Introduction: The "Before Times"
- OT at 2 intensive group homes
- Individual, group, and milieu intervention
- Team supports and trainings
- Leadership roles
- Treatment population and usual routines
- Trauma-informed treatment model: ARC
Before I talk about what happened this year, I want to talk a little bit about what my role looks like most of the time so that we have some context for what I provided before and what has changed. I work in two different group homes for the same agency. I am a full-time employee, but my schedule is split between these two sites. One site is for male-identifying clients and one is for female-identifying clients, and they both have about 15 residents. The age range is between 12 and 18 to 20, depending on the site. I have worked there for about seven years, and I was the first OT that was hired. We really spent a lot of time figuring out the best way to assimilate OT into Justice Resource Institute's existing structure and the trauma-informed treatment that was being provided there.
Typically, I complete evaluations and have a role within the clinical team to identify the best ways to support overall functioning using sensory regulation and modulation and cognitive strategies. I also do a lot of team projects depending on the needs of the program at the time. I provide individual intervention via three groups a week, and then milieu level intervention based on the needs of the program. I engage in monthly trainings and am involved in staff meetings for both programs focusing on a specific OT perspective and different treatment strategies.
I have also grown into some leadership roles at these sites. I participate in the administrative team that has supported many different changes in the culture and programming (macro-level). I also work on an individual micro-level with the kids.
All of our kids are at this time living outside of their home. They have been placed with us for different reasons and have experienced complex developmental trauma throughout their histories. Some common diagnoses that we see are PTSD, disruptive mood dysregulation disorder, reactive attachment disorder, anxiety, and depression. We also have some kids who are on the autism spectrum. There is a wide range of different diagnoses and functional deficits.
Our treatment model the ARC model or Attachment Regulation and Competency. We provide a safe environment whether that is thinking about us as caregivers or the physical environment that we provide to make sure that our kids are able to be comfortable and feel safe in order to build skills and move forward. We also work on regulation and energy modulation to build comfort in a situation and competency for skill development, enhanced executive functioning, and forming an identity.
Our program is a community-based group home. The kids are usually in school all day with structured programming occurring in the afternoon. The kids get home between two and three in the afternoon, and then we provide structure for decompression time. There are groups, mealtime, chores, and community outings. Our kids see their families either onsite, or they can go home. In fact, we have some kids who go home for whole weekends.
We do a variety of different things in the community from daily trips to the library and the YMCA to more paid activities on the weekend. There is a pretty steady structure most of the time.
March 2020
- What changed?
- No school
- No passes, visits, off-grounds activities
- Fear, anxiety, trauma response
- Staffing needs
- Disconnection from external resources
This brings us to March where everything changed. The first thing that happened is that there was no school. This was a huge disruption to the schedule as a huge chunk of the day where everyone had something to do was immediately removed.
We also were not able to send the kids out for passes, visits, or off-grounds activities. They were not able to go and see different family members, and we were not allowed to take them out either. There was a huge change in the rhythm of the day and our ability to fill that time with structure. Programs ebb and flow, but we do our best to keep things moving and consistent as much as possible. However, all of this came to a screeching halt in March and had a huge impact on the staff and the kids' ability to get through every day.
Another impact was fear and anxiety in the kids. They were initially very mad as they could not go anywhere or see their friends. As the reality of the situation started to settle in, they had more distressing questions like, "What happens if everyone here gets sick and you guys cannot come to work?" Or, 'What happens if we cannot get food?" Many of these kids lived through a variety of traumatic experiences, and their fears were not unfounded based on their histories including abandonment, neglect, and food scarcity. This is where their mind went immediately when they started to put the pieces together of the magnitude of the situation that we were facing.
In addition to that, we had a huge change in our staffing needs. With the kids home all day, we needed five staff members in the morning instead of just one during the first shift. This was a big change.
