to work toward.
When you’re working with a child who has ADHD, you’re informed by evidence that shows visual feedback is particularly effective for gross and fine motor skills. In contrast, auditory feedback is more effective for graphomotor tasks like writing or drawing. That shapes your communication—maybe using visual modeling for a motor drill and verbal cues for a handwriting task. You also know these children thrive on structure, repetition, and predictability. So you design tasks that offer consistent practice and reinforce learning through patterns they can anticipate.
With autism, feedback delivery is more flexible. Whether provided by a peer, a video model, a therapist, or even a robot, the key matches the format to what engages the child. You’re not confined to a single strategy—you can shift between showing, telling, or demonstrating depending on the moment. That kind of flexibility allows for more responsive, personalized intervention.
For children with DCD, working memory support is especially important. That’s your cue to build in strategies that reduce cognitive load while enhancing recall. Use timers to create structure, consistent routines to build predictability, short verbal cues to anchor tasks, and visual prompts to support sequencing. Rhythmic elements—like beat patterns or timed sequences—can also enhance memory and motor fluency by linking actions to tempo and internal timing systems.
All of this—dosage, diagnosis-specific strategies, and your understanding of motor learning—comes together to guide your intervention choices. It’s not just about picking activities. It’s about knowing exactly why you’re selecting a particular task, how it supports motor coordination and executive functioning, and what adjustments will make the learning stick. This level of intentionality transforms good clinical work into great therapy, where every decision is purposeful and every moment is meaningful.
Treatment Plan: Jamari
- Dosage: Acute and long-term moderate intensity 30-50 min, 3x/wk. for 17 weeks+, have positive effects on executive function
- Dribbling
- Start: Discrete, stable, closed
- Challenge: move to open
- Move toward autonomous (varied practice)
- Shooting Baskets
- Open: Builds WM
- HORSE: Adds recall
- Create 3-5 step movement to shoot sequences
- Ball Drills
- Add sequence of 3-5 activities (around the world, figure 8s, bounce to wall, pass to person, etc.)
- Add anticipation for memory
- Dribbling
With Jamari, knowing that he has developmental coordination disorder (DCD), our intervention needs to be both evidence-based and closely aligned with his unique strengths and challenges. We’ve determined an appropriate dosage—structured practice delivered at the right frequency and intensity—and we’re starting with dribbling as a foundational skill. Since Jamari is currently in the cognitive stage of motor learning, our initial approach will be simple, structured, and predictable to help him develop fluency without overwhelming him.
Our ultimate goal is to guide him toward the autonomous stage, where movements become more fluid and less cognitively demanding. We’ll gradually introduce variability and complexity into the tasks to support that progression. With shooting, for example, we’ll begin in a closed, familiar format and then transition to more open contexts that require him to adjust his body position or respond to environmental cues. These added demands foster decision-making and adaptability, both supporting executive function growth.
To build working memory engagingly, we can use a game of H-O-R-S-E. This not only introduces fun and motivation, but also challenges Jamari to remember the position, form, and outcome of each shot. He has to recall and replicate, which strengthens memory in a meaningful, context-based way. We can also design three to five-step motor sequences—bounce twice, spin, pass, receive, shoot—that require him to retain and act on a short set of instructions. These sequences are developmentally appropriate and present just enough challenge to stretch his skills while keeping success within reach.
We’ll also use anticipation cues to prime his memory system. By telling him or showing him what’s coming next, we give his brain time to organize and prepare. This reduces cognitive load and supports smoother transitions between steps. Adding rhythm through auditory elements, like a metronome or hand clapping, reinforces timing and coordination. These rhythmic cues support temporal binding, helping him regulate pace and plan movements—key areas of need in DCD.
Through structured skill-building, engaging memory tasks, and using rhythm to enhance fluency, we’re developing an intervention plan that supports both motor and executive function. Most importantly, we’re doing this through an activity Jamari already enjoys. He gets to play basketball—an occupation that’s meaningful to him—while also building the physical and cognitive foundations that will help him succeed across many areas of life.
Modify and Scaffold the Activity for Success
And then we're modifying the activity for success.