We were also really disconnected from our external resources. Typically, we have a lot of great people who fill a lot of different roles. We also rely on the help of mentors, school counselors, and other structured supports that our kids can go to. We could not go to the library or the YMCA. Our weekly dog therapy visits stopped as they could not come into the building. There was also a huge disconnect from the normal sort of web of resources that we have. On top of all of this, we could not go anywhere. Thus, 15 teenagers with many different issues and needs were all in the house together, and that was a lot of together time.
OT Role to Meet Changing Needs
- Routines & Rhythms
- Engagement
- Team Support
I am going to highlight these three categories: routines and rhythms, engagement, and team support. I worked to intervene and provide the best support I could to keep the program running and make the kids feel safe. A lot of what I am going to talk about are parts of my job anyway, but these things really became more of a focus. There was a big shift in perspective. As I talk through each section, I will point out where they overlap. Routines and rhythms and engagement are foundational concepts of the ARC model. I wanted to also highlight the team support that has been essential these past months.
Routines & Rhythms
- The ongoing link between OT practice and trauma-informed mental health treatment
- Our routines and systems provide a sense of felt safety
- The majority of our routines were disrupted and became out of our control
This has always been an area of niche intervention that I have focused on as a starting point for my OT role in the trauma-informed model. Routines and rhythms are part of the ARC language, but there is also a clear link to the routines and rituals that are part of the OT Practice Framework (OTPF). This is the starting point of how OT fits into this overall treatment. The daily routines and systems are how we feel safe in our environment. During March and April when many people were shifting to working from home and losing their routines, as a society, we talked about how important it was to stick to a routine to maintain a structure. This is so important for adults who are functioning in society. For my clients, this is something that is a huge need for them all the time and was more heightened during this time. The majority of our routines were disrupted, and the only thing we could do was maintain control over what was not disrupted.
- So what can we do? Identify and strengthen what we still have control over!
- Keep showing up
- Maintain programmatic routines and expectations: hygiene, meals, chores, activities, bedtimes
- Support remote schooling
- Maintain a connection to the rhythm of the year
The very first thing that we could do was show up and come to work every day. We needed to show the kids that we were going to be present and provide the care that they needed. One helpful change that occurred was that all of our corporate-level off-site team meetings were canceled. Thus, we were all hands on deck for months, and this allowed all of us to be present and provide support for both the staff and the kids. As this pandemic has continued, we have moved to two virtual platforms and have reinstated a lot of team meetings to maintain a connection to the larger agency. As a result, we have been more removed and have had less time to be on the floor. This is something we are still working through for the best balance for both the agency and the kids.
Every day, we have programmatic routines and expectations. Our kids get up, and they complete hygiene routines. We make sure that mealtimes are consistent. We do chores in the house so they can still earn an allowance. Typically, our kids are allowed to spend their allowance on the weekends. We had to have some flexibility in the way that we were able to maintain these routines. For example, instead of going to the store, they could use their allowance for Door Dash. They are still able to work towards something within that routine. We became a little more flexible in wake-up and bedtime routines. It took us a little bit of time to figure out what our new normal was going to look like, but once we did, we maintained consistency there.
A major adjustment that we had to make was adding tech time into the house. Typically, we do not allow the use of cell phones in the program. As the kids were more separated from all of their family and friends and external resources, we made an exception.
Between March and April, there were about three weeks in Massachusetts where the kids had no school. This was particularly challenging. However, once remote schooling began, we were able to think about how we could build our daily routines around that. There were some difficulties that we had to work through like space in the house. Space and our programs are not really set up to have 15 kids doing school all the same time. Our wifi was strained, and we had to make sure that everyone had the help that they needed. This was an area that I came in a lot. I was able to help kids adjust at the moment. "Okay, this worksheet is not working online, so let's print it out." Or, "Say your answers to me, and I'll help you type it." I was able to address their immediate needs and get their schoolwork done while keeping them engaged and regulated.
Using an OT perspective, I also looked at how to utilize the space in the house. We were able to use some basement space. I provided a number of tools like noise-canceling headphones, fidgets, and visuals for stretch breaks. I helped to build a routine into the school day to support remote schooling within this group home setting.
Something else that is particularly important under the umbrella of routines and rhythms is maintaining a connection to the rhythm of the year.
Birthday Celebrations.
The child gets to pick how they want to celebrate their special day in this program. Usually, kids spend their birthdays with their family, whether it is a visit on-site or an opportunity for them to have a pass. In the early months of the crisis, this was not a possibility. We had a number of kids, particularly our younger ones, who were very frustrated by this. I think the May birthdays actually had the hardest time because in Massachusetts that was when the initial stay-at-home order was set to end and then it did not. I helped them to regulate these emotions and figure out how to still make their birthday special. One way is that we customized birthday treats. Figure 1 shows all of the items I baked to support these celebrations.

Figure 1. Birthday treats.
One child turned 14 and wanted an ice cream cake (pink sprinkles). One of the boys wanted a marble cake so this was my first marble cake in the top right picture. It was an adventure, and he was very pleased with it. I also make some cookies and cream cupcakes down here in the lower left. I am going to talk more about this in engagement, but we need to think about the ways that we can meet the kids' individual interests and help build their identities, especially when they are not able to engage with family and normal plans. We can help them to feel safe, connected, and appreciated by our site and our caregivers in these small ways.
The picture in the top left shows some different supplies used for a spa day. This child was particularly disappointed because they were not able to go out for their birthday. We came up with a variety of spa activities in the house. Unfortunately, because of the way my schedule was, I was not there on her birthday. However, I was able to obtain everything that we needed and set it all up with instructions. It is important to stay flexible and meet the individual needs of these kids and help them feel special on their special day.
Holiday Rituals.
In addition to birthdays, holidays are also important to maintain. Participating in cultural and holiday rituals allows kids to have a sense of grounding and connection to the rhythm of the year. We still needed to experience 2020 even if it was a little bit different. For these kids, they are often in different placements so their traditions do not always look the same year to year. Thus, it was really important that we modeled how to embrace new traditions and making the best of it. This flexibility could help them in the future as well.
In April, we made sure that we participated in all of the typical Easter traditions. We made treat baskets, we dyed eggs, and had egg hunts. I personally stuffed all of the eggs with candy. This project that I have up here was a Zentangle group that I did with the kids (Figure 2).
Figure 2. Zentangle art project.
They really liked using this stress-reducing type of art and incorporating it into an Easter theme. We decorated the house so that they could have some fun with this new normal. There were a couple of different activities that I put together for the 4th of July weekend like sensory jars. We also did a cookout and provided water balloons. In May, we created cards for Mother's Day, and we did this for Father's Day as well because, at that point, we still were not able to do in-person visits. We also facilitated a number of Zoom calls between kids and their parents. Another activity we did was create colorful face masks as seen in Figure 3.

Figure 3. Colorful face masks.
Engagement
- OT role to be attuned to the interests and strengths of clients, provide access to materials and supplies
- Project materials: novel and familiar
- Supplies for clients on quarantine precautions
- Formal group sessions and organic small groups
Next, I want to move on to talking about engagement. Engagement encompasses a number of different things. As I mentioned earlier, it is one of the foundational concepts of our treatment model. It not only thinks about what we are doing but also how we are doing it. My particular role in engagement is being attuned to the interests and strengths of my clients and then providing access to the materials and supplies that they need to be able to participate in those things that they want to do and need to do. This is something that I do all of the time, but it became very heightened and important during this past year.
The first thing I had to do was get information. I had to gather intel from the kids about what they wanted to do and how they were going to keep themselves busy during all of this downtime. Once I gathered the information from the children, I went and cleared out Walmart several times to make sure that we had everything we needed to be able to support them moving forward. This is part of our art gallery in Figure 4.
Figure 4. Examples of art projects created by the kids.