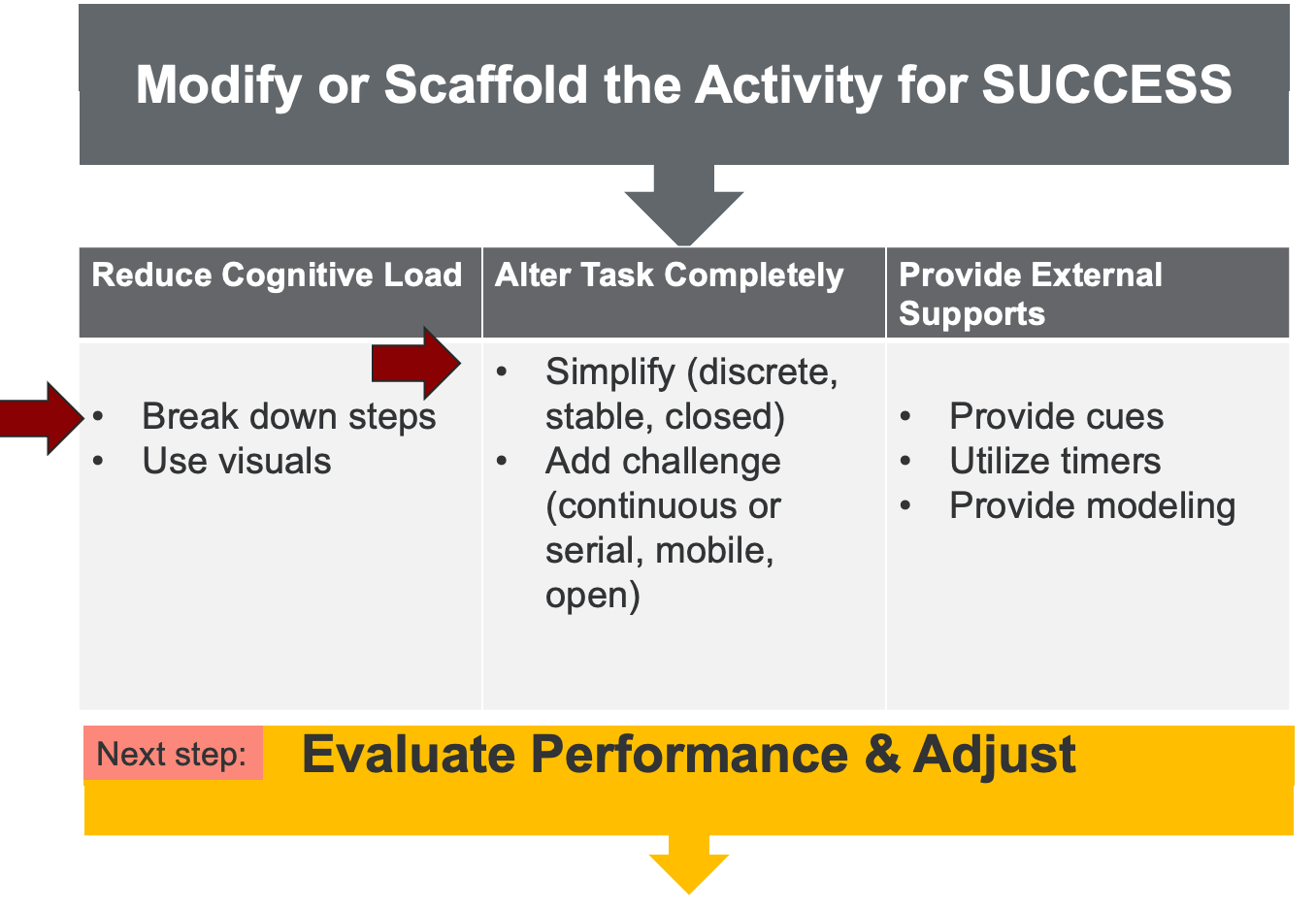
Figure 7. Ways to modify or scaffold the activity for success.
You can break down the steps, use visuals, simplify or challenge, use timers, provide modeling, and provide cues for external support. So, there are things that you already do, but now you're being more explicit about how you're doing them.
Evaluate Performance & Adjust
You're going to adjust as you evaluate his performance, as seen in Figure 8.
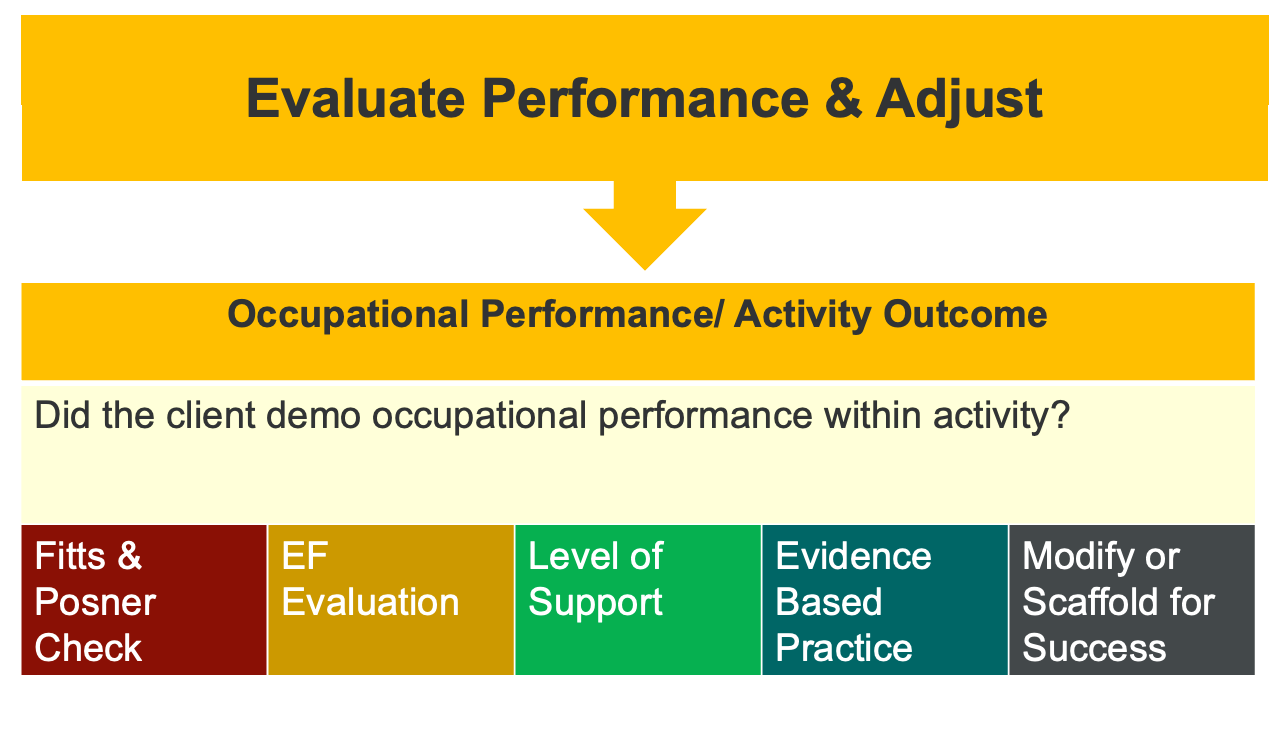
Figure 8. Ways to evaluate performance and adjust.
Now, you can look at the different levels and say, "I'm going to go back. Where is the challenge still happening?" I will go back, recapture it, and keep moving forward until I see him get to at least associative, highly associative, toward autonomous. I'd love to see him be able to join a basketball game and play if that's what he wants to do. In the meantime, I might do something like, hey, let's do some, join some physical exercise somewhere too.
Quick Recap: EF and Motor
- Motor and EF develop together
- Start with OCCUPATION and occupational performance
- Eval EF and Motor (Earlier is Better)
- Dosage, EF Focus, and Fitts & Posner
- Use Clinical Reasoning, EBP, and Adapt Interventions to meet just-right challenge
- Evaluate Performance and Continue to Progress
Executive function and motor development go hand in hand. The best place to begin is with an occupation—something meaningful to the child—because it provides natural context and motivation. From there, both the motor skills and the executive functioning components are evaluated. The earlier you can identify and address these challenges, the better the long-term outcomes will likely be.
As you design interventions, remember the dosage—how often and how intensely the child practices. Consider which executive functions are being targeted, and use the Fitts and Posner model to help you determine the child’s stage of motor learning: cognitive, associative, or autonomous. Let that framework guide the complexity of your tasks and the level of support you provide.
I’ve given you a process to follow, and you can lean into that. Use your clinical reasoning. Use evidence-based strategies. Adapt the interventions to meet the child where they are, aiming for that "just right" challenge, not too easy or hard. Then observe how they perform. Reflect on what went well, what still needs support, and where you might need to loop back in the Fitts and Posner continuum to keep progress moving forward.