The kids painted many pictures over those months and leaned into painting as a medium. Our whole program is covered in their beautiful artwork now. I wanted to make sure that they had access to these materials to engage them in things that were comfortable and familiar during this uncertain time. Additionally, I provided some novel activities so that they could mix it up and learn something new. We did everything from painting, tie-dye, Diamond Dots, puzzles, jewelry making, clay projects, and felt animals.
In addition to the general sort of milieu activities on the days that I was there, I also kept things stocked and organized for the weekends. I would leave a lineup of specific activities that I held for the weekend so that they could have something exciting to do on those days. We are going to get to staff in a little bit, but our staff was also really having a hard time. This was a really big undertaking to keep everyone safe and entertained. I wanted to provide as much support as I could for them so that they were able to engage with the kids in the best way possible.
In addition to that, we had a number of kids that had to be on quarantine precautions for a period of time. For example, if a kid went to the hospital and came back, or if they had gone missing and came back, they would have to be on quarantine until we were able to get a test or adequate time had passed. This has changed a little bit with more availability of testing now, but at the beginning, it was a full two week period. Quarantine was also initiated if someone had symptoms. The kids that were in quarantine felt even more disconnected from what was going on than the kids in the milieu. For them, I created personalized boxes of things that they could do while isolated. I made sure that they had coloring books that met their interests, the type and flavor of gum that they liked, and any regulation tools, like fidgets, to help them during this time.
I also kept up with my group schedule throughout this whole time. I felt that this was one thing that I had control over. If there were any kids on precautions and could not attend, I bagged up the activity for them so they could feel more involved. Maintaining these normal groups ties back to those routines and rhythms. I wanted to make sure that whatever we had control over, we were still doing. I kept up with those structured groups as well as formed some little organic small groups based on kids' interests. For example, I might have two or three kids who wanted to make lip gloss, make mochi, or bake something special. We would do that in addition to the regular weekly schedules. Right now, I am in the middle of a project with a bunch of the kids who wanted to make weighted bears.
Figure 5 shows a bulletin board we installed in April.
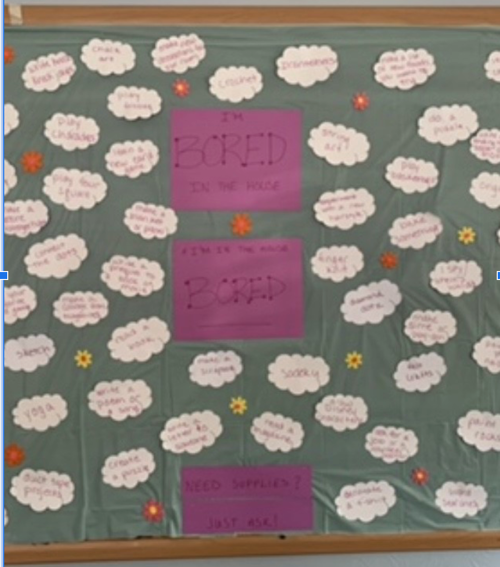
Figure 5. Bulletin board with activity ideas.
This is a little blurry, my apologies. This is a big bulletin board in the living room at one of the homes that provides activity ideas. I maintain this board. It has become a very useful tool to provide information for both the kids and the staff. The clouds are activity ideas. and there are about 70 of them on the board. I used a quote from a TikTok song that says, "I'm bored in the house and I'm in the house bored." The kids thought that was very funny. On the day that I put this up, they sang a song for about six hours. They are able to access any of these activity ideas and supplies. This was a proactive way to get the information out to the staff and the kids. As I said, the staff had been working non-stop. Some of them have their own kids, and they were struggling with coming up with activity ideas at this time. An important role I have is to make sure I know about the kids' interests and provide as many ideas and supplies as possible to help all the shifts run smoothly. Currently, I have a "fall fun" ideas board up so similar to this. This also ties into the routines and rhythms and engagement pieces to provide structure.