We covered a lot in a short amount of time, and I know that the hour flew by. But everything we’ve gone through is there for you to revisit. You can go back, apply it to your caseload, and see how it fits. And now, before we wrap up, we want to support you further by going through the polling activity we had planned. Let’s take a look.
Summary
I hope this information was helpful to you. Thanks for joining me.
Questions and Answers
What are examples of visual feedback for individuals with ADHD?
Visual feedback refers to showing rather than telling. For individuals with ADHD, this can include using images, visual schedules, color-coded charts, modeling behaviors, or providing step-by-step visual instructions. It supports attention and memory by bypassing reliance on verbal (auditory) processing.
What does it mean to add "anticipation" to an activity?
Anticipation involves priming the system by letting the individual know something will happen. For example, saying, “At the end, you’ll have to catch a ball” or “Listen for a sound” helps their brain respond. This enhances engagement and memory encoding, which we often do instinctively.
What does “level of support” mean in this context?
"Level of support" refers to how much cognitive or sensory integration a task requires. A low level of support means the task is basic and doesn’t require much coordination or adaptive behavior. A high level of support means the task is more complex and requires more anticipation, adaptation, and integration of different skills. It can be confusing because “support” might sound like it refers to help from a person, but here it refers to the task demands.
Can you still work on executive functioning skills if the child is medicated?
Yes, absolutely. While there used to be a belief that medication made executive function training less effective, research now shows that skills can still be built even when a person is medicated. Interventions should continue, as medicines and skill development can complement each other.
References
See additional handout.
Citation
Quint, N. (2025). Executive functions and motor control: Opportunities and limitations for occupational performance. OccupationalTherapy.com, Article 5802. Available at www.occupationaltherapy.com