- Not just "stuff to do"
- Relating and responding effectively
- Being present
- Giving clients choices
- Managing our own emotions
- Navigating boundaries during a shared experience
As I said when I introduced the topic of engagement, this is not just about stuff to do, it is also about the way that we do it. It is how we as adults relate and respond effectively to the clients. It is being present and not being on our phones or distracted. We want to be in the moment.
It is important to give our clients choices. These past several months have included a huge loss of control for everybody. We want to make sure that we are still implementing opportunities for empowerment and choice-making whether that be letting the kids decide what they want on the meal schedule, incorporating them into choosing activity options, or even simply just giving them a choice of when in the day they want to do certain things.
Another big one is managing our own emotions. This has been a really stressful, scary, and uncertain time for everybody. We need to respond effectively to the kids while we are there. This is something that I support staff with a lot of the time. I am going to talk more about this, but we call it caregiver affect management. However, this has been even more particularly challenging than it usually is. Again, this has long been an important part of my job, but it is now a top priority.
The other thing that I wanted to touch on was navigating boundaries during a shared experience. This is one of the first times where we are all experiencing something at the same time. Part of my role as a liaison staff between the direct care staff and the administrative/clinical team is modeling the way that we can have appropriate conversations and connecting with individuals in our care while maintaining boundaries. We talk about this in our team meetings and think about the best way to share details and when that might be appropriate and beneficial for the kids and when that might not be.
Team Support
- Caregiver affect management
- Challenges for the team
- Changing staffing needs
We are all there to care for the kids together. And without all of us, we cannot do that. Caregiver affect management, as I had mentioned, is how we maintain ourselves to be in the best space for the kids. It is closely tied to our self-care and how we build resiliency for ourselves as individuals working in an acute trauma-informed environment. Now, throw a pandemic on top of that, and there are a lot of stressors. Sometimes, we are distracted and frustrated. How do we maintain our own energy and how do we use our own tools to make sure that that is not seeping out into our work? We want to make sure that we are our best space to provide the care that the kids need and be there for them at all times.
Some of the particular challenges for our team that came up during this. This is a unique situation. This is really the first time that in our group that we had to face the question of, are we willing to compromise one important group in our lives' safety for another? We had to be very mindful about following precautions and making sure that we were not bringing anything into the program. There were also some individuals, who based on their living situation and high-risk family members, needed to also think about the safety of what they might bring from the program home. This was a unique issue that we had to balance. In addition to that, this has simply just been a very challenging time. There are high needs, and the kids are there all the time. The level of support that is needed to maintain engagement, regulation, and smooth sailing in the house has been at max capacity. People are getting pretty burnt out, and there is a high amount of turnover. In fact, I am running a new hire orientation for the fourth time since August because we are having a really hard time making sure that everyone is in the best space to maintain their role in this team. It is becoming more challenging the longer this goes on. The team support piece has been really ramping up in importance as we have moved through this.
We also have specific changing staffing needs. In the past, when we had kids in school or away on the weekends, the ratio of staff to kids was different. Now, we need a fully staffed house all the time because we have a lot less movement in and out of the house. Kids are able to go on passes again, but there are a lot of different restrictions. We also have had staff leave due to like at-risk family members. They felt that this was not the best time for them to be working in such a close contact type of job. We do not do any like personal care or anything with the kids, but a group home is crowded. While we do our best to maintain social distancing and be safe, at times, kids are in one space for hands-on intervention. This may be needed if there is an imminent risk situation.
- What can an OT do?
- Promote resiliency with access to tools and resources
- Psychological First Aid
For the team support, what can OT do? Again, this is something that I do most of the time, it has ramped up in importance over the past couple of months. This is a picture of my staff support area at one of my programs in Figure 6.

Figure 6. Team support items.
I like to keep an area stocked with snacks, drinks, and practical items that might be needed. These are things like lotion, gum, cough drops, hair ties, deodorant, lens wipes, et cetera. We try to keep these items stocked every week. In addition to the concrete tools, I also regularly provide resources like podcasts, articles, online supports, or any type of event that might be happening. I like to promote that resiliency by providing the tools for them.
This is tied to the principles of psychological first aid (PFA). We use these concepts at times as often we are dealing with programmatic challenges that are pretty acute, whether that is a crisis situation or a restraint situation. We use the principles of PFA to help manage those very stressful times. PFA concepts include being available to provide support, providing comfort and stabilization, listening, finding out what people need, connecting people with resources, and providing information on how to manage emotions. All of these principles are interwoven in a way that team members need at the time to promote resiliency and prevent burnout. These things can help people feel connected and supported so that we can increase our ability to stay together as a team.
Another thing that I have done is to help cover shifts on the floor. Before this year, I covered only about two shifts in my whole time at JRI, and now I probably cover at least one shift a week. We need staff and our people need a break. Someone cannot stay for three shifts at a time. We need to make sure that the floor is covered with someone who is in the right space and energized to be with the kids. This is something that has taken more of a front seat to other things. This is also an opportunity to be a leader and to model that engagement and regulation out on the floor to help tie all of our different departmental teams together.
Additionally, for one of my programs, in the early months, I papered the staff office with the memes. For this specific team, this provided a little humor break. Some of us cope that way, and I knew that this particular team would appreciate it.
- What can an OT do?
- Use meaningful occupations & craft skills to show appreciation!
The last thing I wanted to just talk about was using my own personal skills and meaningful occupations as a person through my OT role. Something that I like to do is craft. I do this with the kids all the time, and my program directors are aware of that. I was able to concretely help the team by providing things that we needed such as the masks as shown in Figure 7.

Figure 7. Examples of crafts made for the staff.
These things helped our team feel appreciated. We can use our own skills to support our team in the best way possible and what they need at that time. There was a time several weeks where literally all I was doing was either working shifts on the floor or sewing masks, but that is what was needed.
Thanks for your time. Now, I can take some questions.
Questions and Answers
Can you elaborate more on DMDD?
Yes, that is a disruptive mood dysregulation disorder. This is when we see different patterns of behaviors of more explosive dysregulation in response to things that happen in the environment and throughout the kid's day.
Who do you lean on?
I do get programmatic supervision, and I work closely with our administrative team. We keep the ship running together and then support each other. There is an official supervision hierarchy, but we tend to co-supervise each other to provide that resiliency and support that we need. That is the culture of our program that we have developed from working together for so long.
Are all the kids the same gender? I'm thinking that would impact activities.
One site is female-identifying clients and the other is male-identifying clients. This does change the flavor of some of my activities, but you would be surprised at what they like to do. I do tend to reuse activities between sites pretty frequently. For the most part, they like a lot of the same things. The boys' program tends to prefer competition and where they can earn prizes and the girls are more crafty. They all like to bake.
How do you address the spiritual needs of the kids during the pandemic?
The kids that express interest in that domain typically have an identified community whether it is through their family or a previous program, and then we connect them through Zoom to their church's activities. I think we have a child at each of my programs right now that we have set up on a Zoom every weekend to be able to participate in their identified community.
Who pays for the supplies? Are these out of pocket for the group home? Do you pay for them? How does that work?
I have a monthly budget and a credit card for the program. I am responsible for managing the budget. I can purchase pretty much whatever I want for different activities.
What is the typical timeframe that a client stays within the program or group home?
It varies, but I would say the average right now is between a year to a year and a half.
I commend you for you shining a positive light on the ways, OT can be valuable in the community. Bravo to your creativity and therapeutic use of self. What are some of the regulation tools that you mentioned?
We use regulation tools at many levels in the program. The kids can have their own, or we have big spaces in the houses. In the bigger sensory room spaces, we have things that provide proprioceptive input and have different texture tiles on the walls. We have tons of fidgets. I go through fidgets like nobody's business. There are different lighting options, fiber optic lights, push lights on the walls, and bean bag chairs. The boys like the video game rocker chairs too. We use weighted tools like blankets, pillows, and stuffed animals. We also use different activity guides. I like yoga poses, stretches, and different body breaks. We also like to use aromatherapy and different scents. We use scent sticks, rollers, and diffuser jewelry. We use pretty much anything that I can find.
How old are the kids in general?
Their age range is from 12 to 20.
Before and after restrictions, how involved are the parents and family members?
This varies by family, and this is not up to us. The Department of Children and Families team decides the amount and type of contact that is allowed between the family members. Typically, we have kids who can talk to their parents on the phone. Our most common visitation schedule is that they go on day passes and maybe like one overnight. Some families take their kids for longer like all of Christmas break. Then, we have some on the other end of the spectrum who can only have supervised monthly visits at the DCF office. These two ends of the spectrum are rare. We usually have more of that in the middle level where they have their visits, but it is monitored. We do pass sheets and do check-ins. We provide support to help those passes be successful.
Where do the clients generally discharged to when they are done with the program? Are they integrated back into their family home or independently out in the community? Probably a variety of that I would assume.
All of the above. It depends on the kid and their family. What placement this is for them. If this is their first time out of the home, they are more likely to go back home. If they have been removed several times and are getting a little older, they are more likely to be on the independent living track. Some of our kids are able to maintain relationships with their parents but are not a good fit to live together. In these cases, they would move to the independent living track. Typically, our goal is to reunite the families as often as we can, but sometimes that is not the best option. Again, that is not up to us.
How many OTs are on staff?
Just me.
Have you had any students come?
Yes, I have had several Level II students. It is very helpful. It is very good to have a fresh perspective. I cover two programs and then the two other programs have an OT as well. I supervise her, and we work together to coordinate the OT services over the four programs.
How is the documentation or billing working in this setting?
Our kids are on a day rate. OT is included in the day rate of the services that are provided so I do not have to actually bill for my services individually. I do document individual progress and group notes for all of my sessions. I also do an initial evaluation for each child, and nd then after that, every quarter their treatment plan is updated by their clinician, and I also write an update for that. A
Are there any OTAs helping?
No. I have been advocating for that for quite some time.
Are there conflicts that happen between the kids due to their large age range? That seems like a significant difference in emotional, mental, and physical developmental abilities.
We have more challenges between the kids of a similar age and the ones who are a little bit further apart. They tend to sort of fall into a sibling-like pattern. That has its strengths and weaknesses. We have conflicts and incidents but for the most part, we are able to keep our relationships at a pretty good level.
Do you have previous participants come back to the program?
We have had that happen at both of my programs. We have had kids either go home or move to a different program, and then have to come back later depending on different circumstances. Sometimes it does not work out at home, or the supports that were put in place were not adequate. Other times it may be that a child went to a higher level of care because they needed a little more support and then they came back to us when they were ready to move back down. It can go either way.
How you got involved in this? This is just such a different setting.
I love it and am so glad I found it. I was looking for a pediatric mental health setting. The timing was really ideal because in Massachusetts, in 2014, there was legislation that was passed called Caring Together that called for the integration of OT into residential programs. I graduated in 2014 so the timing was ideal. After I completed my fieldwork at a recovery program for adults with serious and persistent mental illness, I decided I wanted to go down in age a little bit. I was just lucky enough to find that opening at the time.
What is the biggest challenge?
The biggest challenge is being split between two programs. I want to give all of my time and energy to both of them and I cannot. Finding the balance is the most difficult part. However, there are a lot of good things about working at two programs as well. I get to work with so many great kids and people and see things from two different perspectives.
References
Available in the handout.
Citation
Stumper, J. (2020). OT's mental health response to the COVID pandemic: Adolescents in group homes. OccupationalTherapy.com, Article 5372. Retrieved from http://OccupationalTherapy.com
